Guest Case Study by Dr. Ilana Gurevich
Patient info:
- Emily, 39 yo female
- Diagnosis: – Crohn’s disease of the small and large intestine.
- Chief complaint
- Diarrhea daily – 4-8 BM/D Bristol stool chart 6-7
- Severe anemia
- Needing iron infusions every six months starting in 2010
- Amenorrhea X 7 years
- Osteoporosis
- Edema in the ankles
- Low weight and unable to gain weight
- Fatigue
Emily presents to the clinic as a frail and emaciated female. She is slow to walk and in obvious physical pain. Emily is pale in complexion, very thin with a distended abdomen. On the first visit, Emily informs me that at age 19, she entered the ED for acute abdominal pain, and they rushed her into surgery. At that point, they removed her appendix and resected 4 feet of small bowel due to an obstruction of the intestine caused by Crohn’s disease.
From that point on, she was significantly underweight with a BMI of 16. She was unable to gain weight, and she had been dealing with chronic anemia needed either a blood transfusion or a blood infusion every six months. She had chronic diarrhea and pain. In the last year, she has further deteriorated and had edema in her legs that were so significant she had to wear compression stockings daily to maintain the swelling. She was also so underweight she had been amenorrhoeic for 7+ years and due to this has osteoporosis.
Emily maintained a strict Gut And Psychology Syndrome (GAPS) elimination diet in which she never altered. She also took many supplements which did not seem to make any difference. Emily refused any pharmaceutical medications to manage her disease due to experiencing side effects in the past and fear of continued side effects in the future.
Initial impression
Emily was a very sick and medically fragile case. She had no control over her disease at all. All of the dietary and supplement interventions were not working, and there was severe inflammation and malabsorption secondary to her Crohn’s disease. The cachexia, as well as the edematous ankles and the chronic anemia, were all clues to confirm that she was suffering from significant inflammation.
Tests ordered
- GI Health Panel
- CBC
- Fecal Calprotectin
Testing ordered, rational and results reported
- GI Health Panel – Diagnostechs
- At this point in my treatment of IBD, I used to use this test quite often. At the time, it was the best option for screening both pathologic and functional issues in the GI. I, however, now rarely use this test. Today I am much more likely to use DNA PCR testing since it is more sensitive for parasitology then an on the O&P and culture.
- Dr. R’s note: I agree with Ilana here
- Findings
- Found heavy gram-negative and no gram-positive flora
- Found a secretory IgA immune response to Ameba, Trichinella, Tapeworm
- No way of telling if this was an acute or chronic exposure
- Perceived food sensitivities to milk, soy, and egg
- Complete blood work panel
- The patient has a long history of anemia and needing iron transfusions and infusions. Continuing to be vigilant with monitoring her CBC was not only vital for her maintaining to live, but also a great way to follow her disease. As the CBC improves and can hold improvement, you know that the patient is coming into and maintaining a remission
- Findings:
- At this point in my treatment of IBD, I used to use this test quite often. At the time, it was the best option for screening both pathologic and functional issues in the GI. I, however, now rarely use this test. Today I am much more likely to use DNA PCR testing since it is more sensitive for parasitology then an on the O&P and culture.
| Lab test | Result |
| HEMOGLOBIN | 9.3 L |
| HEMATOCRIT | 31.2 L |
| MCV | 95 |
| MCHC | 29.9 L |
| PLATELET COUNT | 428 H |
| WHITE CELL COUNT | 4.3 |
| RED CELL COUNT | 3.29 L |
| RDW | 12.2 |
| Ferritin | 5.4 L |
| % Saturation | 4.7 L |
- Fecal calprotectin
- This is one of the most sensitive ways of monitoring large bowel IBD. It has been clinically found to be 92-98% predictive of flare and very close to a colonoscopy but much less invasive
- 1042 H
- Recommendations based on these findings and clinical thinking
- Maintain the hardcore GAPS diet
- The patient was very attached to this diet and felt that it was the way for her to heal. Because of this, we decided to continue with this diet.
- Hydrolyzed white fish protein
- This is a product that is anti-inflammatory and very bioavailable to the enterocytes of the GI. I use it clinically similar to how a gastro would use a steroid, in very high doses when patients are acute.
- A turmeric-based anti-inflammatory powder
- This has very anti-inflammatory actions on the intestinal cells of the large and small intestine and is well studied for IBD.
- High dose herbal antimicrobials
- The patient’s unbalanced large bowel microbiome with a high gram-negative flora warranted using herbal anti-microbials at higher amounts.
- Also, the patient had Secretory IgA responses to multiple protozoa. However, since there is no way of knowing if these protozoa were currently present or were present in the past pharmaceutical management was not an option. The use of herbs had a more significant indication.
- Digestive enzymes
- To help support the stomach and pancreas in healthy digestive function
- Start a GAPS legal probiotic
- Due to the large bowel microbiome dysbiosis adding a probiotic was warranted in this case
- Iron
- Rx 72 mg every other day with cofactors for absorption
- Desiccated liver pills
- The patient was already using this, and I told her to stay on them as a way of altering iron absorption
- Methylcobalamin
- 1000 mcg daily
- Although the patient had very significant iron deficiency anemia, her MCV was still trending on the higher edge of normal. This informed that she is suffering from macrocytic anemia as well as the iron-deficiency anemia
- Vitamin D
- 5000 iu daily
- This was warranted for the anti-inflammatory effects it possesses
- Maintain the hardcore GAPS diet
- Improved
- Bowel movements were a lot less painful, and she also had less bloating and discomfort.
- Her BMs were not as regular, but when she has them, they were initially more formed. That formation lasted around 2-3 weeks following treatment initiation.
- She has also evened out with weight and was no longer losing any weight. She weighed herself daily, but it was staying steady. However, even though she was on a high-calorie diet, she was not able to gain much weight.
- Worse
- Her energy was lower overall. She needed naps daily and was very tired in the early evening.
- After the initial improvement in bowels, they then started to deteriorate again and become loose again. She didn’t have nearly as severe of pain as in the past, but the pain was still present.
- Impression
- Even on such an extensive treatment plan, the patient was still not improving as quickly as I would have liked. She always had chronic diarrhea, chronic pain, was still unable to gain weight and was also still anemic. It was apparent to me that I was putting too much attention on using anti-inflammatory herbs and not enough attention the addressing the pathologic microbiome. Because of this, we decided to run a SIBO breath test at this point to see if this was an underlying issue.
- SIBO Breath test
- Positive H2 at 40 min with an increase in 31 ppm
- Positive CH4 at 40 min with a finding of 13 ppm
- CBC
| HEMOGLOBIN | 5.6 L |
| HEMATOCRIT | 23.2 L |
| MCV | 61 L |
| MCHC | 24.2 L |
| PLATELET COUNT | 588 H |
| WHITE CELL COUNT | 6.5 |
| RED CELL COUNT | 3.78 L |
| RDW | 18.6 H |
| Ferritin | <1.5 L |
- Treatment plan and rationale
- Rifaxamin – 550 mg three times a day for 14 days
- Neomycin – 500 mg twice per day for ten days
- This was the standard antibiotic treatment of SIBO for the treatment of both hydrogen and methane.
- Hydrolyzed guar gum – 5 grams split during the day when taking the rifaxamin. 2 grams w AM dose, 2 grams with lunch dose and 1 gram at bedtime
- Since the patient was on a GAPS diet, she didn’t have a lot of carbohydrates in her diet. The efficacy of SIBO antibiotics is based on bacterial and archeal carbohydrate metabolism, so the guar gum was in the treatment plan for that reason.
- Low dose naltrexone – 1 mg daily at bedtime
- This was placed mainly for its effects on mitigating the autoimmune response.
Subjective assessment
- Improved
- The patient noticed a significant improvement in her symptoms. Her diarrhea resolved, and her pain significantly improved. She was able to gain weight, and her blood values improved and were able to maintain. Her energy grew as well, and she was able to walk and was much more mobile. Her edema also improved.
- Worsening
- The only symptom that was still present was bloating. She had always suffered from bloating, but because of all the other issues she had, it wasn’t a primary complaint. Now that she was feeling so much better this then became a primary complaint, and she wanted to address it more aggressively.
- Impression
- We were now treating the underlying cause of her Crohn’s disease. The bacterial overgrowth of her small bowel was impacting her absorption of iron, B12, and her GI function. Addressing the Crohn’s with SIBO treatments, she entered remission for the 1st time in over a decade.
- Follow up CBC
| HEMOGLOBIN | 11.4 L |
| HEMATOCRIT | 36.6 |
| MCV | 101 H |
| MCHC | 31 L |
| PLATELET COUNT | 385 |
| WHITE CELL COUNT | 6.5 |
| RED CELL COUNT | 3.62 L |
| RDW | 11 L |
| Ferritin | 58.5 |
- Follow up SIBO breath test
- Negative H2
- Positive CH4 – 25 ppm at 20 min and continued to be elevated from there
- Treatment plan and rationale
- Allimax
- Take one pill three times a day
- Rotate weekly through
- Oregano essential oil blend
- Neem
- Essential oil blend
- And other forms of herbal antibiotics in there
- Stay on each for at least a week
- Add in NAC
- 1200 mg 2 times per day if you can tolerate it
- Increase the dose of LDN to 2.5 mg once a day at bedtime
- Start low dose erythromycin as a motility agent after the herbal antibiotic phase
- We decided to change off of antibiotics to herbs since they are better tolerated, heal the intestinal permeability of the IBD, and have more broad-spectrum results. Also, because she has no ileocecal valve, she will most likely always have SIBO. Because of this, we choose a continuous herbal antibiotic protocol since it should continue to address the SIBO, but it also heals the mucous membrane so it should be safe.
- Allimax
- Current update on the patient
- The patient is doing fantastic. She has not needed an infusion or transfusion since the last one that was performed on 1/14. She has been able to maintain her iron status since then. She is also at a very healthy weight with a BMI of 20.2 and has been since 2014. She has regular menses and no longer has edema in her legs. Addressing this patient SIBO was the key to putting her into a remission in which she still is currently.
Great case study here. As you can see there is much overlap in how Ilana and I think. Essentially this case needed immune/inflammatory support and antimicrobial therapy. Nothing particularly complicated, but it required an attentive clinician who can modify the plan over time. Elemental dieting or immunoglobulins here could have been used as similar agents to the fish protein and the LDN. Good news, we have options.
Nutrients. 2019 Aug 21;11(9). pii: E1968. doi: 10.3390/nu11091968.
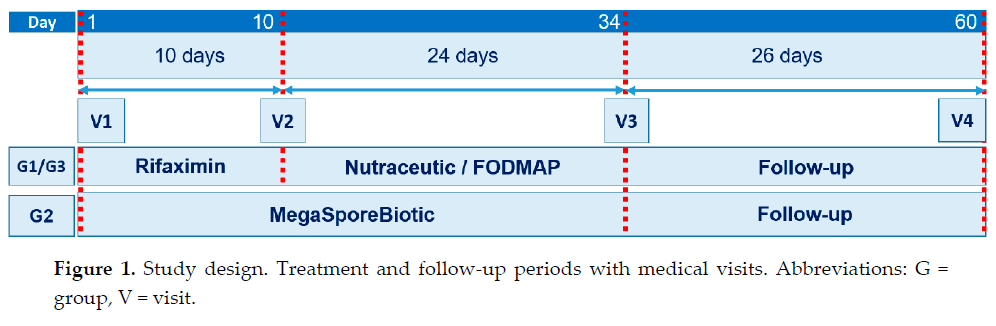
Study purpose
- Compare three treatments
- 10 days rifaximin followed by 20 days nutraceutical (prebiotics, probiotic & B vitamins) – G1
- 10 days rifaximin followed by 20 days low FODMAP diet – G3
- 30 days soil-based probiotic (MegaSpore) – G2
Intervention:
- See above and chart below
- Nutraceutical agent = Bifidobacterium longum W11, prebiotic as soluble fiber and B vitamins—B1, B2, B6, B12
- Nutraceutical agent = Bifidobacterium longum W11, prebiotic as soluble fiber and B vitamins—B1, B2, B6, B12
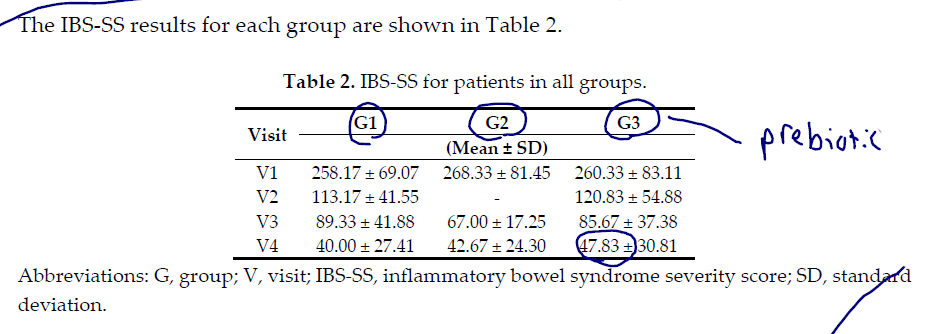
Main Results:
- Results were the same, 60 days after ALL treatments, for all groups. Either rifaximin + low FODMAP, rifaximin + nutraceutical or MegaSpore. This was timepoint V4 with measures IBS-SS (IBS severity survey), QOL score (IBS-QL), and rectal volume.
- At timepoint V3, using a soil-based probiotic yielded better results than rifaximin+low FODMAP or rifaximin+nutraceutical. Treatment impacts were all the same at timepoint V4 (60 days)
- Between groups (intergroup), significant difference were only observed at V3 (34 days). The results showed that treatment with Bacillus spores (G2) attenuated the IBS-SS score better than rifaximin plus the nutraceutical agent (G1) and similarly to rifaximin plus a low-FODMAP diet (G3)
- The results showed that there was no statistically significant differences between groups at timepoint V4 for IBS-SS or rectal volume but only for IBS-QOL.
Additional Results:
- na
Limitations:
- Small study. No placebo or control.
Authors Conclusion:
- “Overall, our study demonstrated that MegaSporeBiotic (a mix of spores from five Bacillus spp.) had a similar impact on severity score and all parameters of the rectal volume sensation test and a significantly better effect on QL compared with rifaximin plus nutraceutical agent or a low-FODMAP diet.”
Interesting Notes:
- na
Clinical Takeaways:
- Probiotics are highly effective for IBS.
- Probiotics have a better (number needed to treat than rifaximin; 8-9 versus 11 respectively), see my SIBO article for more.
- What to tell your patients:
- Probiotics are very helpful for IBS and for SIBO. There is a good chance you will not require antimicrobial therapy (herbal or antibiotic) after a thorough probiotic protocol.
Dr. Ruscio Comments
As I have been saying for quite some time, probiotics are quite helpful for IBS, as supported by dozens of clinical trials and a handful of meta-analyses. They are also helpful for SIBO. So it is no surprise to see how effective they are here.
I love the fact that we have another study showcasing the effects of probiotics on SIBO, especially when comparing to other treatments. It is also important not to get overly excited about this one study and overlook the wealth of research on the other two categorical types of probiotics. Maintain a birds-eye perspective on the probiotics research, all three categories are viable for IBS.
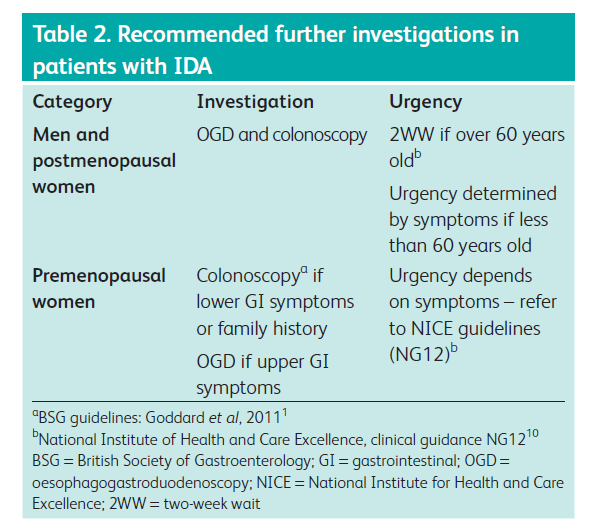
Clin Med (Lond). 2018 Jun;18(3):242-244. doi: 10.7861/clinmedicine.18-3-242.
Study Purpose
- Discuss causes and laboratory interpretation of iron anemia
Intervention:
- Review, non-systematic
Background Notes
- Anemia is hemoglobin (Hb) below the lower limit of normal, as defined by the laboratory performing the test.
- It is important to clarify the cause of anemia, as patients with iron deficiency anemia (IDA) deserve urgent investigation since 8–15% (if they are over 60 years old) of these patients will be diagnosed with gastrointestinal cancer.
- If there is no iron deficiency, investigative efforts can be directed elsewhere.
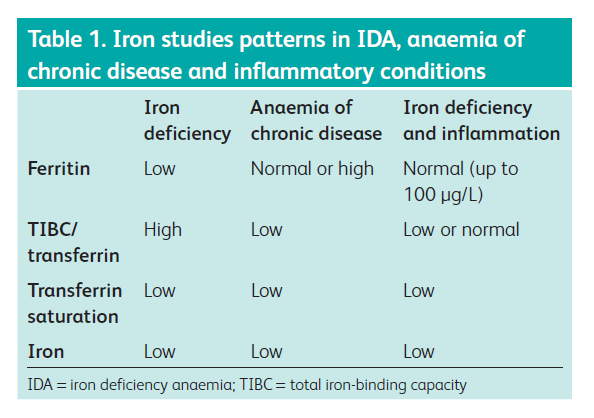
- The transferrin saturation is the amount of iron that is bound to transferrin, expressed as a percentage of the TIBC. In IDA, the ferritin, serum iron, and transferrin saturation are low, but the TIBC increases.
- As the body tries to compensate for low iron levels, this correlates positively with the TIBC.
- In contrast, in anemia of chronic disease (ACD), the ferritin is raised, owing to an increase in the iron regulator hepcidin.
- Studies have shown that hepcidin expression is upregulated when there is infection or inflammation, via inflammatory cytokines such as IL-6 (5). Hepcidin binds to ferroportin (the iron exporter on cells) which results in internalization and degradation of this transporter, which reduces iron release from cells. This failure of release of iron from the ferritin stores results in low iron, low transferrin saturation and low TIBC, with high ferritin (Table 1).
Lab Interpretation
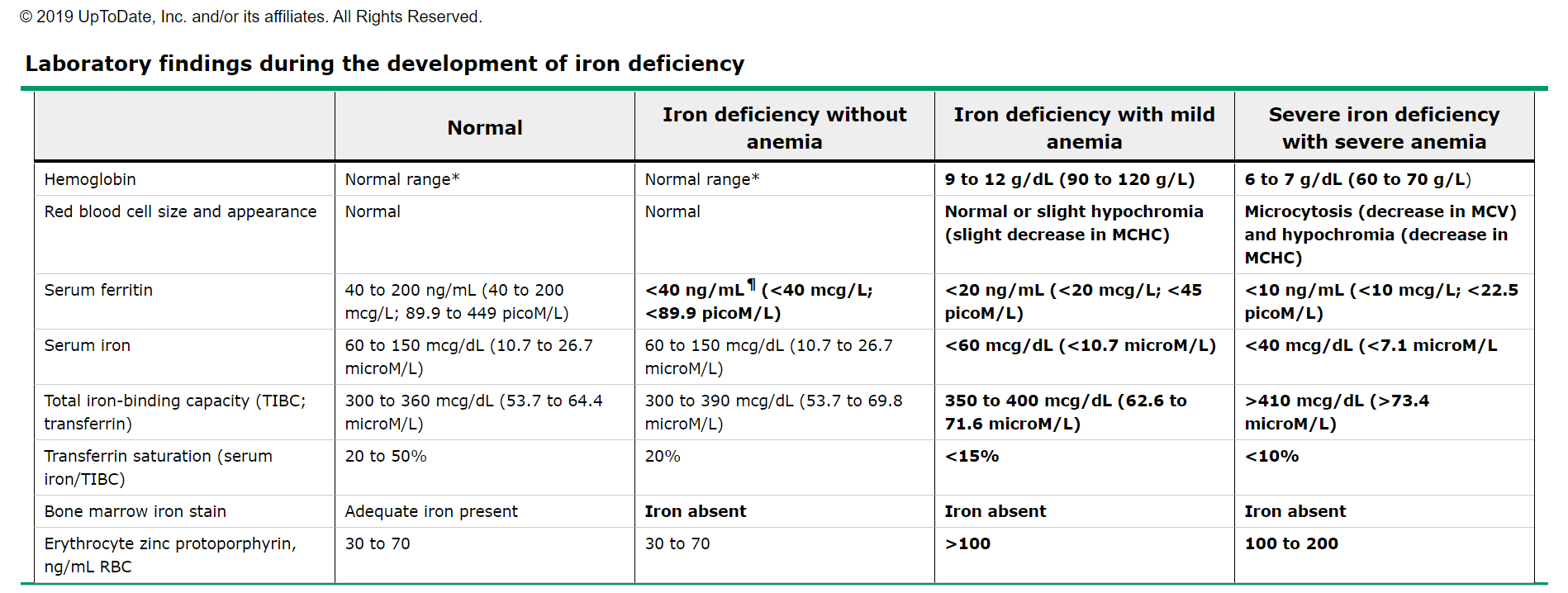
- Ferritin is the best indicator of iron deficiency and low ferritin alone is diagnostic of IDA. Inflammation can elevate ferritin.
- Iron is stored intracellularly as ferritin and in the presence of infection, malignancy or chronic inflammation, the ferritin rises as it is an acute-phase protein.
- Therefore, the diagnosis of IDA is challenging when there is coexisting inflammation, as the ferritin can be up to 100 μg/L (normal range 20–200 μg/L in our institution), even in the presence of iron deficiency. In this case, further tests can help clarify the diagnosis.
- Fantastic summary table
- If IDA and ACD coexist, ferritin of greater than 100 μg/L can reliably rule out iron deficiency.
- Any hemoglobin, in the presence of ferritin below the lower limit of normal, or below 100 μg/L in the presence of infection/inflammation, should be investigated as IDA.
- My question here is how do we define infection/inflammation? CRP, ESR, pylori, SIBO…? Attempting to have authors on the podcast to elaborate.
- MCV: If iron deficiency coexists with B12 or folate deficiency, the MCV can be high, normal or low.
- RDW:
- High in IDA, B12 deficiency and folate deficiency.
- Normal in ACD and hemoglobinopathies.
- UpToDate also provides the following table (as you can see, ferritin will shift before hemoglobin or serum iron).
Causes If Iron Deficiency Anemia (IDA)
- IDA can be caused by blood loss (gastrointestinal [GI] or other), or reduced absorption of iron.
- The commonest cause of IDA in menstruating women is menstrual blood loss.
- The most common cause in men and non-menstruating women is GI blood loss.
- Positive findings on a colonoscopy: malignancy, polyps, angiodysplasia or inflammatory bowel disease (IBD).
- Positive findings on a gastroscopy: ulcers, angiodysplasia and cancer macroscopically, and celiac disease or atrophic gastritis microscopically.
History Findings
- In patients with IDA, particular note should be taken in history to:
- previous or recent blood donation
- previous history of IDA
- adequate dietary intake
- overt blood loss
- family history of iron deficiency anemia
- family history of hemoglobinopathies
- NSAID use
- Investigations to consider in iron deficiency anemia
- Fecal occult blood
- The use of fecal occult blood testing (FOBt) in the investigation of IDA is recommended by the National Institute for Health and Care Excellence (NICE) as an alternative to endoscopic investigation in patients less than 60 years of age. However, in the view of the authors, this approach is inappropriate because the low sensitivity of FOBt makes it inadequate for this purpose and significant pathology will be missed.
Treatment
- Once investigations have been performed, underlying causes should be treated. If no cause is identified then an iron replacement strategy is appropriate.
- Iron replacement
- For example, ferrous sulfate or ferrous fumarate once or twice a day, is continued until the Hb normalizes, which may take up to 6–12 weeks depending on the degree of anemia.
- Subsequently, a further 3 months of oral iron should be taken to replenish the stores.
- The Hb should then be checked every 3 months for a year, then after a further year.
- If the Hb is not restored or if it falls within 1 year of replenishing the stores, persistent obscure bleeding is present and should be investigated.
- This strategy has been shown to be safe, provided that dietary deficiency is replaced, NSAIDs have been stopped and the Hb is being reliably monitored.
- For those with recurring anemia
- If there is persistent obscure bleeding as evidenced by a failure to restore or maintain the Hb with iron supplement treatment, as described above, a small bowel capsule endoscopy should be considered to identify small bowel pathologies such as Crohn’s disease, angiodysplasia or neoplasia. If this is normal, or the Hb continues to fall without an explanation, non-GI cancer should also be sought.
Clinical Takeaways:
- Ferritin may be the first indicator of iron anemia.
- It is important to delineate between anemia of iron deficiency versus chronic disease/inflammation.
- What to tell your patients:
- You can be iron deficient without full-blown anemia (low ferritin only).
- It is important for us to optimize gut health as the potential cause of the iron deficiency and/or anemia.
Dr. Ruscio Comments
The paper helps to validate the work by Soppi we have discussed prior, finding problems in women with ferritin below 100.
SYMPOSIUM REPORT: An Evidence-Based Approach to IBS and CIC: Applying New Advances to Daily Practice: A Review of an Adjunct Clinical Symposium of the American College of Gastroenterology Meeting October 16, 2016 • Las Vegas, Nevada.
Gastroenterol Hepatol (N Y). 2017 Feb;13(2 Suppl 1):1-16.
Study purpose
- The purpose of the “review was to evaluate the efficacy of therapies for IBS or CIC compared with placebo or no treatment in randomized controlled trials.”
Intervention:
- Review, non-systematic
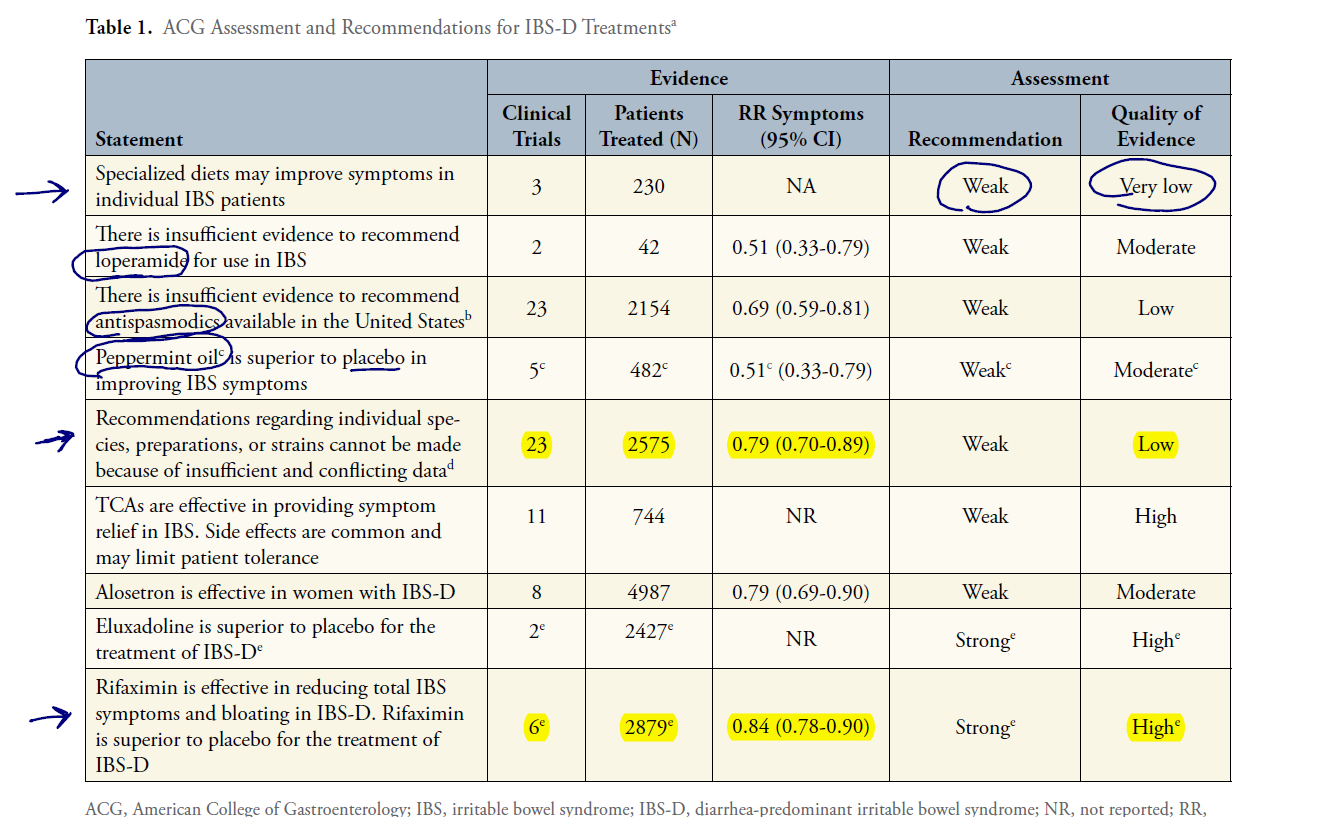
Main Results:
- IBS therapies
- “Evidence-based approaches to managing diarrhea-predominant IBS include dietary measures, such as a diet low in gluten and fermentable oligo-, di-, and mono-saccharides and polyols (FODMAPs); loperamide; antispasmodics; peppermint oil; probiotics; tricyclic antidepressants; alosetron; eluxadoline, and rifaximin.”
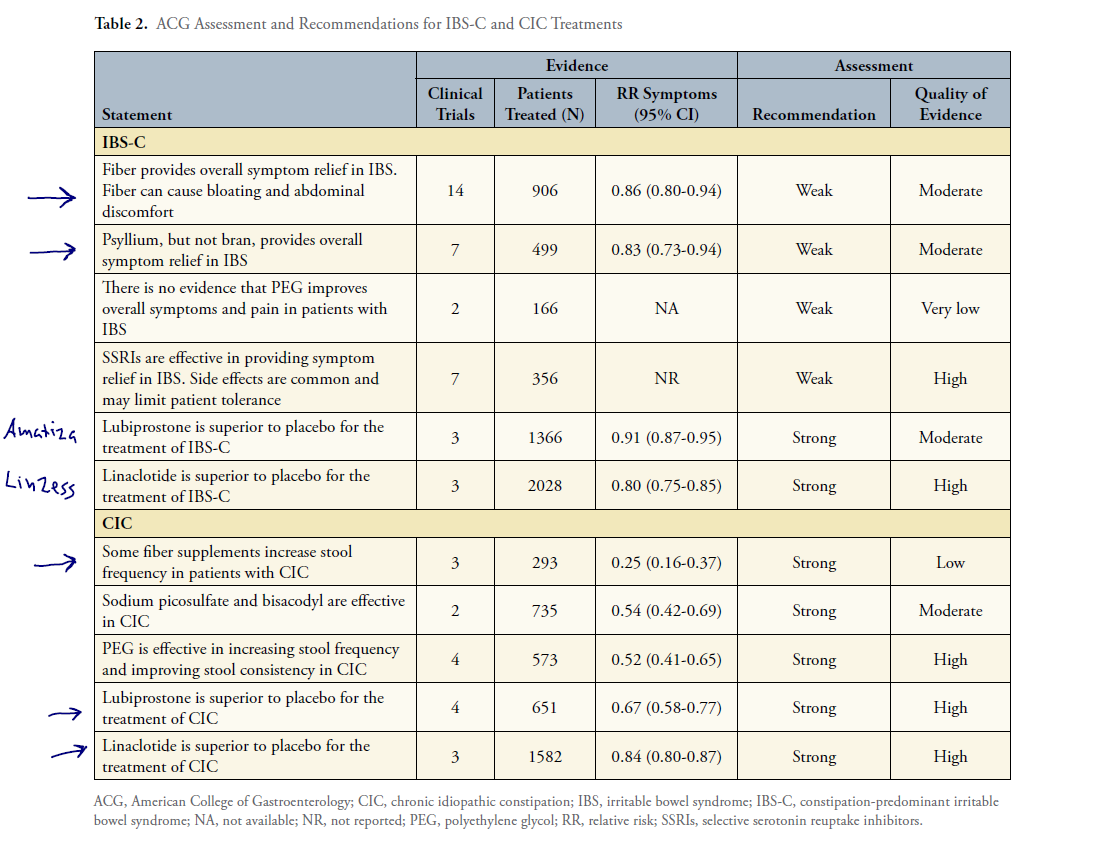
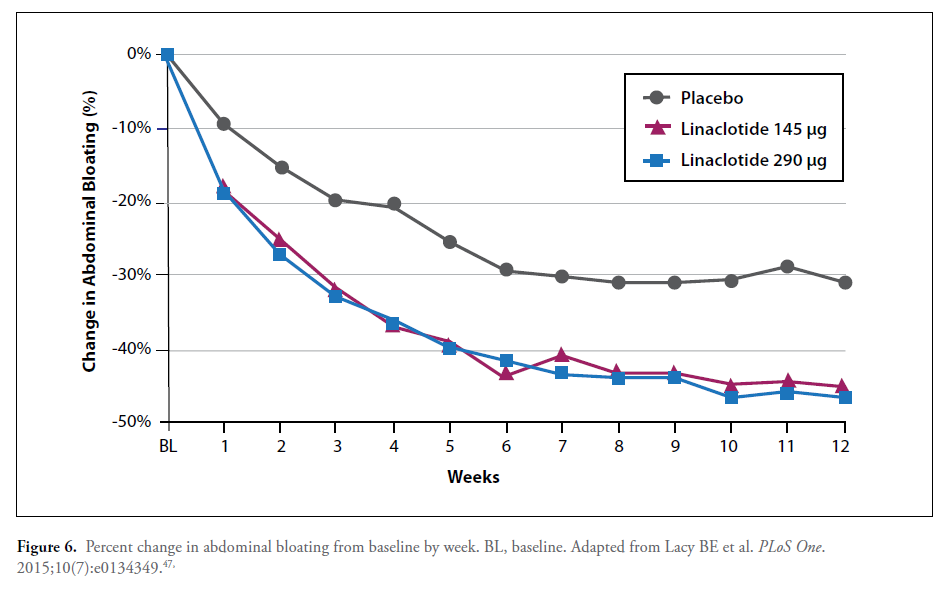
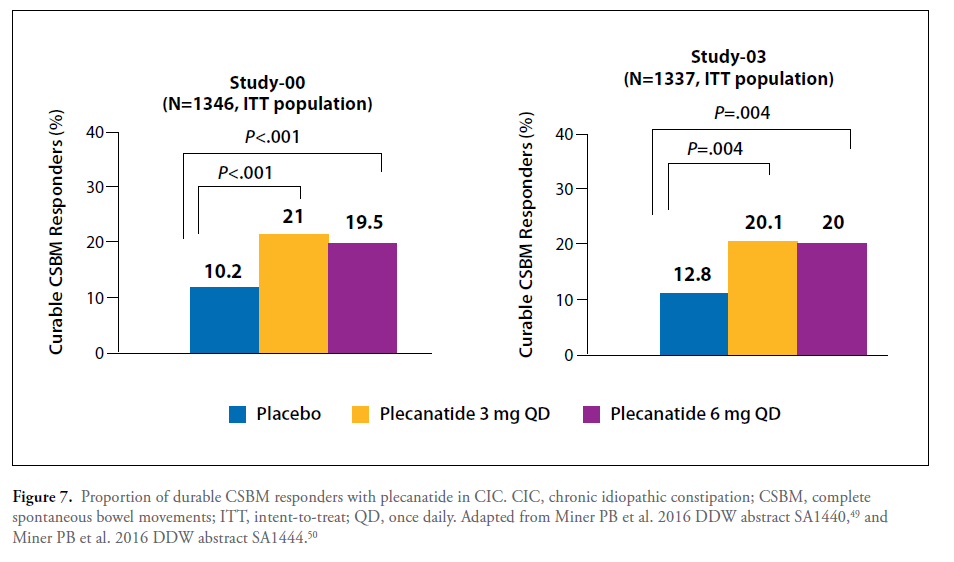
- Constipation therapies
- “Evidence-based approaches to managing constipation-predominant IBS and CIC include fiber, stimulant laxatives, polyethylene glycol, selective serotonin reuptake inhibitors, lubiprostone, and guanylate cyclase agonists.”
Additional Results:
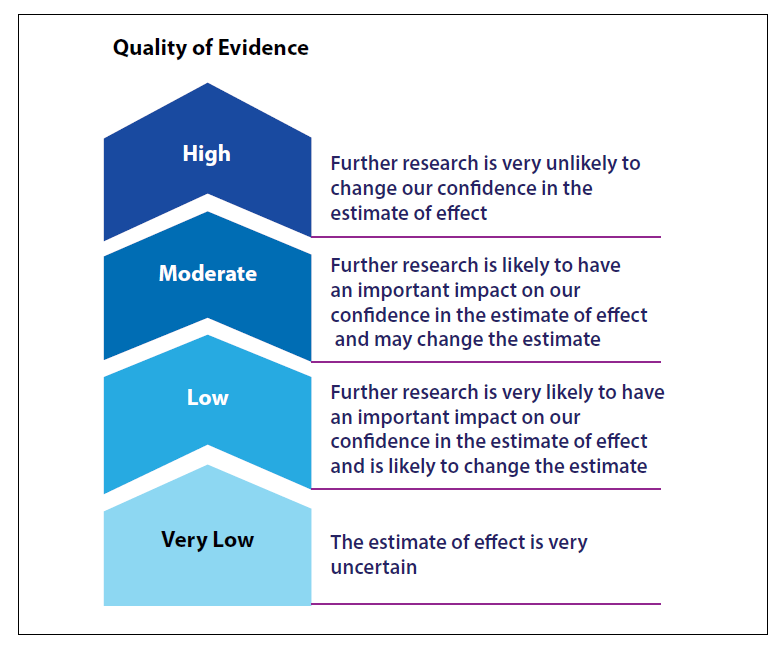
- Quality of evidence
- Interpreting Key Measures of Treatment Efficacy
- RR (Relative Risk): of 0.80 = 20% more patients achieving the desired result from treatment than from placebo.
- For example, an RR of 0.80 is interpreted as the probability of not achieving global symptom improvement being 20% compared with that without treatment. In other words, patients treated with the active therapy are 20% (100 × [1-RR]%) more likely to achieve symptom improvement compared with patients treated with placebo
- NNT (Number Needed to Treat): is the number of patients who need to receive treatment in order for one to see the desired response. NNT helps to compare different treatments, but not to measure effect relative to placebo.
- Although NNT values are helpful when comparing 2 active therapies, they are not as useful when comparing active treatment against placebo.
- To the contrary, comparing the NNT of treatments that have been evaluated in separate placebo-controlled RCTs can be misleading, as the NNT will vary based on differences in study duration, patient population, endpoint, and other key aspects of the study design.
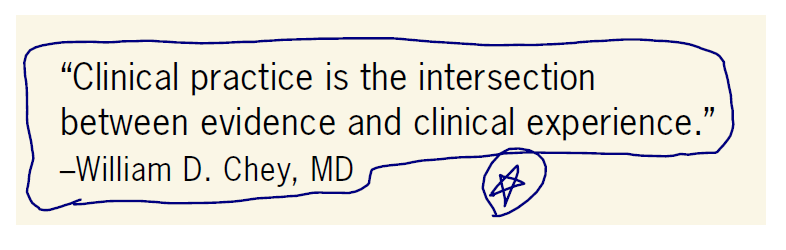
- Be evidence-based, but not ‘evidence-limited’. Glad to see this note that evidence must be combined with clinical experience, or as I say be evidence-based but not evidence-limited.
- In order to critically appraise the evidence, clinicians must understand study limitations, recognize bias, extract information, and reach appropriate conclusions (14). However, it is important to recognize that the application of evidence-based medicine does not devalue clinical experience. To the contrary, successful evidence-based practice requires that clinicians apply the scientific findings to their clinical decision-making process for individual patients (11).
- The magnitude of benefit, risk of side effects, patient preferences, and cost for individual patients are all key aspects of clinical decision-making. However, clinical experience guides the clinician’s application of data to individual patients. The treatment nuances that clinicians learn over time is invaluable when applying evidence, and is also crucial when useful evidence is absent. Lack of evidence should not be construed as lack of efficacy.
- And very good to see this applied to probiotic research….
- “For example, the ACG monograph concluded that the quality of evidence for the use of probiotics in IBS is low and that the strength of the recommendation regarding their use is weak (6). Rather than concluding that all probiotics are ineffective, this indicates that the current evidence is insufficient to identify specific probiotics that are effective. In the future, well-designed research trials may identify effective probiotics or provide more definitive evidence that probiotics are not effective. Until those studies are performed, physicians should use their own clinical experience to decide when to use a probiotic and which probiotic to select.
- RR (Relative Risk): of 0.80 = 20% more patients achieving the desired result from treatment than from placebo.
IBS Treatments Summary
- The table below provides an evidence summary of available treatments. See my notes below.
- Rifaximin & Probiotics
- Rifaximin has a similar NNT (Number Needed to Treat) as probiotics AND a similar relative risk reduction. The quality of evidence differs, however. This is mostly due to the individual study sizes (N) for probiotics being smaller, and different probiotic formulas being used. In my opinion, the lather indicates that different probiotics formulas can all provide benefit.
- When we weight the cost and potential invasiveness of rifaximin versus probiotics, it seems tenable to perform a trial on probiotics first.
- “… the large number of preparations included in these studies makes it very difficult to evaluate the efficacy of individual species and strains of probiotics used in IBS.”
- “As mentioned previously, these conclusions do not indicate that probiotics are not effective in individual patients, but rather that the evidence supporting their efficacy is weak.”
- It is important to note that rifaximin does display good safety data, so we should also be careful not to vilify rifaximin due to it being an antibiotic.
- Rifaximin is well-tolerated, with a safety profile similar to that of placebo. Further, despite concerns regarding the long-term or repeated use of an antibiotic, rifaximin has demonstrated an excellent safety pro-file throughout the time periods that it has been evaluated (6).
- Dietary trials
- “Of 12 RCTs that evaluated dietary intervention in IBS, only 3 of these trials met the inclusion criteria and were evaluated by the ACG review.”
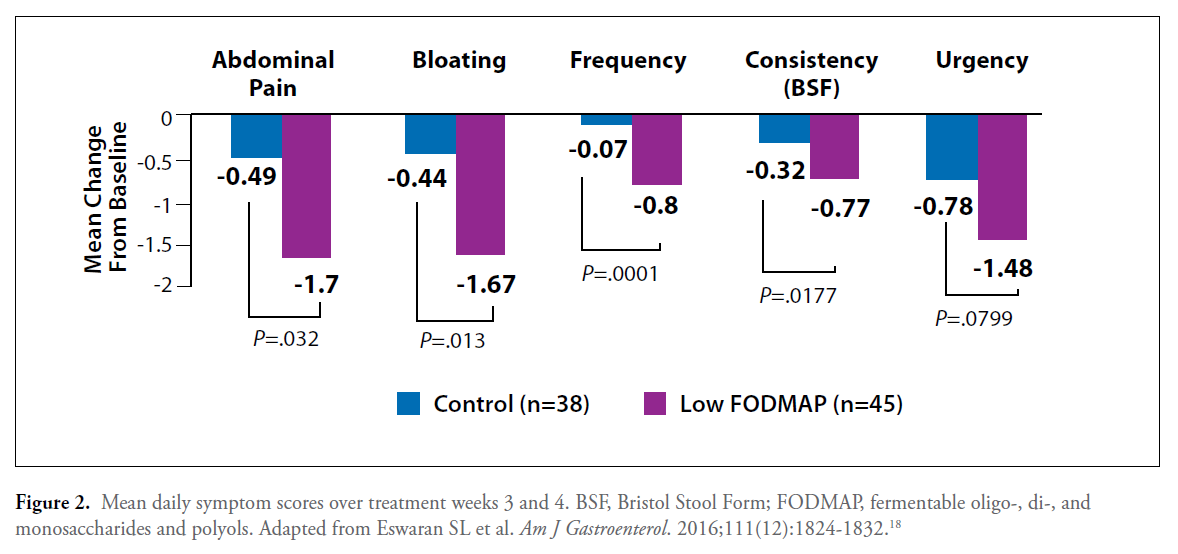
- An RCT was recently published (see results table below), validating that the low FODMAP diet can work better than standard dietary recommendations (control).
- Since the ACG review was conducted, however, results of the first RCT of the low FODMAP diet in patients with diarrhea-predominant IBS (IBS-D) in the United States have been published (18). In this single-center study, 92 patients were randomized to either a low FODMAP diet or a diet based on modified National Institute for Health and Care Excellence (mNICE) guidelines for 4 weeks. From 40% to 50% of patients reported adequate relief of their IBS-D symptoms with either diet, but the low FODMAP diet was significantly more effective in improving individual symptoms, particularly pain and bloating (Figure 2).
- Since the ACG review was conducted, however, results of the first RCT of the low FODMAP diet in patients with diarrhea-predominant IBS (IBS-D) in the United States have been published (18). In this single-center study, 92 patients were randomized to either a low FODMAP diet or a diet based on modified National Institute for Health and Care Excellence (mNICE) guidelines for 4 weeks. From 40% to 50% of patients reported adequate relief of their IBS-D symptoms with either diet, but the low FODMAP diet was significantly more effective in improving individual symptoms, particularly pain and bloating (Figure 2).
- Peppermint oil
- The research looks promising, but the lower relative risk reduction is exactly what I experienced in clinical practice with peppermint…. 50% versus 80% chance of improvement when comparing peppermint to probiotics. So, after clinical experimentation, I now use probiotics over peppermint oil but am still open to peppermint.
- Based on data from 5 RCTs involving 482 patients, the ACG review calculated an RR of 0.51, reflecting a 50% probability of this agent improving IBS symptoms (6).
- Although classified as an antispasmodic based on its calcium channel–blocking properties, peppermint oil and its active ingredient, L-menthol, have a number of other effects that may be relevant to IBS, including normalizing orocecal transit time, κ-opioid antagonism, and 5-HT3 antagonism (5, 19). In contrast to conventional antispasmodics, a relatively strong body of evidence worldwide supports the use of peppermint oil.
- The research looks promising, but the lower relative risk reduction is exactly what I experienced in clinical practice with peppermint…. 50% versus 80% chance of improvement when comparing peppermint to probiotics. So, after clinical experimentation, I now use probiotics over peppermint oil but am still open to peppermint.
- Fiber
- Fiber and prebiotics appear a double-edged sword, they can help but that can also flare and so should be used cautiously
- Soluble fiber appears better than insoluble fiber
- “the benefit is limited to soluble fibers, most notably psyllium (6, 32) In the largest study to date, 275 adults with IBS were randomized to soluble fiber (psyllium), insoluble fiber (bran), or placebo once daily for 12 weeks (33).
- Psyllium was found to be significantly more effective than placebo in providing adequate symptom relief in the first 2 months of therapy, whereas bran was not more effective than placebo (33). Importantly, early drop-out was considerable in the bran group, most commonly owing to exacerbation of IBS.
- Constipation Treatment Summary
- The main finding here I’d like to point out is we have evidence and similar effectiveness for natural therapies. However, the main limitation is the quality of the evidence (likely mostly due to smaller studies).
- Also, higher doses of stimulants or laxatives do not appear to offer any additional benefit.
Limitations:
- The lead author has worked as a consultant for a company that makes peppermint oil and for another company that manufactures rifaximin.
Authors Conclusion:
- The successful application of evidence-based medicine requires that clinicians integrate their understanding of the evidence with their own clinical experience in order to balance the magnitude of benefit and risk for individual patients.
Clinical Takeaways:
- Many natural treatments have an acceptable evidence-base justifying their use. The evidence is usually not as ‘strong’ as pharmaceuticals which is often due to a lack of larger trials than it is a finding of inferiority.
- Clinical practice requires the application of evidence-based therapies, in addition to clinical experience and personalization.
- What to tell your patients:
- Probiotics can be used before we consider rifaximin.
- We can perform a cautious trial on fiber for your constipation.
Dr. Ruscio Comments
The above provides a good summary of navigating the available IBS and constipation therapies.
Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial.
https://www.ncbi.nlm.nih.gov/pubmed/29246725
- “daily oral Theracurmin may lead to improved memory and attention in non-demented adults. The FDDNP-PET findings suggest that symptom benefits are associated with decreases in amyloid and tau accumulation in brain regions modulating mood and memory”
- See expanded summary here, but essentially Theracurmin improved memory at a dose of 2 caps per day.
Gluten-induced symptoms in diarrhea-predominant irritable bowel syndrome are associated with increased myosin light chain kinase activity and claudin-15 expression.
https://www.ncbi.nlm.nih.gov/pubmed/27869798
- Those who experience a worsening of their IBS after eating gluten were shown to have leaky gut as part of the underlying cause.