Hypothyroid Case Did NOT Respond to Levothyroxine, Did NOT Require Combination Therapy, GI Support Resolved Symptoms.
Patient Info:
- Monica, 36y/o, Female
- Previous Dx:
- Hypothyroid
- Rx:
- Levothyroxine
- Chief Complaints:
- Fatigue, 8-Constant
- Bloating, 8-Constant
- Weight Gain, 10-Constant
- Constipation, 10-Constant
- Dry Skin, 6-Intermittent
- Feeling Cold, 6-Intermittent
- Other Symptoms:
- PMS, digestion, pelvic pain, depression, brain fog
- Allostatic load – severe (cravings, fatigue, stimulants)
Initial Impression:
- Monica is a 36y/o female, on a Keto diet, with a good lifestyle, demeanor, and outlook.
- Dx/Rx:
- Dx: Hypothyroid
- Rx: Levothyroxine
- Previous Testing:
- n/a
- Onset:
- Constipation lifelong. Hypothyroid started postpartum, symptoms not responsive to Levothyroxine.
- Family History:
- Diabetes
- High Blood Pressure
- High Cholesterol
- Prior Treatments:
- Helpful: Miralax, natural thyroid support, Keto
- Not helpful: Levothyroxine
- Notes/DDX:
- Could have GI dysbiosis, need bowel support, female hormone support, iron, and/or thyroid med change
- Prognosis:
- Good to excellent
- Previous Diets:
- Keto, Atkins
Testing:
- Tests Ordered
- CMP, CBC w/ differential, Iron panel, lipid panel, vit D
- TSH, fT4 Dialysis/LC-MS, fT3 (immunoassay)
- TPO and TG antibodies
- Optional
- Aerodiagnostics Lactulose SIBO breath test
- Doctors Data Para 3x w/ H. Pylori stool test
- Rationale
- Basic workup for GI. Checking for thyroid AI.
- Performing most-sensitive thyroid assay to determine if her fT4 or fT3 are out of range thus requiring dose adjustment.
Recommendations:
- Diet:
- Start on Paleo low FODMAP diet.
- Can continue to eat one meal/day most days, but try to eat 2 meals 2-3 days/week.
- Work to cut coffee consumption in half.
- NRT: Multivitamin, EPA/DHA, Vitamin D/K
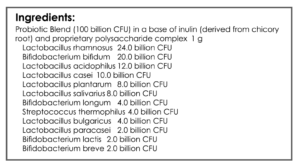
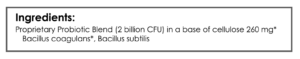
- GI: Lacto-Bifido blend probiotic, soil-based probiotic, Dietary Fiber
- Note: Be on diet for 2 weeks before adding in supplements, but continue diet until follow up. Then be on the supplements for 3 weeks before following up. Make a note of the change you noticed from diet versus supplements.
- Follow up: 6 weeks
Subjective Assessment:
- Paleo low FODMAP – very helpful for bloating, fatigue, regularity
- Reduced Coffee – helpful
- Multi, EPA/DHA, D/K – helpful
- Lacto-Biff, Soil-Based, Fiber – helpful – no longer needs Miralax!
- Improved:
- Fatigue, bloating, constipation, skin, hormone issues, clothes fit better
- Same:
- Weight
- Worse:
- n/a
Lab Interpretation:
- Metabolic Panel: Alkaline Phosphatase 35-L
- Lipid Panel: Cholesterol 217-H, LDL 135-H
- Iron Panel: TIBC 241-L Ferritin 88
- Vitamin D: 42.9-WNL
- Thyroid Autoantibodies (TPO + TGA): TPO Ab 135-H
- Stool Test + SIBO Breath Test: Not performed
Impression:
- Today has greatly improved, every chief complaint responded to treatment. Paleo low FODMAP, less coffee, Multi, D, fish oil, probiotics, and fiber – all very helpful. Labs show ferritin 88, low normal fT4/T3 LC-MS. Will maintain current plan + slight food reintroduction, then follow and first wean off supplements, then formal reintroduction.
Recommendations:
Starting:
- Continue the current plan and keep up the good work!
- Can cautiously trial some off-plan foods and see how you do.
Follow up: 2 months
Subjective Assessment:
- Has regressions if deviates from diet (gluten, popcorn), other foods OK (cheese, grains feel good)
- Gluten might cause nerve pain
- Improved:
- Bloating, constipation, skin, weight, clothes fit better
- Same:
- Slight fatigue, female, PMS, cravings, headaches
- Worse:
- n/a
Impression:
- Continues to improve. Fatigue and hormonal symptoms are least responsive. Gluten seems to cause neuro reactions. Today will start on iron (ferritin, fatigue), female hormone support, and higher carb (does better here), and reintro of FODMAPs. Finishing touches now.
Recommendations:
- Starting
- Bring a bit more carbohydrate back into diet
- Gradually reintroduce FODMAPs into diet, move towards a regular Paleo Diet
- Be cautious with gluten, it may be best to strictly avoid this given the pain reactions
- NRT: Ferrochel
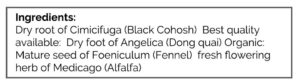
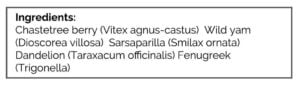
- Cycling Female: Estro + Progest Harmony
Follow up: 2-3 months
Subjective Assessment:
- Iron supplement – thinks it helped fatigue
- Increasing carbohydrates – is satisfying
- Female hormone support supplement – relieved headaches, cravings, PMS
- FODMAP reintroduction – some bloating and weight increase, so has stayed low FODMAP
- Improved:
- Fatigue, bloating, constipation, skin, PMS, cravings, headaches, brain fog, depression
- Same:
- Weight (up/down)
- Worse:
- n/a
Impression:
- Is under stress now, which is impacting weight. However, overall, she is doing great and all chief complaints have improved (other than weight). Iron supplement appears to have helped energy, hormonal support has helped headaches, cravings, and PMS and is feeling more satisfied with more carbohydrates. Will advise on weaning off program now, refer to Dr. Nelson for macros and follow up as needed.
Recommendations:
- Start:
- See Dr. Mike Nelson for weight/macros
- Take iron supplement for four months, then either stop or retest, but OK long term if desired. Recommended retesting: CMP, CBC w/ diff, and iron panel.
- Come off the Multi, EPA, and vit D when desired.
- Stay on female hormone support for another 2-3 months.
- Work to increase protein intake and track food in Cronometer.
Follow up: As needed or once yearly
Dr. Ruscio’s Comments
Her symptoms, fatigue, and constipation could have easily been attributed to the thyroid. This provides a clear example of how we should start with basic thyroid replacement (LT4) and GI care, then reevaluate. She did great on Paleo low FODMAP and probiotics.
Then, we found normality of fT4 and fT3 via the most sensitive thyroid hormone measure, dialysis/LC-MS. Also, remember that her levels may have improved slightly if her absorption of medication was improved as her gut became healthier.
Finally, a slight push to balance her female hormones with herbal supports and we saved this patient from months or years of pursuing thyroid fine-tuning. There is a time and place for that, just make sure to follow the algorithm so you perform the right therapy at the right time.
I have received several questions about a recent 60 Minutes’ expose on probiotics. After watching this video, quite frankly, I was shocked at how misinformed and unbalanced the piece was. They exhibited a clear bias, portraying probiotics as ineffective and even went as far as to insinuate they could harm children and were being snuck into infant foods with a profit motive.
I could not believe how poorly done this episode was, so I have put together a response. We will also be sharing this on the public area of the website but I wanted to get this data to our clinicians with some of my additional commentary so you can respond to patient/client questions.
High-Quality Data About Probiotics
Dr. Patricia Hibberd claimed “There’s not enough high-quality research to recommend off-the-shelf probiotics for the medical problems for which they’re commonly used”, and “There’s a lot of conflict among scientists about whether probiotics provide any benefit at all.”
Certainly, I wouldn’t say that probiotics are a panacea, and I agree there is a need for more research to confirm the trends that have emerged from the research.
However, there is ample evidence from meta-analyses and systematic reviews that compile the results of numerous clinical trials showing probiotics are a safe and effective treatment for various conditions.
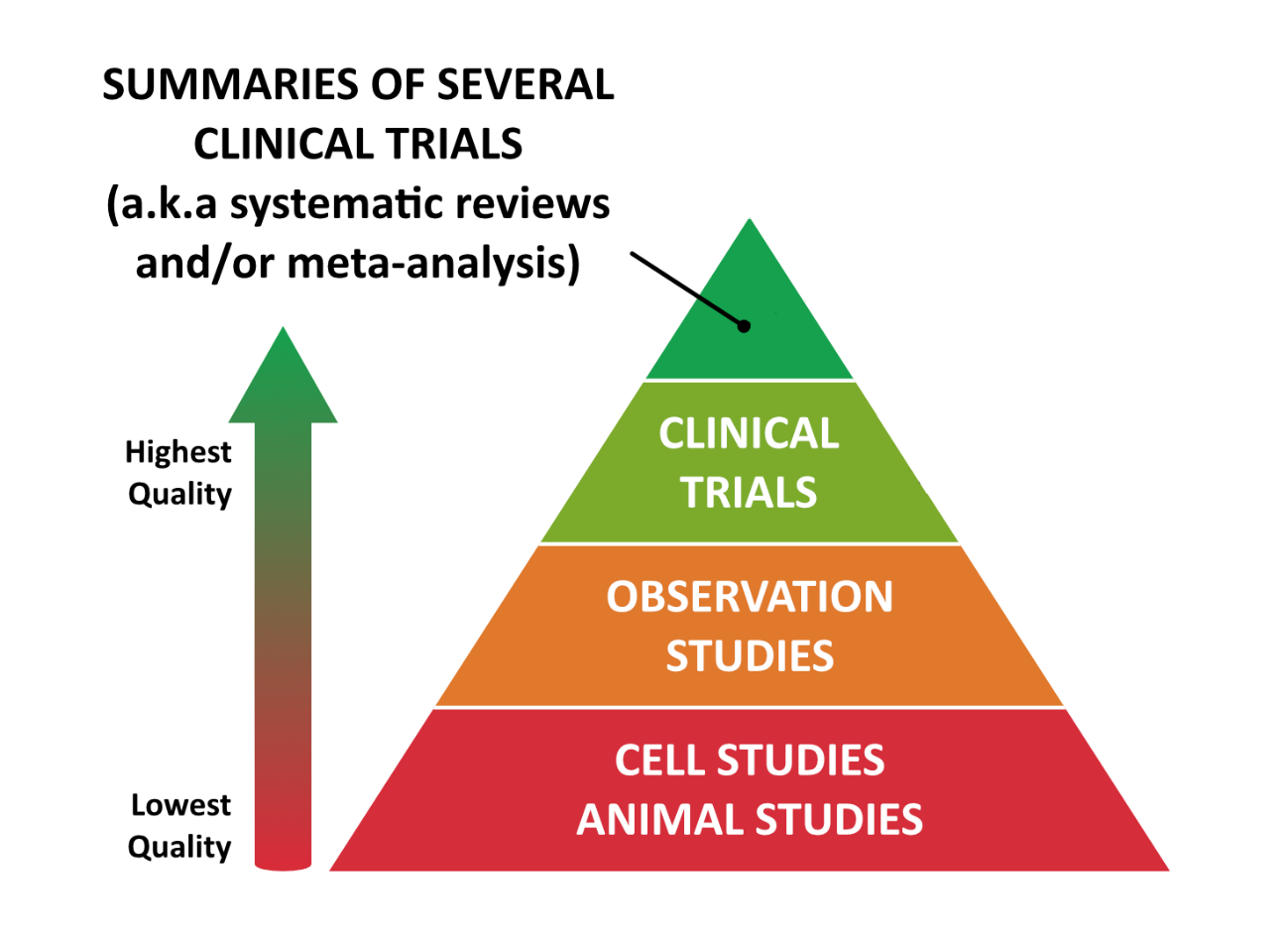
There’s a widely-accepted hierarchy of research quality, as shown in this pyramid diagram:
The difference between these levels of evidence is similar to the way restaurants are reviewed. You could ask one person’s opinion about a restaurant, but they may have been there on a particularly bad night. If you ask a group of friends, you might get a few different opinions. If you look online, you might find hundreds of reviews and now you can see overall trends and an average score.
The highest levels of evidence are summaries of multiple studies. These include:
- Systematic Reviews – A review of all the available research data on a given topic.
- Meta-Analyses – A review of all the available research which evaluates all the data together to show overall trends.
Both of these types of studies protect against cherry-picking and bias and are considered the gold standard of research. If their results are positive, they are the equivalent of a 4- or 5-star review of a restaurant on Yelp! or Google.
High-Level Evidence Clearly Shows the Benefits of Probiotics
According to the research, there is high-level scientific support showing that conditions such as Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), mood disorders (such as depression), and gut infections respond well to probiotics.
There is also limited, but encouraging scientific support showing probiotics can benefit brain function, hormones, seasonal allergies, autoimmune conditions, and sleep.
There may not be agreement among all scientists, but to characterize these results as inconsequential is entirely inaccurate.
Let’s review specific data about the claims 60 Minutes and their guests made during the segment.
 |
Probiotics Don’t Reduce Antibiotic-Associated Diarrhea |
When asked if there was any evidence that probiotics help antibiotic-associated diarrhea, Dr. Patricia Hibberd unequivocally said, “No.” Evidence suggests she is wrong.
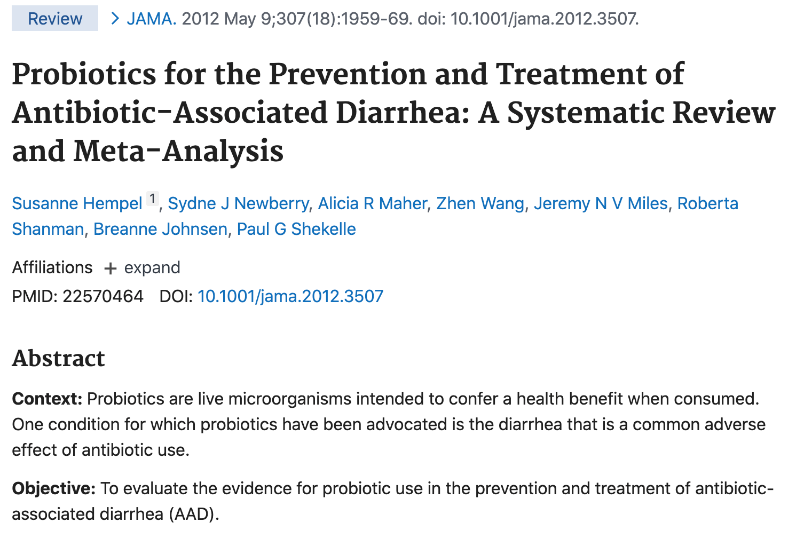
The Journal of the American Medical Association published a meta-analysis of 82 randomized-control trials on antibiotic-associated diarrhea. The study included trials of several different types of probiotics and concluded
“The pooled evidence suggests that probiotics are associated with a reduction in Antibiotic-Associated Diarrhea.” [1]
That’s one review, but is there a chance that this is a selective citation? Nope. Here are two additional meta-analyses confirming the same result:
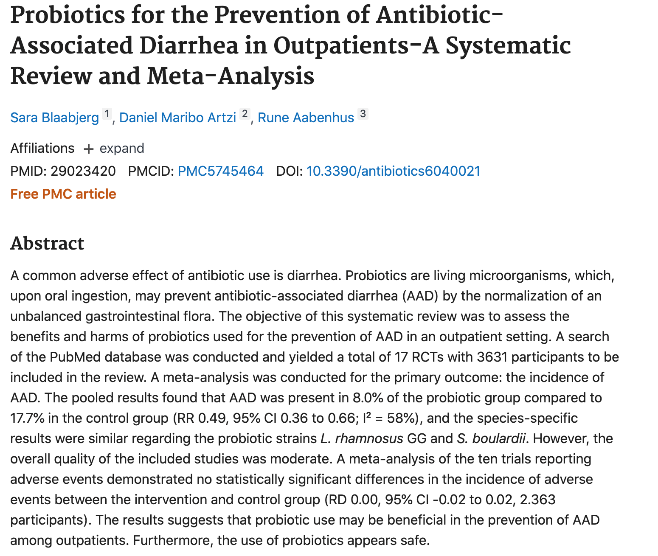
- A systematic review and meta-analysis of 17 randomized controlled trials pooling 3631 participants found that subjects using probiotics had half the rate of antibiotic-associated diarrhea compared to controls. [2]
- A systematic review and meta-analysis of 51 randomized controlled trials pooling 9569 participants concluded: “Lactobacillus rhamnosus GG (LGG) had the highest probability of being ranked best both ineffectiveness and tolerance on prevention of AAD.” [3]
These data may not suggest that everyone will prevent or avoid antibiotic-associated diarrhea if they use probiotics, but the evidence clearly suggests that probiotics at least reduce the incidence of antibiotics associated with diarrhea. Stating otherwise is not an accurate statement.
 |
Probiotics Don’t Help Irritable Bowel Syndrome (IBS) |
When asked if there was any evidence that probiotics could be used to treat irritable bowel syndrome (IBS), Dr. Hibberd also said, “No.” This surprised me because there is very good evidence – both meta-analyses and clinical trials – that show people with IBS benefit from probiotics.
- Two meta-analyses have shown probiotics to be an effective treatment for IBS, with no side effects.[4] [5]
- In another meta-analysis, the results of 20 placebo-controlled clinical trials were reviewed, including a total of 1,404 subjects. The probiotic group showed improvement in global IBS symptoms when compared to the placebo group. [6] This includes improvements in:
- Constipation, diarrhea, and/or loose stools
- Abdominal pain
- Bloating
- Flatulence
- Food intolerance
- Fatigue and difficulty sleeping
These three meta-analyses share the results of a total of 28 clinical trials, which collectively suggest probiotics are beneficial for treating IBS.
While I can appreciate someone like Dr. Hibberd being circumspect regarding probiotics, her statement could lead those suffering from IBS to avoid probiotics which have been demonstrated to alleviate this suffering and ostensibly improve quality of life, reduce days of missed work, etc….
 |
Probiotics Don’t Help Allergies |
Dr. Hibberd also claimed there was no evidence that probiotics have been shown to be beneficial for allergies. There isn’t as much evidence here as for IBS, but there are still some very promising data.
- A meta-analysis of 22 randomized control trials concluded that probiotics can significantly improve seasonal allergies. [7] The results claimed: “Despite high variability among the studies, synthesis of available data provided significant evidence of beneficial clinical and immunologic effects of probiotics in the treatment of allergic rhinitis.” Another high-quality study supports this same finding. [8]
- There is also data, albeit mixed, suggesting that probiotic supplements given to children may prevent or reduce the formation of allergies. [9]
 |
The Effects of Probiotics are Due to the Placebo Effect |
Meta-analyses and systematic reviews typically only include randomized and placebo-controlled trials. The design of these randomized, double-blind trials protects against the placebo effect and other researcher bias. If a randomized, double-blind study concludes that a probiotic intervention performed better than a placebo, then there is likely true benefit to that intervention.
 |
Probiotics Don’t Colonize the Gut |
It’s widely accepted and known that most probiotics don’t colonize the gut. The exception to this are the soil-based probiotics. [10]
The 60 Minutes segment highlighted this fact with the apparent intention to suggest that because probiotics don’t colonize the gut, they don’t have benefits. Despite the fact that most probiotics don’t colonize the gut, they still have beneficial effects on the immune and inflammatory balance in the gut.
 |
Probiotics Shouldn’t Be Taken with Antibiotics |
Doctors Eran Elinav and Eran Segal shared the results of their study in the 60 Minutes segment that showed people who used probiotics with antibiotics took longer for their microbiome to return to normal after the course of antibiotics.[11] While this is an interesting study result and is cause for concern, it’s also just one small study among a larger field of meta-analyses and systematic reviews.
There are a lot of data showing that using probiotics during antibiotic therapy leads to better outcomes and fewer side effects during treatment.
Consider:
- A systematic review of 20,215 patients with H. pylori infections showed that patients who took probiotics and antibiotics together had better results than patients who only took antibiotics. [12]
- A systematic review of 63 clinical trials found that in healthy subjects who experienced a disturbance in their microbiota after antibiotic use, 83% of subjects experienced recovery in their microbiota after taking probiotics. [13]
- There is also research to show that probiotics and antibiotics are more effective together for SIBO and other gut infections:
- One study of 40 patients with SIBO showed more than double the success rate in those taking a combination of S. boulardii and metronidazole (an antibiotic) when compared to those taking metronidazole alone. [14]
- Another study showed a combination of probiotic and antibiotic therapy normalized glucose breath tests for 13 out of 15 patients with both SIBO and Crohn’s disease. [15]
Though more study needs to be done, we do have reasonable evidence to suggest that using probiotics with antibiotics improves their effectiveness, and reduces their side effects. There is also the data suggesting that probiotics reduce antibiotic-associated diarrhea (see above).
Sadly, 60 Minutes appears guilty of cherry-picking one, small and less significant study, and overlooking the wealth of higher-quality data, thus misleading the viewer.
 |
Probiotics May Not be Safe for Infants and Babies |
It’s understandable that we want to make sure that what we give to babies, infants, and children is safe. However, to claim that just because there are no long-term studies demonstrating their safety we shouldn’t use them, disregards the proven benefits of probiotics for infants and babies.
For example, researchers have found the following benefits from probiotic use for babies: [16]
- Less colic and irritability
- Less diarrhea
- Fewer spitting episodes
- Fewer respiratory infections
More studies show that probiotics:
- Appear safe for infants and even preterm infants [17] [18]
- Protect infants against intestinal fungus (candida) overgrowth [19]
- Reduce the risk of ear and respiratory infection in babies [20]
In fact, because many babies are born today by C-section, they miss getting the inoculation dose of their mother’s probiotic bacteria. [21] C-section babies are at greater risk for health conditions like asthma, allergies, reduced bacterial diversity, and future obesity. [22] [23]
Though probiotic supplements will never live up to the diversity and complexity of the mother’s native microbiome, giving C-section babies probiotics may help protect against some of these long-term health consequences.
Overall, again I would argue that 60 Minutes’ claims stand to pose more detriment than benefit for the viewer.
 |
Probiotics Haven’t Been Shown to be Safe |
Dr. Frank Greer claimed on 60 Minutes that there are no long-term studies to show that probiotics are safe. While it’s true that there aren’t long-term studies, there is a general consensus that probiotics are considered safe in most cases.
The National Institutes of Health [24] states that probiotics are generally safe, even for premature infants. To quote:
“Given the large quantities of probiotics consumed around the world, the numbers of opportunistic infections that result from currently marketed probiotics are negligible. For example, probiotics have been administered to thousands of newborn infants, including some who were premature, without a single case of sepsis.”
There does appear to be some risk for immune-compromised patients, as 60 Minutes states, but there is still room for interpretation of this opinion.
The journal Expert Opinion on Drug Safety recommends the following: [25]
“Critically ill patients in intensive care units, critically sick infants, postoperative and hospitalized patients, and patients with immune-compromised complexity were the most at-risk populations.”
“While the overwhelming existing evidence suggests that probiotics are safe, complete consideration of risk-benefit ratio before prescribing is recommended.”
When it comes to immune-compromised individuals, recent research suggests that probiotics may actually be safe and beneficial.
An analysis of 57 clinical studies indicates that probiotic and/or synbiotic administration in immune-compromised adults is safe with regard to the current evaluated probiotic strains, dosages, and duration. There were no major safety concerns in the study, and overall, adverse events actually occurred less frequently in immune-compromised subjects receiving probiotics compared to the control group.[26]
That said, I will agree with 60 Minutes about the regulation of probiotics. There is little Food and Drug Administration (FDA) oversight of probiotics products on the shelves, and many products do not contain what they claim. For example, one study of 5 brands of soil-based probiotics showed only one brand matched its label claims. [26]
But given the potential and proven health benefits of probiotics, this shouldn’t be an argument against using probiotics, but rather an argument against using low-quality, unvetted products. Choose probiotics that are verified by third-party testing, have clear label-claims and expiration date.
The Bottom Line
Contrary to the claims promoted by 60 Minutes and their guests, probiotics have ample evidence and clinical data to support their use for IBS, antibiotic-associated diarrhea, infants and babies, allergies, and during antibiotic therapy. They are generally recognized as safe, and have benefits beyond the placebo effect, despite the fact that most of them don’t colonize the GI tract.
Consumers should be cautious to purchase probiotics from reputable sources and not to look at them as a panacea or a replacement for medical care.
In summary, I fear their recommendations will pose more harm than good for consumers by misleading them away from a safe and natural therapeutic.
Effect of Probiotic Supplementation on Migraine Prophylaxis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Nutr Neurosci. 2020 May 18;1-8. doi: 10.1080/1028415X.2020.1764292.
- Conclusions: A pooled analysis of available randomized controlled clinical trials showed that probiotic supplementation had no significant effect on the frequency and severity of episodic migraine attacks.
- To countervail the above, it is also important to acknowledge the limitations of probiotics, in this case with migraines.
Associations Between Migraine, Celiac Disease, Non-Celiac Gluten Sensitivity and Activity of Diamine Oxidase
Med Hypotheses. 2020 Apr 11;142:109738. doi: 10.1016/j.mehy.2020.109738.
- Results and conclusions: 9 of 10 patients with NCGS belonged to the decreased serum DAO activity group (group 1; n = 26), suggesting a strong relationship between reduced serum DAO activity and NCGS.
- In my experience, histamine intolerance diminish as gut health improves. This is likely because of inflammation and damage to the villi can decrease DAO (histamine degrading enzyme) production.
- So, fix the GI, which will restore DAO production, and subsequently see histamine tolerance improve.
Association Between Levothyroxine Treatment and Thyroid-Related Symptoms Among Adults Aged 80 Years and Older With Subclinical Hypothyroidism | Endocrinology
https://jamanetwork.com/journals/jama/fullarticle/2753909
- Findings In this pooled analysis of data from 2 randomized clinical trials that included 251 participants aged 80 years and older, treatment with levothyroxine, compared with placebo, was not significantly associated with improvement in thyroid-related patient-reported quality of life outcome scores for hypothyroid symptoms or tiredness.
- Meaning These findings do not support routine treatment with levothyroxine for subclinical hypothyroidism in adults aged 80 years and older.
- As we have discussed on the podcast prior, there appears to be a normal, age-associated elevation in TSH which does not require hormone replacement. This is important to bear in mind as overzealousness with thyroid evaluations may subject aging populations to unneeded medication.
Organic Acid Testing
A Practitioner asks:
Should I be ordering any other tests alongside an Organic Acid Test to help improve interpretation?
If you wanted to get specific about other tests to have alongside or before organic acid testing, even for gut directed symptoms, I strongly support baseline blood chemistry and certain nutritional markers to build a bigger picture. For example, while there are limitations to Serum B12, Folate and B6 levels, it is really helpful to have these and homocysteine when looking at some of the urinary organic acids to see if they are concordant or discordant, essentially saying does this person really have a nutritional deficiency.
So ultimately, baseline blood chemistry and nutritional markers may be helpful to build a better picture when choosing to perform OAT and prevent making incorrect interpretations from the OAT alone.