Practitioner Case Study – September 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
Case Study
Patient Info:
- Angela, 41 y/o, Female
- Previous Dx
- Hypothyroidism at 19 y/o (potentially without labs)
- Bell’s palsy around 2005
- Meibomian gland dysfunction diagnosed around 2017
- Potential fatty liver
- Rx
- Levothyroxine 75 mcg (Hypothyroidism)
- Chief Complaints
- Fatigue, 8-IN
- Anxiety, 8-IN
- Brain Fog, 7-IN
- Itchy Scalp, 9-IN
- Lack of deep sleep (hot flashes), 7-IN
- Joint Pain, 4-IN
- Other Symptoms
- Female, severe – irregular, heavy flow, PMS, hot flashes
- Allostatic Load – mod/severe – fatigue, fasting, sleep, cravings
Visit 1 (Day 1) – History and Exam
Initial Impression
- Angela is a generally healthy 41 y/o female, on a paleo-like diet, with a good lifestyle demeanor and outlook.
- Dx/Rx
- Dx:
- Hypothyroidism (potentially without labs). Bell’s palsy. Meibomian gland dysfunction. Potential fatty liver.
- Rx:
- Levothyroxine 75 mcg (Hypothyroidism)
- Previous Testing
- CBC (no ferritin), CMP – normal
- TSH – normal
- Onset:
- Gradual onset, but did appear worse postpartum and after coming off of hormonal birth control.
- Family History
- Rheumatoid Arthritis
- Diabetes
- Hypothyroid (mother)
- Prior Treatments:
- Helpful: fiber, enzymes, paleo, birth control, progesterone.
- Non-responsive: Thyroid Rx, probiotics, Restore.
- Notes/DDx
- Female hormones and GI are chief focus, could have silent GI imbalance contributing to symptoms.
- May also require more carbohydrates, have abdominal adhesions, or need to get off unnecessary thyroid medication. Need to qualify if she is truly hypothyroid.
- Prognosis
- Good to excellent
- Dx:
Previous Diets
- Whole 30 – helpful, not enough fiber.
- AIP – helpful, not enough fiber.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests Ordered
- LabCorp
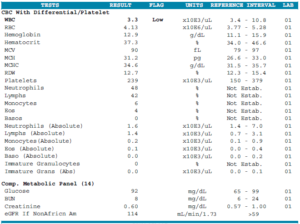
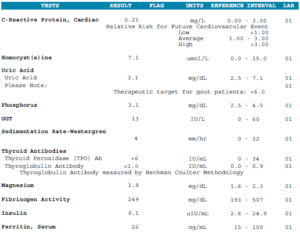
- CBC w/ diff, CMP, Hemoglobin A1c, Vitamin D
- Lipid panel, Insulin, CRP, homocysteine, fibrinogen
- Sedimentation Rate-Westergren
- Uric acid, phosphorus, GGT, magnesium
- Iron, TIBC, Ferritin
- Free T4 by dialysis-LC/MS, TSH, Reverse T3
- TPO and TG antibodies
- Optional:
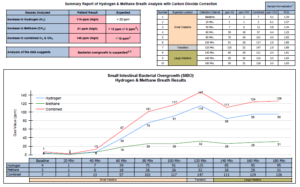
- Aerodiagnostics Lactulose SIBO breath test
- GI-Map stool test, without zonulin
- Rationale
- Fairly straight forward. We will assess thyroid via the more sensitive dialysis-LC/MS to ensure her dose is correct. The GI testing may help identify if there is a GI imbalance present that is manifesting extra-intestinally.
- LabCorp
Recommendations
- Diet
- Continue previous Paleo-like Diet. Work to slightly increase carb intake. Use My Fitness Pal to monitor daily carbs for 1 week and make sure to consume at least 150-200 grams per day.
- Eat every 3-4 hours.
- NRT: Vit D/K, Omega-3 supplement
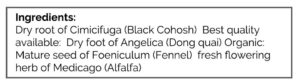
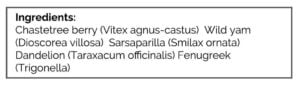
- Cycling Female: Female Hormone Support Herbs
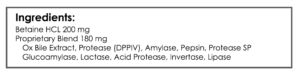
- GI: Fiber, Prebiotic, Digestive Enzyme
- Note: Be on the diet for 2 weeks before adding in the supplements, but continue diet until follow up. Then be on the supplements for 3 weeks before following up. Make note of the changes noticed from diet vs supplements.
- Sequence: testing, diet, supplement program, follow up.
- Follow Up: 6-7 weeks
- Rationale
- Some of the symptoms here could be due to inadequate carb intake, hence the slight bump up. When allostatic load flag high, consider this.
- Female hormones symptoms are clear, hence herbal support.
- Since digestive symptoms are minimal/non-existent, it is possible her GI health could improve with fiber and prebiotic support. I am more cautious to do this when GI symptoms are severe, however.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment
- Increasing Carbohydrates – was a shift, helped her energy, maybe mood and sleep
- Digestive Enzyme w/ HCl – very helpful (ran out for a few days)
- Female Hormone Support – helpful
- Fiber + Prebiotic – helpful
- Overall is much better today.
- Improved:
- Fatigue, anxiety, brain fog (not fully), joint pain, sleep & female (hot flashes).
- Same:
- Itchy scalp
- Worse:
- n/a
Lab Interpretation
- SIBO Breath Test: H2: 75 (74 rise), CH4: 26
- WBC 3.3-Low, Calcitriol 83-High
- TPO + TG Antibodies – normal
- Vitamin D: 39 – normal
- Ferritin: 22 – normal
- FT4 by dialysis – normal
Impression
- Overall is much better today. All treatments have helped. Labs show SIBO and low ferritin. Today will start on probiotics and iron, then follow up in 2 months.
Recommendations
- New
- Nutrient Replacement Therapies: Iron supplementation (we will be retesting in Dec ’19)
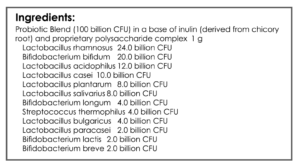
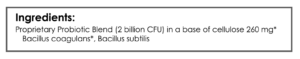
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, soil-based probiotic
- Start probiotics one at a time, every 3-5 days.
- Use Cronometer for food tracking
- Follow Up: 8 weeks
- Dr. R’s Note
- We could even make a case here to do nothing since she was responding so well.
Visit 4
Subjective Assessment
- “Digestion, energy and sleep are all better.”
- Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, soil-based probiotic – helpful.
- Improved
- Fatigue, anxiety, brain fog, joint pain, sleep & female (hot flashes), itchy scalp.
- Same
- Fatigue after lunch (slight), anxiety (slight) – Note: These are the least responsive of her symptoms, just to clarify. I list them here so it is easy for me to see in her chart.
- Worse
- n/a
Impression
- Today, “digestion, energy and sleep are all better.” Probiotics were helpful. Still has a bit of fatigue and anxiety, might be from unneeded thyroid medication or low ferritin. But today will trial lavender supplement, then retest ferritin before f/u in Dec. Consider thyroid withdrawal (coming of hormone and monitoring levels) in Jan.
Recommendations
- New
- Mood Support: Lavender
- Continue exercise + meditation
- Retest ferritin 2 weeks before next visit
- We can consider the thyroid withdrawal in Jan in collaboration with prescribing doc
- Follow Up: December 2019
Dr. Ruscio’s Comments
Few important notes on this case:
- SIBO cases can see improvements with fiber and prebiotics. Just be cautious because reactions can occur.
- Female hormone support and increasing carb intake can be impactful when allostatic load flags high.
- Will iron resolve her mild, remaining fatigue? Hopefully. Or, it will continue to improve with time.
- Part of her symptoms (especially anxiety and fatigue) may be from unneeded thyroid medication. We could not verify if her diagnosis was incorrect, so we will need to perform a withdrawal and monitoring. It is best to do this once most/all symptoms have improved, thus reducing variables. This will be one of our next steps.
Overall, another case that could have been much harder but was not because we were working one step at a time and focused on key issues.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!