Practitioner Case Study – July 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Dr. Ruscio’s Thyroid Medication Review: T4 Versus Combination Therapy (T4+T3)
- The Gut-Thyroid Connection, Profound but Underappreciated: Dr. Ruscio’s presentation at the LDN conference in June 2019.
- Rapid-fire Research – ultra concise summaries of noteworthy studies
- Randomized placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome
- Effect of vitamin D3 supplementation on blood pressure in adults: An updated meta-analysis
- Thyroid-stimulating hormone (TSH) serum levels and risk of spontaneous abortion: A prospective population-based cohort study.
Case Study
Patient Info:
- Eileen, 54y/o, female
- Previous Dx
- Psoriasis, Eczema
- Rx
- N/A
- Chief Complaints
- Itchy skin in groin area and neck, 3-CO
- Dry stools, 3-IN
- Other Symptoms
- Allostatic – mild
- Female – mild
Visit 1 (day 1) – History and Exam:
Initial impression
- Eileen presents as a 54yo female on a healthy diet, with a good lifestyle, demeanor, and outlook on her health.
- Dx/Rx:
- Psoriasis, eczema. Not currently taking any medication.
- Previous testing:
- Purported SIBO and Geotrichum. “high creatinine and low glomerular filtration also MCHC is low. These findings have been consistent for 10 years”
- Onset:
- Fairly healthy until 3 years ago. Started with lower abdominal pain and UTIs (3 in 1.5 years). Eczema and psoriasis on/off past several years, but worse in past 3.
- Family history
- Father who is 85 years old has kidney disease (has to watch his diet-oxalates) and mother had breast cancer.
- Prior Treatments:
- Habx and antifungals help, as has a lower carb diet.
- Nystatin & later Candibactin AR/BR – helped, but still 10% short. Topical antifungal – temporary help. Probios – help bowels. Gut healing cocktail – helpful.
- Notes/DDX
- Eileen may be able to improve the last 10% she is looking for by further gut care (habx, healing) or by changing her diet (low histamine or oxalate).
- She may also have Hg reactivity + tissue burden.
- Prognosis
- Since she is already 90% improved this might be as good as it can get, but I think mod-good chance she will improve further.
Previous Diets
Paleo-like, lower protein, mod/lower carb
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests ordered
- CMP
- CBC w/ diff
- Lipid panel
- Iron panel
- TSH, Free T4
- Vitamin D
- Hemoglobin A1C
- 24-hour urinary oxalates *important*
- Optional:
- Aerodiagnostics SIBO breath test
- GI-Map stool test
- Rationale
- We will assess for oxalate overload and any lingering GI dysbiosis or infection
Recommendations
- Diet:
- Continue previous Paleo-like, lower protein, mod/lower carb diet.
- Perform a 1-week trial on the Low Histamine Diet, in conjunction with the previous diet. Continue to reduce histamine if this helps.
- Practice intermittent fasting 2-3 days per week wherein you go 14-18 hours without food from dinner onward.
- NRT: Vit D/K, Omega-3 supplement, Curcumin
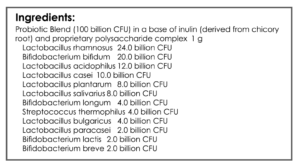
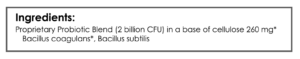
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, soil based probiotic
- Note: Please be on the diet for 2 weeks before adding in the supplements, but continue diet until follow up. Then be on the supplements for 3 weeks before following up. Please make a note of any changes noticed from diet versus supplements
- Follow Up: 4-5 weeks
- Rationale
- Assess if histamine intolerance is causing her symptoms
- Evaluate if a well-rounded probiotic protocol could resolve any presumed dysbiosis
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Low HI trial + Low Ox: helpful for bubbles in urine and skin. I did not recommend the low oxalate, however, when she saw I was testing for it she elected to use this handout from our patient resources page.
- NRT: Vit D/K, Omega 3’s, Curcumin. GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, soil based probiotic – may have caused dry stools and undigested particles in stools. Skin is much better.
- Improved:
- Bubbly urine, itchy skin
- Worse:
- Stool consistency
Lab interpretation:
- SIBO Breath test: not taken
- GI-MAP: Pseudomonas, Klebsiella, yeast, Gliadin IgA
- Ferritin – 36
- Oxalate (U24h) umol/d – 491 (range 40.9 – 431.7)
- Vitamin D: 25-OH nmol/L 50 – 250 Results: 240
Impression:
- Eileen has seen improved urine bubbles and skin from low HI + low Ox diet. Supplements appear NR and might cause rxn. Labs show elevated oxalates but the local doc did not run renal panel so can’t correlate to function currently, but historically has had low GFR. GI-dysbiosis also found. Today will continue with low ox diet/low hi diet, try to pinpoint supp reaction, and start Magnesium citrate. Then consider potentially adding Habx. Will also back off on vitamin D since she is nearly out of range high.
Recommendations
New:
- Do not take anymore than 4,000 IU of vitamin D per day
- Avoid gluten for now, then reintroduce later
- See low oxalate diet here: https://drruscio.com/dietary-oxalates-healthy-foods-harm-sally-norton/
- Continue to eat lower histamine and lower oxalate
- Eliminate supps (curcumin) and then start again to identify the irritant
- GI: Magnesium citrate
Follow up: 2 months
Visit 4
Subjective Assessment:
- Curcumin discontinuation – no change
- Magnesium citrate – helpful; bowels
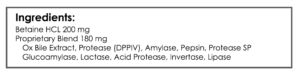
- Digestive enzymes – might help.
- Improved:
- Bubbles in urine
- Itchy skin
- Constipation/dry stools.
- Worse:
- n/a
Impression:
Eileen is continuing to improve and all CCs have responded. Stopping curcumin did not cause change. Magnesium citrate helped bowels. Enzymes (self-directed) may also help. Today will start on GI support nutrients, enzyme/HCl/bile.
Recommendations:
- New:
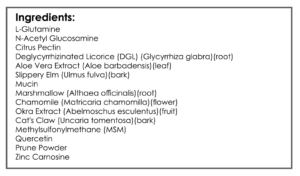
- GI: digestive enzyme, GI support nutrients
- Experiment with the Curcumin
- Continue using soap judicially
- Follow Up: 4-8 weeks
Dr. Ruscio’s Comments
This is a simple case but one that points out a few important insights.
- A low histamine diet can be helpful for some patients, as can a low oxalate diet. In this case, both may have been required. With time we will experiment to find the broadest possible intake of both.
- Lab testing, 24-hour urinary oxalates, may help predict who requires a low oxalate diet – I’m still evaluating this but so far it looks good.
- Probiotics can improve many causes of dysbiosis
- Sometimes a little magnesium is quite helpful to maintain regularity as the GI is adjusting to dietary changes and dysbiosis treatment.
- Citrate from minerals help bind oxalates, so this could have been a double bonus.
- Be on the lookout for over-supplementation with vitamin D
With time we will work Eileen to find minimal number and dose of her supplements.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!