Practitioner Case Study – February 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Vitamin D Treatment in Patients with Hashimoto’s Thyroiditis may Decrease the Development of Hypothyroidism.
- Effects of Long-Term Combination LT4 and LT3 Therapy for Improving Hypothyroidism and Overall Quality of Life.
- Non-Celiac Gluten Sensitivity: All Wheat Attack is Not Celiac
- Rapid-Fire Research – Ultra-Concise Summaries of Noteworthy Studies
- The role of low fermentable oligosaccharides, disaccharides, monosaccharides, and polyol diet in nonceliac gluten sensitivity.
- A low FODMAP diet is associated with changes in the microbiota and reduction in breath hydrogen but not colonic volume in healthy subjects.
- Recommendations for treatment of hypothyroidism with levothyroxine and levotriiodothyronine: A 2016 position statement of the Italian Society of Endocrinology and the Italian Thyroid Association.
- Effectiveness and safety of calcium and vitamin D treatment for postmenopausal osteoporosis.
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Kristen, 50yo, female
- Previous Dx
- hypothyroid
- thyroid nodule
- Rx
- levothyroxine
- vaginal progesterone
- Chief complaints
- brain fog/impaired memory**, 6-INT
- insomnia, 6-CO
- redface/red eyelids (Rosacea), 4-CO
- outer eyebrow missing, 6-CO
- teeth clenching, 5-INT
- Other symptoms
- female: heavy periods
- prevent cognitive decline
Visit 1 (Day 1) – History and Exam:
Initial Impression
- Kristen presents as a generally healthy 50yo female with a good diet, lifestyle, and outlook on health but could use some vigorous exercise.
- Her CC is cognition and preventing cognitive decline, also would like to improve sleep and skin. She has responded well to Levo, probiotics, fish oil and diet (paleo-like).
- I suspect we will find GI imbalance, she needs some hormone support (adrenal/female) and needs to obtain more exercise.
- She may also have HI or sleep-disordered breathing so mind this ddx.
- I anticipate she will do very well with this approach, prognosis good to excellent.
- Previous testing:
- na
Previous Diets
- Paleo-like – helpful.
Previous Treatments
- Levo – helped energy/puffy eyes. Probiotics – helped skin. Fish oil – helps skin. Vitex – not sure. Progest cream – not sure.
Visit 2 (A few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- BioHealth 401H stool test
- Blood panel
- CBC w Diff & platelet count
- Metabolic Panel, Comprehensive
- Lipid Panel
- Iron Panel: iron, TIBC, Iron Sat., Ferritin
- Sed Rate (ESR), Westergren
- Insulin, fasting
- Hemoglobin (HGB) A1c
- C-Reactive Protein (CRP) Quant.
- Vitamin D
- Thyroid Autoantibodies (TPO and TGA)
- T-4, Free (Thyroxine, Free)
- Thyroid-Stimulating Hormone (TSH)
- Rationale
- SIBO and dysbiosis/pathogen testing should be performed given the gut-thyroid connection, and due to the gut-brain
- A standard blood panel to screen for anemias, vitamin D and thyroid antibodies and hormone levels should also be performed.
Recommendations
- Diet and lifestyle
- Please continue your paleo-like diet, wherein you eat lower carb during the day and have some carbs at night.
- Eat regular meals, every 3-4 hours.
- Have a snack before bed and again when you wake up at night and see if this helps your sleep.
- Exercise at least 3x per week, vigorously, to the point of breaking a sweat.
- Treatment
- NRT: multi, vit D/K, DHA/EPA. On her own; curcumin, resveratrol, vitamin C
- Adrenal: Pregnenolone, DHEA
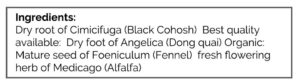
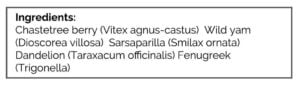
- Female hormone support herbs
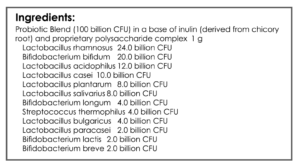
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, Fiber
- Rationale
- You could make an argument for a trial on a more restrictive diet (AIP or Paleo low FODMAP), but I had the sense that her problems were more so driven by dysbiosis and a need for some hormonal support.
- Adrenal support, plus female hormone support are indicated given her symptoms. In my opinion, testing is not needed to guide either of these.
- Probiotics and fiber may improve her GI
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Eating before bed – helpful
- Meals before bed/when waking – helpful
- Exercising – working on it
- Initial program – helpful
- Improved:
- Insomnia (much better), red face/eyelids (slightly), teeth clenching. Heavy periods.
- Same:
- Brain fog (slightly better).
- Worse:
- na
Lab Interpretation:
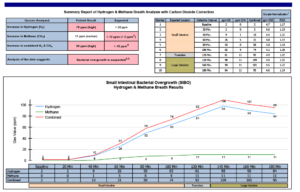
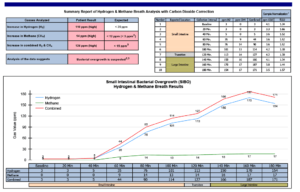
- Aerodiagnostics Lactulose SIBO breath test
- H2 101, CH4 14
- H2 101, CH4 14
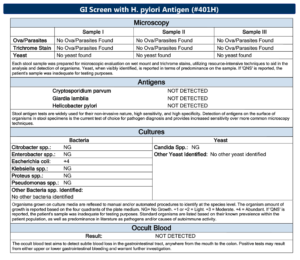
- BioHealth 401H stool test
- wnl
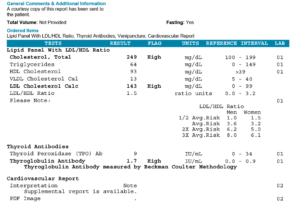
- Blood panel
- Lipid Panel Cholesterol 238-H, LDL 139-H
- Thyroid Autoantibodies (TPO and TGA) TGA 1.8-H
- Vitamin D 52-WNL
- Dx
- Severe H2 predominant SIBO. Hashimoto’s (TGA 1.8).
Impression:
- 6/28/17 –
- Pre-visit: Her CC is cognition and preventing cognitive decline, also would like to improve sleep and skin. I suspect we will find GI imbalance, she needs some hormone support (adrenal/female) and to obtain more exercise.
- Post-visit: Today’s SIBO, combined with hormone support and exercise is likely all that will be needed to resolve CCs. Kristen has responded moderately to initial program/diet. Starting on Habx base protocol today. Mind other ddx if MR.
Recommendations:
- Continue the previous program
- Starting
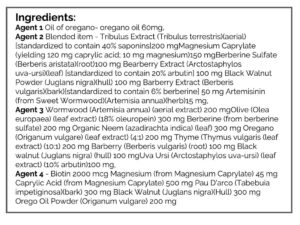
- GI: Habx base protocol
- FU: 4-5 weeks
Visit 4
Subjective Assessment:
- Month 1 Habx – well tolerated, MR.
- Overall is feeling good
- Improved:
- Insomnia (much better). Red face/eyelids (slightly). Heavy periods.
- Same:
- Brain fog (slightly better), teeth clenching.
- Worse:
- na
Impression:
- 8/2/17 – Today Kristen is still doing well but Habx appears minimally effective. She has not yet done 30 days on a strict paleo diet so we will start on this now, and finish Habx. Then fu and decide to continue/modify treatment or to retest.
Recommendations:
- Continue prior program, including Habx
- Starting
- Perform the Paleo Diet as the Whole 30
- start on motility support once you have finished the antimicrobials
- GI: motility support
- FU: 4-5 weeks
Visit 5
Subjective Assessment:
- Whole 30 – might have been too low CHO
- 2nd-month Hbx – seem helpful.
- Motility support – not sure.
- Overall feels at about 80% towards 100%
- Improved:
- Red face/eyelids, outer eyebrows. Slight: brain fog/memory, insomnia.
- Same:
- Teeth clenching, heavy periods.
- Worse:
- na
Impression:
- 9/6/17 – Today Kristen has seen all CC improve other than teeth clenching and heavy periods. Whole 30 may have been too low CHO. Will maintain current treatment plan today, but will start on the trial of PaleoLF/StandardLF Then fu 1-2 months and decide to retest or retreat with Habx. Also will consider low HI diet.
Recommendations:
- Continue previous
- Eat regular meals, every 3-4 hours.
- Continue to have a snack before bed and again when you wake up at night and see if this helps your sleep.
- Exercise at least 3x per week, vigorously, to the point of breaking a sweat.
- And
- NRT: multi, vit D/K, DHA/EPA. On her own; curcumin, resveratrol, vitamin C.
- Adrenal: Preg, DHEA
- Female hormone support herbs
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, fiber, motility support
- Now ending
- GI: Habx base protocol
- Starting
- Perform the Paleo Low FODMAP diet and/or the Standard Low FODMAP diet. Start more strictly for the first 2-3 weeks (this would be Paleo Low FODMAP) and then reintroduce (this would be Standard Low FODMAP).
- FU: 1-2 months
Visit 6
Subjective Assessment:
- Paleo LF (mostly) – felt fine either way.
- Improved:
- Red face/eyelids, outer eyebrows. Slight: brain fog/memory, insomnia. Teeth clenching, heavy periods.
- Same:
- still does get some red face/eyelids though**
- Worse:
- na
Impression:
- 11/8/17 – All of Kristen’s CCs have improved. She seems to do OK on either Paleo or PaleoLF. Today will have her reintro to broaden diet, maintain the current plan, and then retest before our next fu in about 2 months. At fu consider either program curtail or retreatment of SIBO.
Recommendations:
- Continue previous, and
- Starting
- reintroduce previously eliminated foods to broaden your diet
- perform retesting 2-3 weeks before our next follow up
- otherwise, maintain the current plan
- FU: 2-3 months
- Retesting
- Aero Lactulose SIBO
- Blood panel
- Lipid panel
- thyroid antibodies; TPO, TG
Visit 7
Subjective Assessment:
- Symptomatically doing well, might have even improved more than at last visit.
- Food reintro – went OK. Wheat slightly problematic.
- Improved:
- all CCs
- Same:
- na
- Worse:
- na
Objective Assessment:
- Aero Lactulose SIBO
- H2 65, rise 63. CH4 9.
- Blood panel retesting
- Lipid panel Cholesterol 249-H, LDL 143-H
- Thyroid antibodies; TPO, TG TG 1.7-H
Impression:
- 1/31/18 – Today’s labs show SIBO values greatly reduced, TGabs unchanged. Kristen continues to improve and has reached a peak level of improvement, which has been maintained after reintro. Will now start on program curtail and follow up as needed.
Recommendations:
- Dietary
- Please continue on your paleo-like diet, wherein you eat lower carb during the day and have some carbs at night. But, broaden your diet as instructed below.
- Eat regular meals, every 3-4 hours.
- Continue to have a snack before bed and again when you wake up at night and see if this helps your sleep.
- Exercise at least 3x per week, vigorously, to the point of breaking a sweat.
- Treatment
- NRT: multi, vit D/K, EPA/DHA. On her own; curcumin, resveratrol, vitamin C
- Adrenal: na
- Female hormone support herbs
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, Fiber
- Starting
- The following are OK longer term but experiment to find a minimal needed dose
- NRT: vit D/K, EPA/DHA
- Female hormone support herbs
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, Fiber
- Wean off now:
- Adrenal support, motility support
- FU: as needed and/or yearly checkup
- The following are OK longer term but experiment to find a minimal needed dose
Dr. Ruscio’s Comments
At her last visit, Kristen had maintained her new peak level of health for roughly 3 months and in the context of a dietary reintroduction. This suggests a very favorable prognosis. She still has a SIBO positive breath test, but the data don’t indicate that all patients need to be treated to ‘normal’ especially in the context of no symptoms. You could make an argument to do this, but I don’t feel it be a prudent course of action.
It also appeared that she did not experience much improvement after the first month of antimicrobials, but then turned the corner after the second month. This does happen so it is important not to discontinue Habx too soon as some respond late.
She did also have non-responsive TG antibodies, however, the data regarding the clinical significance of TG antibodies is unclear. So, I do not see the need to intervene with selenium, CoQ10 et cetera in a non-symptomatic patient. However, you could make an argument for this also.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!