Practitioner Case Study – September 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Non-celiac gluten sensitivity: people without celiac disease avoiding gluten—is it due to histamine intolerance?
- Serum-derived bovine immunoglobulin/protein isolate therapy for patients with refractory irritable bowel syndrome
- A review of the use of biotin for hair loss
- Rapid-Fire Research – ultra concise summaries of noteworthy studies
- Serial Frozen Fecal Microbiota Transplantation in the Treatment of Chronic Intestinal Pseudo-Obstruction: A Preliminary Study
- Escherichia coli Nissle 1917 in Ulcerative Colitis Treatment: Systematic Review and Meta-Analysis
- Selenium Supplementation Significantly Reduces Thyroid Autoantibody Levels in Patients with Chronic Autoimmune Thyroiditis: A Systematic Review and Meta-Analysis
- Iodine Nutrition Status and Thyroid Disorders: A Cross-Sectional Study from the Xinjiang Autonomous Region of China
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Katherine, 34yo, female
- Previous Dx
- Anemia APOE4/4
- Rx
- NA
- Chief Complaints
- Loose stools w/ undigested food, 7-CO
- Eczema, 6-CO
- Insomnia, 6-IN
- Get cold easily and fingers turn white and numb, 10-IN
- Brain fog, 5-IN
- Underweight, 8-CO
- Other Symptoms
- Burnout, mod – fasting, cravings, sleep
- Female, mod – GI, pain, flow
Visit 1 (Day 1) – History and Exam:
Initial Impression
- Katherine presents as a 34yo female with good diet, lifestyle and outlook on her health
- Dx/Rx
- She has been diagnosed with anemia previously and is on no Rx
- Previous Testing
- Only genetic testing
- Onset
- Her CCs started after travel in Africa and a Giardia infection, which was treated with Abx
- Prior Treatments
- She has previously responded well to AIP (autoimmune paleo diet), Habx, enzymes (with previous ND and health coach) and notices reactions to high histamine and high FODMAP foods, she does not do well with fasting
- Notes/DDX
- Katherine will likely respond to a term of low FODMAP and low histamine diet combined with treatment of any lingering dysbiosis. She may also need to eat more frequently, consume less caffeine and might need herbal HRT.
- Other
- If non-responsive consider ulcers, per her history, or helminths or histamine blockers
- Prognosis
- Prognosis good to excellent
Previous Diets
- Fermented foods – help GI. Paleo – helps skin. Fasting – shaky, irritable. AIP – most helpful; acne, eczema, PMS but GI NR. High FODMAPs & high histamine – flare GI and migraines.
Previous Treatments
- Giardia abx – cleared giardia. Habx, fish oil, D – helped eczema. Lauracidin – die off, then might help. Enzymes – helpful (gas, discomfort).
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aero Lactulose SIBO breath test
- GI-MAP stool test
- Quest #2 blood & urine
- Comprehensive blood chemistry and thyroid evaluation
- Quest #1 blood, urine, stool & breath
- Full GI panel
- Rationale
- Given Katherine’s symptoms, digestive tract dysbiosis or infection is highly suspected
- It is also prudent to perform a standard/comprehensive blood chemistry
- We will also rule out thyroid dysfunction and evaluate thyroid antibodies because some anemia (personal hx of anemia) may be driven by parietal cell autoimmunity and this has a 30% overlap with Hashimoto’s.
Recommendations
- Dietary
- Please start on the Paleo low FODMAP diet. You can avoid any foods on this list that you know do not agree with you.
- After 2 weeks on low FODMAP, continue with this diet but also follow the low histamine diet, as best you can, for 1 week. If this helps, continue to restrict high histamine foods.
- Make sure to eat every 3-4 hours.
- You can consume white rice, potatoes or other gluten-free grains to prevent weight loss. Or, add in our gut-friendly semi-elemental shakes using our semi-elemental diet.
- Please stop all caffeine.
- Have a snack before bed and when waking and see if this helps you sleep more soundly.
- Please be on the diet for 3 weeks before adding in the supplements, but continue diet until our follow up. Then be on the supplements for 3 weeks before following up. Please make a note of the change you noticed from each one of these.
- Sequence: testing, diet, supplement program, follow up
- Lifestyle
- NA
- Treatment
- NRT: vitamin D/K, Omega 3-6-9 blend, multivitamin
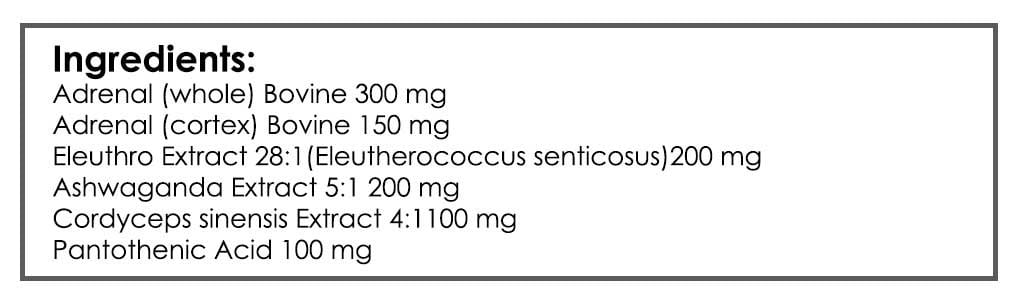
- Adrenal: Adrenal Support formula
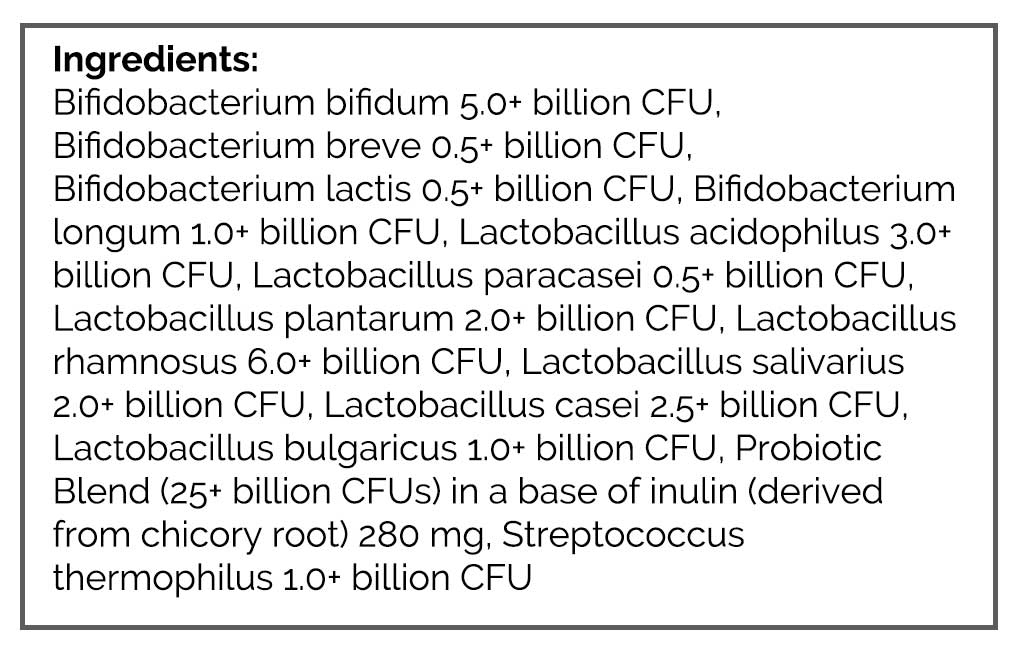
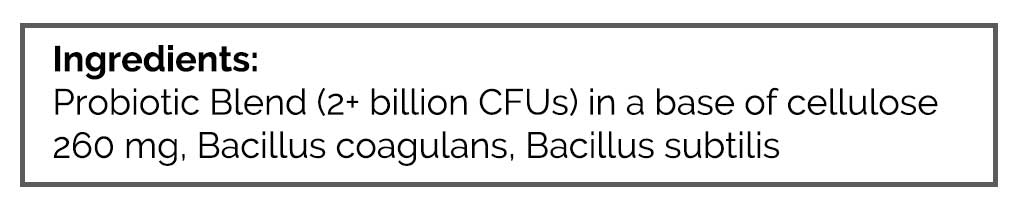
- GI: Lacto/bifido blend probiotic, S. boulardii probiotic, Soil-based probiotic – take all probiotics once per day only. Digestive enzyme/HCl
- FU: 7-8 weeks
- Rationale
- Dietary: We will revisit the dietary change of low FODMAP, which has previously been helpful, then layer in the low histamine diet to see if this provides synergy. However, since she showed some signs of high allostatic load/burnout (cravings, fasting intolerance, insomnia) she might need to increase her carb intake and eat frequent meals. This is where loosening dietary boundaries can make a sizeable impact. This is also why reducing caffeine intake may help.
- Supplemental: Adrenal support may help with some of the symptoms of burnout/high allostatic load (no testing needed). Probiotics may help remedy her symptoms and address the presumed dysbiosis. History of anemia may indicate digestive section support needed.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Stopping caffeine – very helpful; helped her sleep better
- Paleo low FODMAP diet – very helpful; gas, bloating, stool consistency
- Low HI diet – no change, but already ate somewhat low HI
- Frequent meals, more CHO, snack before bed – helpful
- Adrenal support – rxn, migraines
- Supplement program – may have flared Eczema
- Improved:
- Gas, bloating and stool consistency; Insomnia; Brain fog; Female: Flow
- Same:
- Get cold easily/fingers; Weight
- Worse:
- Eczema
Lab Interpretation:
- Aero Lactulose SIBO breath test
- H2: 12, rise 3 CH4: 15
- GI-MAP stool test
- H. pylori Dysbiotic: Pseudomonas spp.
- Blasto
- Fungus: Candida, Geotrichum
- Quest #1 blood, urine, stool & breath
- did not perform – too far away
- Quest #2 blood & urine
- did not perform – too far away
- Dx: GI-Map: H. pylori, Blasto, fungal and bacterial dysbiosis
Impression:
- 1/3/18 – Katherine will likely respond to a term of low FODMAP and low histamine diet combined with treatment of any lingering dysbiosis. She may also need to eat more frequently, consume less caffeine and might need herbal HRT. If NR, consider ulcers, per her history, or helminths or histamine blockers. Prognosis good to excellent. Today’s labs show [H. pylori, Blasto, fungal and bacterial dysbiosis]. Katherine has improved globally, only NR CCS might be due to reactions from multi (B vitamins) and/or Omega blend (nuts). Today will continue with current plan but will dc Multi, Omega, and start elemental formula to help with weight gain. At FU if not fully responsive will treat with Habx protocol.
Recommendations:
- Continue previous plan with the following modifications
- Stop the adrenal support now
- Come off the Multi for now
- Transition to nut-free omega blend
- Consider experimenting with an Elemental formula to gain weight
- Keep up the good work
- FU: 6-8
Visit 4
Subjective Assessment:
- Stopping Adrenal, Multi – improved HAs/migraines
- Feels better when eating fewer vegetables and fruits
- Low histamine – feels better
- Elemental diet – tolerated, helped with weight
- Improved:
- Eczema, headaches. Gas, bloating and stool consistency (not perfect though). Brain fog (even better). Insomnia. Female: Flow. Weight (gained back what she lost)
- Same:
- NA
- Worse:
- NA
Lab Interpretation:
- Quest #1 blood, urine, stool & breath
- Candida albicans IgG, IgA, IgM IgG 1.1-H, IgA 2.1-H
- Indicans, urine qualitative 1+
- Quest #2 blood & urine
- Unremarkable
- Dx: LC: Candida, potential dysbiosis. GI-Map: H. pylori, Blasto, fungal and bacterial dysbiosis
Impression:
- Katherine has done great; all CCs are now improved. Stopping Multi and Adrenal support resolved reactions. Elemental diet was well tolerated. She feels better when eating fewer vegetables, also when eating low histamine. Today’s pending labs from the last visit show candida. Today will work to broaden diet into a standard low FODMAP diet, with more starch/grain and less fruit/veggie. Then, at FU will work to curtail program and follow up as needed.
Recommendations:
- Continue previous plan with the following modifications.
- Continue to be cautious with histamine.
- Slowly start into your dietary reintroduction. Starting with the allowed foods on the standard low FODMAP food list. Work to increase your intake of starchy carbs and grains, while decreasing vegetables and fruit intake.
- At the next visit, we will wean off your program.
- FU: 2-3 months.
Visit 5
Subjective Assessment:
- Is still doing well, and even improving slightly – all CCs improved
- Feeling like can eat more foods with time, but still has to be cautious
- Low HI – tried strictly again and it was helpful for previous only non-responsive symptoms of itchy skin and is better digesting food
- Standard low FODMAP intro – OK; Sprouted oat and rice – OK; Potatoes and buckwheat – rxns
- Improved:
- Eczema, headaches. Gas, bloating and stool consistency (not perfect though); Brain fog (even better); Insomnia
- Female: Flow; Weight (gained back what she lost)
- Same:
- NA
- Worse:
- NA
Impression:
- Is still doing well, and even improving slightly – all CCs improved. Tried low HI again, even more helpful. SLF reintro – OK. At FU, if better 1st reintro 2nd program curtail. If regressing, consider Habx. Knowing that in some cases of histamine intolerance probiotics can initially be helpful, but then can cause oversaturation if the dose is not reduced, I am recommending today experimentation to find the minimal effective dose.
Recommendations:
- Continue previous plan
- Experiment with probiotics, take a few days to week off
- FU: 3 months
Visit 6
Subjective Assessment:
- Is currently a stressful time of year and she notices stress affects her stools negatively; seems like she’s become more reactive to foods
- Taking time off probiotics – no change
- Improved:
- Eczema (even better); Headaches; Histamine tolerance; Gas, bloating; Brain fog; Insomnia; Female: flow; Weight (gained back what she lost)
- Same:
- Stool consistency; FODMAP sensitivity
- Worse:
- NA
Impression:
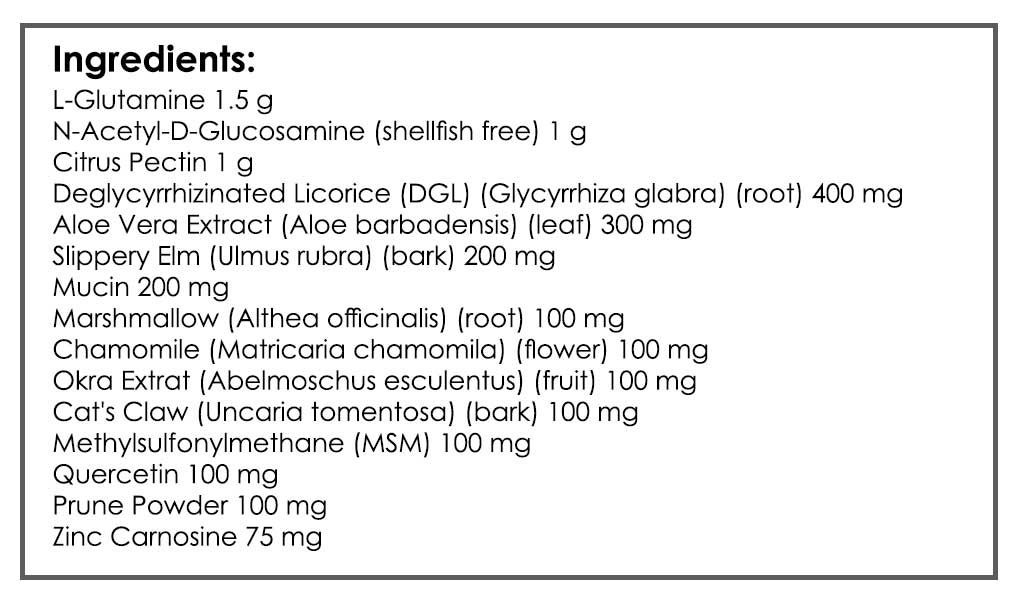
- Today Katherine has maintained all improvements (all CCs improved) other than loose stools and inability to reintro some FODMAPs. She is, even more, histamine tolerant and skin continues to improve. She is under work stress and she has noticed stress flares her loose stools historically. So, today decided to start on GI-repair cocktail and then fu 4 weeks after the stress has passed. We will consider the following at FU: if better 1st reintro 2nd program curtail. If regressing, consider Habx or SBI, histamine supports.
Recommendations:
- Continue previous plan, plus the following
- GI repair cocktail
- Also, consider rotating foods in your diet, as outlined in Healthy Gut, Healthy You.
- You’re doing great, don’t forget that 🙂
- FU: 2 months
Dr. Ruscio’s Comments
There are a few important lessons contained in this case study.
First, we see yet another case study where 2 different GI labs results do not fully match (yes, there was some overlap but they don’t fully match). Also, that the results didn’t require directed antimicrobial treatment.
Second, some people do better shifting to a dietary approach some would label ‘unhealthy’. Namely, in this case, more carbs, including some grains, and fewer vegetables and fermented foods.
Third, time can be a key factor for healing. Once we made a couple modifications to her initial program she started to improve visit by visit, without any additions changes needed. I will review a study in the FFMR soon showing a low histamine diet can actually resurrect one’s ability to produce the histamine metabolizing enzyme DAO (meaning the low histamine diet may ‘heal’ the intestines and allow better enzyme production).
Fourth, sometimes a flare of symptoms is normal and no cause for alarm. Katherine saw a slight regression in her stools during a period of heavy work stress. What she needed was calm reassurance from her doctor that this is OK and does not mean anything is ‘wrong’.
I hope you see the emerging theme here that listening to the patient, reading the signs their body provides and making incremental changes can allow you to piece together the puzzle of finding the ideal confection of stimuli required to allow healing.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!