Practitioner Research Review – October 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- Histamine-reduced diet and increase of serum diamine oxidase correlating to diet compliance in histamine intolerance.
- Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options.
- Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: Bridge between Functional Organic Dichotomy.
- Rapid-Fire Research – ultra-concise summaries of noteworthy studies
- Serum zonulin in patients with inflammatory bowel disease: A pilot study
- Trichuris suis ova therapy in inflammatory bowel disease: A meta-analysis
- Type of fish consumed and thyroid autoimmunity in pregnancy and postpartum.
- Helicobacter pylori CagA antibodies and thyroid function in latent autoimmune diabetes in adults.
- Blocking nocturnal blue light for insomnia: A randomized controlled trial
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Histamine-reduced diet and increase of serum diamine oxidase correlating to diet compliance in histamine intolerance.
https://www.ncbi.nlm.nih.gov/pubmed/30022117
Study Purpose
- To assess the impact of a low histamine diet on levels of DAO, the enzyme the body uses to metabolize histamine
Intervention:
- Retrospective chart review of 63 histamine intolerant (HI) patients, over a 13 month period
- Diet compliance assessed via questionnaire. Serum DAO levels tested.
- Histamine intolerance was diagnosed if: “presented with functional abdominal complaints and a serum DAO value < 10 U/mL”
Main Results:
- The greater the dietary adherence the greater the improvements in DAO levels.
- 4 levels of dietary compliance were identified
- Four diet-compliance groups, which were determined as:
- strict (HRD every day)
- occasional (HRD 3 days a week)
- rare (HRD once a week)
- no diet
- Four diet-compliance groups, which were determined as:
- 4 levels of dietary compliance were identified
- As seen in the image below, one needed to follow a low histamine diet for at least 3 days per week to obtain a significant increase in serum DAO. This is good news, it suggests ardent adherence is not required (of course ultimately use the response to reintroduction to dictate this).
- Significant increases in DAO levels correlated with symptomatic improvements (see 2nd chart below)
- 79% of subjects reported improvement in symptoms on a low histamine diet. Of these patients, 50% experienced increased DAO. Translation: DAO is part of HI but it is not the end all be all, so don’t overly rely on testing here.
- Sixty-three patients reported their symptomatology after initiating a HRD, 50 of these indicated improvement of symptoms (79%).
- Of these 50 patients, 33 also had an increase in DAO (52%).
- DAO levels increased from an average of 5.4 to 8.2, see image above.
- There was a significant increase of DAO from median 5.4 U/mL (range: 1.5–9.9) to 8.2 U/mL (range: 1.5–20.4), whereas DAO in 13 patients with continuing symptoms slightly decreased (p = 0.701)
Additional Results:
- Diagnosis of histamine intolerance
- Diagnosis of histamine intolerance (HIT) has been based on low serum diamine oxidase (DAO) values, functional gastrointestinal disorders and improvement of symptoms with a histamine-reduced diet (HRD).
- Serum DAO levels are not a reflection of gastrointestinal DAO activity, but may still be useful as part of HI diagnosis.
- Although serum DAO values are not established to reflect gastrointestinal DAO activity, the diagnosis of HIT can be supported with measurements of serum DAO (2).
- “DAO is the primary enzyme required for the degradation of ingested histamine and is synthesized by apical enterocytes located in the intestinal villi (8).”
Limitations:
- This was a small study and therefore some of the findings did not reach statistical significance (p-values not less than/equal to 0.05).
Authors Conclusion:
- “An HRD is useful, simple and inexpensive to reduce HIT related symptoms [9] and we here show symptom improvement in 79% and an increase of DAO in 52% of patients with HIT.”
Clinical Takeaways:
- A low histamine diet may improve the symptoms of histamine intolerance in roughly 80% of patients.
- A low histamine diet may also increase DAO levels in roughly 50% of patients who improve symptomatically.
- At least 3 days per week of adherence to a low histamine diet may be required to elicit these effects.
Dr. Ruscio Comments
A low histamine diet can be helpful in those who have not fully responded to other diets or other therapies. These studies suggest there may be a reparative effect of a low histamine diet and that adherence doesn’t have to be highly diligent.
Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options.
https://www.ncbi.nlm.nih.gov/pubmed/21418662
Study
Study Purpose
- Provide a guide to MCA disease/syndrome diagnosis and treatment
Intervention:
- Expert commentary
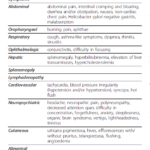
Main Results:
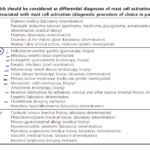
- While MCAS can sound intimidating, the treatment appears relatively straight-forward: anti-histamine agents, mast cell stabilizers and medications to manage any non-responsive symptoms.
- Effective therapy often consists simply of antihistamines and mast cell membrane-stabilizing compounds supplemented with medications targeted at specific symptoms and complications.
- The diagnosis of MCAS is something to consider in patients with multi-system symptoms which do not respond to other treatments and/or there is no other diagnosis to explain.
- Mast cell activation disease is now appreciated to be considerably prevalent and thus should be considered routinely in the differential diagnosis of patients with chronic multisystem polymorbidity or patients in whom a definitively diagnosed major illness does not well account for the entirety of the patient’s presentation.
- A history of allergic/inflammatory disorders dating back to childhood or adolescence should raise suspicion of MCAS.
- Symptoms often initially manifest during adolescence or even childhood or infancy but are recognized only in retrospect as MCAD-related.
- Moreover, symptoms often occur in a temporally staggered fashion, waxing and waning over years to decades.
- Symptoms also tend to gradually become more frequent and more severe over time.
- Patients with most types of MCAD often initially enjoy symptom-free intervals interspersed amongst symptomatic periods. Over time, symptom-free intervals shorten, and finally, symptoms become chronic with an intensity which fluctuates but with an overall trend toward steadily increasing intensity.
- The symptoms of MCAS can affect many systems including gut, respiratory, cardiovascular, dermatological and neurological.
- A questionnaire can be used to suggest MCAS.
- The foundation of treatment is avoidance of offender/trigger.
- The cornerstone of therapy is avoidance of identifiable triggers for mast cell degranulation such as animal venoms, extremes of temperature, mechanical irritation, alcohol, or medications (e.g. aspirin, radiocontrast agents, certain anesthetic agents). Individual patients may have variable tolerance patterns and avoidance lists, but it also is not uncommon to have no identifiable, reliable triggers.
- Treatment options are outlined below. They should also be trialed one at a time, allowing roughly 4 weeks to evaluate. Unless a reaction occurs, then stop immediately. As you can see, the foundation consists of antihistamines and mast cell stabilizers.
- First hints of success with any given therapy are usually seen within 4 weeks once suitable dosing has been achieved. Multiple simultaneous changes in the medication regimen are discouraged since such can confound identification of the specific therapy responsible for a given improvement (or deterioration).
- Ineffective or harmful agents should be stopped promptly.
Additional Results:
- MCAS may be responsible for some cases of IBS, fibromyalgia and interstitial cystitis
- Lab markers include: mediators tryptase, histamine, and heparin in the blood; methylhistamine in the urine and a CBC with differential.
- In addition to the detection of the characteristic clinical constellation of findings, it must be investigated whether levels of the mast cell-specific mediators tryptase, histamine, and heparin are elevated in the blood, whether the excretion of the histamine metabolite methylhistamine into the urine is increased, and whether mast cell activity-related eosinophilia, basophilia or monocytosis in the blood can be observed.
- In addition to a few others, listed below:
- Other useful markers fairly specific to mast cells include serum chromogranin A (in the absence of cardiac and renal failure, neuroendocrine cancer, and proton pump inhibitor use) and serum and urinary leukotriene and prostaglandin isoforms (e.g. leukotriene E4, prostaglandin D2, and prostaglandin 9α,11βPGF2).
- GI conditions/pathology are important to rule out before considering MCAS, this is why I advise exhausting all/most GI therapies before moving to MCAS.
Authors Conclusion:
- “MCAD comprises disorders affecting functions in potentially every organ system by abnormal release of mediators from and/or accumulation of genetically altered mast cells. There is evidence that MCAD is a disorder with considerable prevalence and thus should be considered routinely in the differential diagnosis of patients with chronic multisystem polymorbidity of unknown cause. In most cases of MCAD, diagnosis is possible by relatively non-invasive investigation. Effective therapy often consists simply of antihistamines and mast cell membrane-stabilizing compounds supplemented with medications targeted at specific symptoms and complications.”
Clinical Takeaways:
- MCAS might be responsible for otherwise non-responsive patients with multi-system symptoms
- History combined with a symptom questionnaire can firm up suspicion
- Testing is available but it is involved and somewhat non-specific
- Treatment centers around avoidance of triggers, antihistamines and mast cells stabilizing agents
- Conditions in the GI should be ruled out/address before considering MCAS
Dr. Ruscio Comments
MCAS can sound confusing at first pass, however, a good history and questionnaire can sharpen the diagnosis. Initial treatment could be rendered in a standard functional medicine practice, however, I would advise referring to an MCAS specialist if you are not making progress within 3-6 months.
Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge Between Functional Organic Dichotomy
https://www.ncbi.nlm.nih.gov/pubmed/28274108
Study Purpose
- Review the evidence connecting SIBO and IBS
Intervention:
- Review, non-systematic
Main Results:
- This is the most important point in this paper, in my opinion. As you can see below, the lactulose breath test leads to false positive testing (meaning people test positive for SIBO who likely don’t have it). You might be asking, but what if we use the earlier cutoff of 90 minutes to reduce these false positive? Great question. The data below were using the ‘early cutoff’ criteria and still found a significant false positive when using lactulose as compared to glucose.
- On average
- IBS patients tested 23% positive on culture, 26% positive on glucose and 45% positive on lactulose
- Healthy subjects tested 1% positive on culture, 5% positive on glucose and 21% positive on lactulose
- However, when using the glucose test, there is the risk of seeing a false positive in those with distal SIBO. So, we can’t say one is truly better than the other but perhaps more accurately that if one is using lactulose the test should be interpreted conservatively.
- early-peak criterion = rise in breath hydrogen within 90 minutes by 20 ppm above basal following lactulose ingestion
- SIBO is more common in those with IBS according to numerous studies and 2 meta-analyses
- (The) frequency (of) SIBO among patients with IBS ranged between 4% and 78% and that among controls, between 1% and 40% (37, 39, 40, 45, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68). Most case-control studies revealed that SIBO was commoner among IBS than controls; this suggests that there is significant association between SIBO and IBS.
- Two meta-analyses also suggested association between IBS and SIBO. In a meta-analysis by Ford et al. (69), of the 12 studies including 1,921 patients with IBS, pooled prevalence of a positive LHBT and GHBT was 54% (95% confidence interval [CI], 32% to 76%) and 31% (95% CI, 14% to 50%), respectively. The odds ratio (OR) for any test showing positive SIBO result among patients with IBS as compared to controls was 3.45 to 4.7 (69).
- In another meta-analysis on 11 studies, breath testing was found to be abnormal among patients with IBS than controls (OR, 4.46; 95% CI, 1.69 to 11.80). Breath testing had an overall sensitivity and specificity in separating IBS patients from healthy subjects of 44% and 84%, respectively (42).
- In the past five years, additional studies have further corroborated this.
- In these studies, frequency of SIBO among patients with IBS ranged between 19% and 37% and that among healthy controls between 0% and 12% (27, 39, 54, 62, 64, 67, 68, 70).
- Short chain fatty acids are toxic to the small intestine, despite being helpful for the large intestine
- Though short chain fatty acids are useful for colon by providing nutrients to the colonocytes, conservation of energy and absorption of water and electrolytes, in the small bowel, it inhibits nutrient absorption and inhibits jejunal motility (ileal brake) through liberation of peptide YY, neurotensin and glucagon like peptide-1, which promotes SIBO (89).
- SIBO may increase mast cell activation
- Immune activation in response to SIBO recruits increased number of intraepithelial lymphocytes, mast cells and enterochromaffin cells (100).
- Immune activation leads to hypersensitivity
- Moreover, mediators of host immune response trigger the enteric nervous system altering GI motility and visceral hypersensitivity, which are the major pathophysiological mechanisms of IBS (101).
Additional Results:
- Intrinsic causes of SIBO (note: there is more here than just motility):
- stomach acid & bile, motility, gut immune function, gut mucous membrane, gut-derived anti-microbial peptides, ileocecal valve
- There are several intrinsic and extrinsic factors that prevent overgrowth of bacteria in the small intestine. Intrinsic factors include: (1) secretion of gastric juice and bile, which have anti-bacterial effect; (2) peristaltic movement preventing adherence of bacteria into the intestinal mucosa; (3) normal gut defense including humoral and cellular mechanisms; (4) mucin production by intestinal mucosal epithelial cell inhibiting pathogenic bacteria; (5) gut antibacterial peptides such as defensins; and (6) ileocecal valve preventing retrograde translocation of bacteria from colon to the small intestine.
- stomach acid & bile, motility, gut immune function, gut mucous membrane, gut-derived anti-microbial peptides, ileocecal valve
- Extrinsic causes of SIBO –
- Diet, drugs (PPIs, H2 blockers, antibiotics, opioids…), pre and probiotics.
- Extrinsic factors include diet and drugs modulating gut flora, such as pre and probiotics, gastric acid suppressants such as proton pump inhibitors (PPIs), H2 blockers, and antibiotics and drugs altering motility (prokinetics, anticholinergics, and opioids)
- Diet, drugs (PPIs, H2 blockers, antibiotics, opioids…), pre and probiotics.
- ‘Gold standard’ duodenal culture may miss up to 70% of bacteria
- Though quantitative culture of the upper gut aspirate has traditionally been used as the gold standard for the diagnosis SIBO, its limitations include difficulty and invasiveness, cost, contamination by oropharyngeal flora, and inability to culture as high as 70% bacteria colonizing the gut.
- Culture may also be a poor measure 1) due to not sampling from the specific location of SIBO and 2) because air exposure may invalidate the sample
- Moreover, distribution of bacterial overgrowth may be patchy and upper gut aspirate may not be able to detect bacterial overgrowth in distal gut (30,32).
- The anaerobic bacteria may not grow if air is used during endoscopy; hence, either nitrogen or carbon dioxide is better for this purpose.
- There may be as many as 340 types of bacteria that can overgrow in SIBO. Note: this is why I do not feel we have to definitively identify exactly what is overgrowing (through gut bacterial mapping), but rather can use some testing to identify the theme of dysbiosis, then go to work on rectifying it while using symptoms to gauge improvement.
- In a recent study, using 212 different culture conditions, 340 different bacterial, 5 fungal species and one virus were identified, including 31 new species using culturomics (MALDI-TOF) technique (34, 35).
- SIBO pathology may include de-conjugation of bile, enterotoxicity, intestinal permeability, B12 deficiency, inflammation, and immune activation
- SIBO is more often associated with diarrhea than constipation-predominant IBS (7). Mechanism of diarrhea in patients with SIBO include de-conjugation of bile salts, enterotoxic effect of bacterial metabolites, increased small intestinal permeability, deficiency of vitamin B12 and low grade inflammation resulting from immune activation in the small intestinal mucosa (22,37,85).
- SIBO is associated with increased level of serum endotoxins, inflammatory cytokines and chemokines, and endogenous production of ethanol (23, 95, 98).
- SIBO may cause lactose intolerance
- Secondary deficiency of disaccharidases (e.g., lactase) is well known in patients with SIBO (8).
- “SIBO can be classified into two categories based on difference in bacterial flora”:
- (1) Gram-positive flora might be due to the failure of gastric acid barrier, and (2) coliform bacteria might be due to the failure of intestinal clearance and small bowel anatomical alterations (52, 77).
- Other culture studies have found a common grouping of bacteria found in SIBO
- Recently, one study based on culture of jejunal aspirates showed that Pseudomonas aeruginosa, Escherichia coli, Acenetobacter lwoffii, Staphylococcus species, Klebsiella pneumoniae, Streptococcus species, Acinetobacter baumannii, Enterococcus faecalis, and Enterococcus faecium were dominant bacteria among patients with SIBO (39).
- Pyleris et al. (54) reported that of 42/112 patients with IBS having SIBO, E. coli, Enterococcus species and K. pneumoniae were the predominant species. Gram negative bacilli and Enterobacter were most common on culture of jejunal aspirates among patients with IBS (54).
Interesting Notes:
- “The small intestine comprises mainly of Gram positive and aerobic bacteria and the large intestine contains predominantly Gram negative and anaerobic bacteria.”
- Rifaximin is effective, but as a monotherapy is not highly effective, in my opinion.
- with nonconstipating IBS (n=1,260) diagnosed by Rome II criteria. IBS subjects receiving rifaximin at a dose of 550 mg three times daily for 14 days reported adequate relief in global IBS symptoms as compared to identical placebo (TARGET 1: 40.8% vs 31.2%, p=0.01 and TARGET 2: 40.6% vs 32.2%, p=0.03) (115). Moreover, rifaximin was more effective in relieving abdominal bloating than placebo (TARGET 1: 39.5% vs 28.7%, p=0.005 and TARGET 2: 41.0% vs 31.9%, p=0.02) (115).
- Retreatment with Rifaximin is similarly effective
- Retreatment with rifaximin showed 33% response rate as compared to 25% in placebo group (p=0.02), consistent with FDA guidelines for clinical assessment of IBS drugs (1).
- Rifaximin may be better than other antibiotics for SIBO
- In a recent meta-analysis, efficiency of rifaximin (two studies) in eradicating SIBO was 64.1% as compared to 41% with other systemic antibiotics (metronidazole or tetracycline, p=0.003).
Authors Conclusion:
- “Though frequency of SIBO among patients with IBS varied between 4% and 78% patients, most studies reported the frequency to be higher among IBS than controls.”
- “Clinical phenotype of IBS may be used to consider treating patients empirically for possible SIBO.”
Clinical Takeaways:
- IBS is more common in those with SIBO
- Glucose testing more closely approximate duodenal culture results than does lactulose testing
- Short chain fatty acids may be toxic to the SI, perhaps part of the reason why low FODMAP diet is helpful for those with SIBO and IBS
- There are numerous causes of SIBO, both intrinsic and extrinsic
- Rifaximin is one effective therapy
Dr. Ruscio Comments
There is a lot in this paper and I don’t have much to add other than reiterating there are merits to each type of testing and that there are additional causes of SIBO than impaired motility.
Rapid-Fire Research – Ultra-Concise Summaries of Noteworthy Studies
Serum zonulin in patients with inflammatory bowel disease: a pilot study.
https://www.ncbi.nlm.nih.gov/pubmed/30160088
- Serum zonulin is highly sensitive for the evaluation of intestinal permeability in IBD patients.
- There is no correlation between zonulin values in serum and feces.
- Note: another study suggests serum and fecal may both have utility.
Trichuris suis ova therapy in inflammatory bowel disease: A meta-analysis.
https://www.ncbi.nlm.nih.gov/pubmed/30142867
- TSO therapy showed no statistical benefit for IBD patients, so it is suggested that clinicians consider its value carefully before putting into clinical practice. Perhaps continued investigations of larger sample size are necessary due to the previous results with lack of power.
- From Dr. William Parker, former podcast guest and helminth researcher
- I’ve been feeling guilty because I haven’t made the time to respond to that article. They included lots of data from experiments using helminths that were inactive due to high pH, and they’ve included experiments which could never have worked because they were too short-term.
Type of fish consumed and thyroid autoimmunity in pregnancy and postpartum.
https://www.ncbi.nlm.nih.gov/pubmed/26306774
- “These data reinforce recommendations that pregnant women should avoid consuming swordfish and indicate consumption of oily fish as a favorable alternative. Because thyroid autoantibodies are markers of autoimmune-related postpartum problems, our data suggest a dietary prophylaxis of such problems.”
- I have reviewed this study previously and details are available here.
Helicobacter pylori CagA antibodies and thyroid function in latent autoimmune diabetes in adults.
https://www.ncbi.nlm.nih.gov/pubmed/27775795
- This study found that only the virulent strain of H. pylori (identified with CagA) correlated with autoimmunity
- Prevalence of IgG against H. pylori and GagA was 52.1% and 20.9% respectively. Antibodies against H. pylori were not associated with TPO Ab and TSH.
- Antibodies against CagA showed a positive association with TSH and TPO Ab.
- Subjects with hypothyroidism (TSH ≥ 3.5 μU/ml) had an increased frequency of Ab anti-CagA
- I’m not convinced this strain testing needs to be performed routinely, however for those who would like to pursue testing, it is offered via the GI-Map test.
Blocking nocturnal blue light for insomnia: A randomized controlled trial
https://www.sciencedirect.com/science/article/pii/S0022395617308592
- Reducing blue light exposure before bed by wearing amber glasses can improve insomnia
- Wearing amber vs. clear lenses for 2-h preceding bedtime for 1 week improved sleep in individuals with insomnia symptoms. These findings have health relevance given the broad use of light-emitting devices before bedtime and the prevalence of insomnia.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!