Practitioner Case Study – October 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Histamine-reduced diet and increase of serum diamine oxidase correlating to diet compliance in histamine intolerance.
- Mast cell activation disease: A concise practical guide for diagnostic workup and therapeutic options.
- Small Intestinal Bacterial Overgrowth (SIBO) and Irritable Bowel Syndrome (IBS): Bridge between Functional Organic Dichotomy.
- Rapid-Fire Research – ultra-concise summaries of noteworthy studies
- Serum zonulin in patients with inflammatory bowel disease: A pilot study
- Trichuris suis ova therapy in inflammatory bowel disease: A meta-analysis
- Type of fish consumed and thyroid autoimmunity in pregnancy and postpartum.
- Helicobacter pylori CagA antibodies and thyroid function in latent autoimmune diabetes in adults.
- Blocking nocturnal blue light for insomnia: A randomized controlled trial
Practitioner Question of the Month
Practice Tip
Case Study
Patient info:
- Andrew, 33yo male
- Previous Dx
- na
- Rx
- na
- Chief Complaints
- Constipation 1BM/day or every 2 days, hard
- Heartburn (from CHO) – 10 – constant
- Brain fog – 10 – constant
- Fatigue – 8 – intermittent
- Anxiety/low motivation – 9 – constant
- Dizziness – 7 – intermittent
- Frequent urination – 6 – constant
- Other Symptoms
- Tinnitus, joint aches
Visit 1 (Day 1) – History and Exam:
Initial Impression
- Andrew presents as a generally healthy 33yo male with good diet, lifestyle and demeanor.
- He notices his overall health is better or worse depending on the health of his GI. He has seen some improvement in going AIP-autoimmune paleo (especially heartburn) but still has some and still has constipation, brain fog, and fatigue.
- Has seen some functional medicine doctors and done some treatment but no long-standing results. MD general practitioner workup all came back negative.
- I think the issue is indeed his gut but he hasn’t had a consistent plan with good follow through /competent FM GI doc.
- No unusual ddx.
- Prognosis good to excellent.
- Dx/Rx:
- na
- Previous Testing:
- Upper endoscopy – wnl (within normal limits, normal)
- Onset:
- Nothing noted
- Family History
- Father – high cholesterol. I think two of father’s siblings have had diverticulitis.
- Prior Treatments:
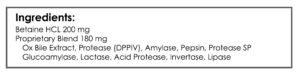
- Omeprazole – short-term relief. Habx – helped gas/bloating, not constipation – but can cause fatigue/depression. MotilPro – ginger burn. Iberogast – helped constipation short term. Betaine HCl – very helpful for digestion. Mg – helps constipation.
Visit 2 (A few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Glucose SIBO breath test
- DiagnosTechs GI-15 stool/saliva test
- Optional: Diagnostic Solutions GI-MAP stool test
- Blood Panel
- CMP, CBC w/ diff, lipid panel, iron panel, insulin fasting, TSH, fT4, vitamin D, Hemoglobin A1C
- Rationale
- Given his history, it makes sense to look into Andrew’s GI health.
- I think you can make a case either way for lactulose or glucose SIBO breath testing.
- The GI-Map is listed as optional since it may help but I also can’t say it’s fully required, so I leave it up to the patient. Those who want to be more aggressive usually elect for the optional test, those who prefer being cost conservative usually forgo the optional testing.
- The blood panel is a fairly foundational routine assessment: thyroid, anemia, vitamin D, blood sugar…
Recommendations
- Diet/Lifestyle
- Please perform the Modified Fast (see resources for PDF), then
- start on low FODMAP w/ SCD diet.
- After a few weeks on whole foods, try the semi-elemental diet for 2-4 days (see resources for PDF). If you do not tolerate this version well, consider experimenting with the others listed.
- Take a break for a short walk every 45 minutes to prevent mental fatigue.
- Supplemental
- Adrenal: Preg, DHEA
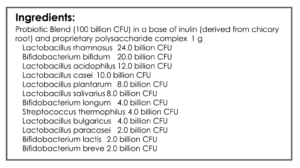
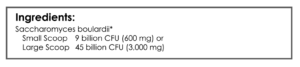
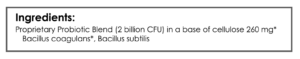
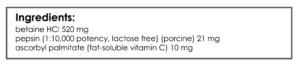
- GI: Lacto/Biff probiotic, S. boulardii, Soil-based probiotic, digestive enzyme with HCl, betaine HCl.
- After 2 weeks on plan, experiment with fiber supplement for 1.5 weeks
- Rationale
- Fasting can aid in GI repair. The low FODMAP with SCD diet may provide additional benefit for his GI.
- We will beta test elemental diet in case we need to use a full course later
- We will call for some rest in case he is overworking
- Preg and DHEA can improve fatigue, brain fog, and dizziness
- The probiotics, enzymes, and HCl can all help repair his gut and optimize digestion
- Fiber may aid constipation, but may also cause a flare, so this should be started in isolation.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Low FODMAP – very helpful. Addition of SCD (cutting rice) made him tired.
- MF (both, 4 days) – overall felt the same.
- GI: probiotics, enzymes, HCl – about the same.
- Has not tried semi-elemental diet
- Improved:
- frequent urination
- Same:
- constipation, heartburn, brain fog, fatigue, dizziness, anxiety
- Worse:
- na
Lab Interpretation:
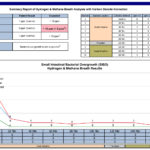
- Aerodiagnostics Glucose SIBO breath test
- H2 3, CH 0 – elevated baseline
- DiagnosTechs GI-15 stool/saliva test
- Taenia solium (tapeworm) IgA
- BioHealth 401H
- Endolimax nana
- LabCorp PCO
- Ferritin 401-H
- Dx
- Potential T. solium, E. nana. High Ferritin
- Summary
- T. solium found via antibody is inconclusive, so retesting can be important. T. solium can also be located in the brain (although extremely rare) and the larvae can expand when treated thus exacerbating neurological symptoms. So, it’s prudent to refer for conventional medical eval before treatment to cover your bases.
Impression:
- 11/11/16 – Since Andrew has neurological sequelae we will ask him to see GP before treating T. solium and also perform a retest to verify. Does well on low FODMAP but not with the addition of SCD. Will continue with the initial program today to eval fiber, then SED/ED, then also try low histamine, then fu. Has had elevated SIBO baseline on more than one test so might have proximal SIBO.
Recommendations:
- Diet/Lifestyle
- Take a break for a short walk every 45 minutes to prevent mental fatigue
- Supplemental
- Adrenal: Preg, DHEA
- GI: Lacto/Biff probiotic, S. boulardii, soil-based probiotic, digestive enzyme with HCl, betaine HCl
- Start/New
- Follow the standard low FODMAP diet now, discontinue low FODMAP with SCD
- After 2 weeks on plan, experiment with fiber for 1.5 weeks
- Finally, try the semi-elemental for 2-4 days (see resources for PDF). If you do not tolerate this version well consider experimenting with the others listed.
- Bring your Taenia solium results to your local doctor and ask them to perform an evaluation/clear you for treatment.
- Follow Up: 4-8 weeks
Visit 4
Lab Interpretation:
- GP’s eval for T. solium
- Negative
Subjective Assessment:
- Better on the standard low FODMAP
- Fiber – no change
- Either the lacto/biff or S. boulardii – rnx constipation
- Low histamine diet – helps neurological symptoms (I had mentioned this as something we could try soon, but Andrew was eager so began a trial on his own accord).
Impression:
- 12/14/16 – Andrew’s general practitioner ruled out T. solium; essentially repeat testing was negative (this is why it’s important not to jump to conclusions based upon antibody testing). Andrew was NR to fiber and suspects one of the probiotics might be causing constipation. Low histamine was very helpful. Today will continue a low histamine and standard low FODMAP diet, modified initial program, then a trial of semi-elemental diet, then finally progress to Habx – using one at a time b/c previous rxns have been noted. If NR, consider prolonged elemental diet or other ddx.
Recommendations:
- Diet/lifestyle
- Take a break for a short walk every 45 minutes to prevent mental fatigue
- Supplemental
- Adrenal: Preg, DHEA
- GI: Soil-based probiotic, digestive enzyme with HCl, betaine HCl.
- Start/New
- Stop the Lacto/Biff and S. boulardii
- Continue with low histamine diet and modified low FODMAP diet
- Stop the fiber
- Perform 2-4 days on the semi-elemental diet before starting antimicrobials
- GI: Habx base protocol with Artemisinin
- *work onto antimicrobials one at a time*
- Follow Up: 5-7 weeks
Visit 5
Subjective Assessment:
- Elemental diet – neuro reaction, flared GI. Caused backslide.
- Habx 1st month (biota-clear 1a, biota-clear 1b) – negative rxn: headaches, indigestion, fatigue, no appetite.
- Really feels like histamine is an issue for him.
- Been off Habx now for 1 week – starting to feel quite a bit better.
- Previous ND had put him on few months of Habx and this helped much of GI SS.
- Now – not quite back to previous high, but getting close
- Improved:
- Sleep, headaches, indigestion, brain fog, tinnitus, joint pain – all SS
- Same:
- na
- Worse:
- na
Impression:
- 1/18/17 – Andrew did not tolerate semi-elemental diet or Habx. He has done very well on low FODMAP/histamine and with the previous program. Since he had treated with Habx with previous ND and seen GI SS improve substantially, I suspect he no longer needs Habx but rather time with low FODMAP/histamine to allow GI to heal and immune/histamine signaling to unwind. We will follow up in a few months and eval if we need to consider revisiting Habx or investigating mast cell triggers.
Recommendations:
- Diet/lifestyle
- Continue with low histamine diet and modified low FODMAP diet
- Take a break for a short walk every 45 minutes to prevent mental fatigue
- Supplemental
- Adrenal: Preg, DHEA
- GI: Soil-based probiotic, digestive enzyme with HCl, betaine HCl.
- Start/New
- Consider an experiment with modified fasting where you skip breakfast and/or lunch.
- Experiment with weaning off items in your program
- Discontinue using elemental diet and antimicrobials
- Follow Up: 2-3 months visit
Visit 6
Subjective Assessment:
- Could not tolerate DHEA & Preg drops; causes stomach burning.
- Feeling about the same as last time.
- Eating more veggies/meat and less rice – more bloating lower GI.
- Eating more rice – upper GI burning.
- Intermittent fasting – causes jittery feeling. Does best with 4 meals/day.
- Craves CHO but has a hard time with many of them.
- Main SS: fatigue, mental endurance, feeling cold, CHO cravings, stomach burning/cramping, bladder discomfort
Impression:
- 3/15/17 – Andrew about the same as last visit and is trying to get back to our peak improvement form Nov 16. He regressed after Habx and elemental diet so will not revisit this. Seems like he may do better with increased CHO intake but this also seems to cause some GI reactions. He also does not do well with fasting. Suggesting prone toward hypoglycemia and metabolic need for carbs but also likely having a degree of CHO malabsorption and histamine intolerance. Today starting increased CHO experiment, then a trial of GI soothing nutrient, then a trial of acid lowering in case this is gastritis (gastritis/hyperacidity appears to be more common in those with histamine intolerance, my estimation). Next, consider histamine lowering agents. Andrew also requested to be tested for heavy metals, which I do not suspect to be an issue but proceeded to order the testing given his curiosity.
Recommendations:
- Diet/Lifestyle
- Continue with low histamine diet and modified low FODMAP diet
- Take a break for a short walk every 45 minutes to prevent mental fatigue
- Supplemental
- Adrenal: see below
- GI: Soil-based probiotic, digestive enzyme with HCl, betaine HCl.
- Start/New
- Increase your carb intake and give this 2 weeks, then
- if this does not help, add in GI repair powder and Vitamin C.
- GI: GI repair powder, Vitamin C
- if this does not help, try to wean off your HCl but stay on the enzyme.
- If this helps then run a trial of the natural acid lowering/stomach repair agent.
- GI: natural acid lowering agent
- Increase your carb intake and give this 2 weeks, then
- Testing
- LabCorp PCO
- Heavy Metals Profile II, Random or 24 Hour Urine
- Heavy Metals Profile II, Blood
- Porphyrins, Quantitative, Random Urine
- LabCorp PCO
- Follow Up: 2-4 months
Visit 7
Subjective Assessment:
- Decreased HCl – helped stomach aches,
- Increasing his CHO content – very helpful.
- Did not start on vitamin C or gut repair powder or acid reducing agent b/c was improved.
- Felt better on the day of DMSA (he took this as a pretest challenge)
- Improved:
- Body temp, bowel movements, stomach aches (burning/cramping), headaches
- Same:
- Fatigue, mental endurance capacity, tinnitus,
- Worse:
- Lower GI cramping, joint aches, metallic taste in mouth
Lab Interpretation:
- LabCorp PCO
- heavy metals and porphyrins – wnl
- Quest Outside Labs (requested by another doctor)
- H: BUN, AST, **ALT
- Dx:
- 4/26/17: liver damage/inflammation
- 11/11/16: potential T. solium, E. nana. H Ferritin, mild mixed proximal SIBO.
- Summary
- Heavy metal toxicity or tissue burden does not appear to be an issue
- Liver inflammation noted
Impression:
- 4/26/17 – Increasing CHO and decreasing HCl has helped. Today will move forward with vitamin C and GI repair powder to attempt to further lower HI, and start on a liver support supplement. Will then start acid lowering agent to assess if gastritis is a factor. Will also retest CMP/CBC to eval elevated liver enzymes and reassess ferritin/iron overload. Additionally, will run CIRS/mold screen through life extensions. He noted he felt better on the day of DMSA so consider detox therapy soon. Other end-phase considerations: retesting SIBO, FMT or Helminths.
Recommendations:
- Diet/Lifestyle
- continue with low histamine diet and modified low FODMAP diet
- take a break for a short walk every 45 minutes to prevent mental fatigue
- Supplemental
- Adrenal: Preg, DHEA
- GI: Soil-based probiotic, digestive enzyme with HCl, betaine HCl.
- Start/New
- start on new GI support items now. You can stagger start if you wish to isolate for effect.
- GI: GI repair powder, Vitamin C, acid lowering agent, liver support.
- Perform testing now
- Testing
- LabCorp
- Life Extension Panels
- Follow Up: 2 weeks after collecting lab testing
Visit 8
Subjective Assessment:
- Liver support – helps GI.
- GI support powder, Vitamin C, acid lowering agent – has not started.
- Improved:
- GI: indigestion, burning, cramping.
- Same:
- Neuro; brain fog, fatigue, HA, tinitus.
- Worse:
- na
Lab Interpretation:
- Just passed online visual acuity test (failing is suggestive of mold/CIRS)
- Life Extension Panels
- Dx
- Suggestions of mold/CIRS and renal disease
Impression:
- Key Point: Why did I start down the path of pursuing mold? Seeing Andrew’s GI improve with no corresponding improvement in his neurological symptoms is suggestive there may be more than a GI issue present. It’s important to wait and see if someone’s neurological symptoms will trail behind improvements in the GI (so don’t rush to mold or other ddx) but if you have waited a couple months and seen the GI maintain improvements with no improvement neurologically, it could be time to consider other ddx.
- 5/17/17 – Lab pattern is consistent with renal disease, referring to PCP now. This might be driving high ferritin also. Mold/biotoxin appears to show genetic predisposition and immune activation, which might be driving renal findings. Will start with CIRS protocol non-rx, then consider adding previously recommended GI support. Will also perform Ermi testing now (see results below), VCS testing and take 2 weeks out of the home. Also advised to see a mold/CIRS specialist.
Recommendations:
- Start/New
- See your local primary care provider immediately for renal evaluation
- Consult with a mold and/or CIRS specialist
Dr. Ruscio’s Comments
We followed up with Andrew 6 months later to check in and he commented that he was very appreciative of our office helping him identify mold as an issue, that he has been working with a specialist in the treatment of mold (and Lyme) and progressing nicely. His PCP had also ruled out renal disease, thankfully.
Andrew’s case is a good example of when there is a need to address more than the GI and consider other diagnoses/causes. This is also another reason I am not a proponent of high amounts of testing. How does this relate? Too much testing can make it hard to get a sense of what a typical treatment response looks like because you are distracted by a litany of testing variables. However, when you do understand what a typical response looks like, you can then identify when someone’s response is abnormal. Once you identify this abnormality and determine that the response is not an anomaly (its happened repeatedly), it is then a good idea to consider other differentials and move the patient in the most substantiated direction. If this direction is one you are not well versed in, refer out. Don’t try to do everything, patients appreciate when you respect your own limitations.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine









Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!