Practitioner Case Study – March 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Leptin in Autoimmune Diseases
- Clinical Trial: the Combination of Rifaximin With Partially Hydrolysed Guar Gum Is More Effective Than Rifaximin Alone in Eradicating Small Intestinal Bacterial Overgrowth
- Autoimmunity Affects Health-Related Quality of Life in Patients With Hashimoto’s Thyroiditis
- Bacillus as Potential Probiotics: Status, Concerns, and Future Perspectives
Practitioner Question of the Month
Practice Tip
Case Study
Digestive Enzyme Causing What Looked Like SIBO, Complete Resolution After Avoiding Enzymes And Using Iodine And Female Hormone Support
Patient Info:
- Catherine, 35yo female
- Previous Dx
- SIBO. Low T3. Low Ferritin.
- Rx
- Nature-Throid -Low T3, LDN-SIBO, B12 injection- energy/MTHFR, Bio-Identical Progesterone – Low Progest.
- Chief complaints
- Diarrhea, 7-INT
- Gas/Bloating, 8-CO
- Hair loss, 8-INT
- Fatigue, 6-CO
- Brain Fog, 5-INT
- Joint Pain, 4-INT
- Other symptoms
- female: thinning hair, painful periods, GI, heavy flow
- anxiety, mood swings
- fibrocystic breast-like symptoms
Visit 1 (day 1) – History and Exam:
Initial Impression
- Catherine presents as a generally healthy 35yo female with a good diet, lifestyle (but exercise is limited by illness) and outlook on her health.
- She has been dx with SIBO, previously treated with Rifax followed by Habx and responded well but then relapsed. A low FODMAP/AIP diet has also been helpful, as have been enzymes.
- I suspect she merely needs more follow up/through in her care and she will do quite well, and that GI is main underlying driver of sequela
- There are some other dx to mind though, adhesions, hormones… see list:
- SIBO, PI
- Vinc/cdtB ab
- SIFO, H2S SIBO
- Dysbiosis
- GI infection
- Female hormone imbalance
- Fibrocystic breast
- Histamine intolerance
- Ulcer, gastritis, high HCl
- APCA
- Abdom/pelvic adhesions
- RA
- Semi-sedentary
- IBD
- Prognosis good to excellent.
Previous Diets
- Low FODMAP – helps GI. AIP – helps brain fog/joint pain. Fasting – does not do well.
Previous Treatments
- Nature-Throid – slightly helpful. Rifaximin followed w/ Habx – improved greatly, then relapsed. Progest – helps moods/cycles. B12 – helped E. LDN – tolerate, MR. HCl – MR. Enzymes/bile – helps GI.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests ordered
- Aerodiagnostics Lactulose SIBO breath test
- Doctors Data Comp. Stool w/ Para 3x stool test
- Quest – IBS check
- LabCorp – Full wellness panel
- LabCorp – Full GI panel
- Rationale
- Given her digestive symptoms ordering a full GI workup for dysbiosis is warranted
- Testing for vinculin and CdtB antibodies can rule out IBD as the cause of diarrhea
- The wellness panel will screen for anemias and for hypothyroidism, among other things
Recommendations
- Please perform the Modified Fast for 2-4 days (see website for PDF), then
- Continue with your previous diet of AIP and personalized low FODMAP
- NRT: Iodine, Multi, Vit D/K, Omega 3,6,9 blend
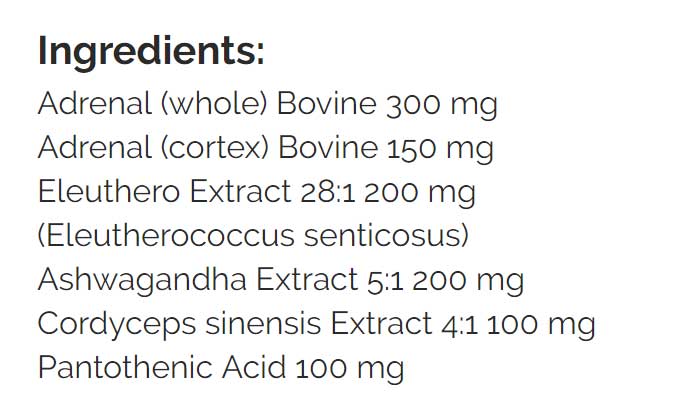
- Adrenal: Adrenal Support formula
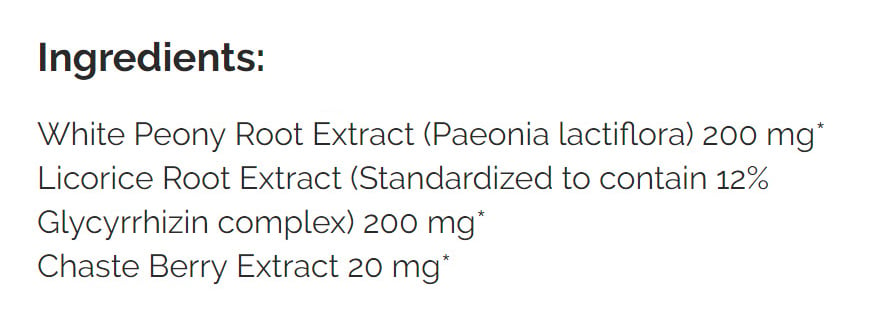
- Female: Herbal progesterone support
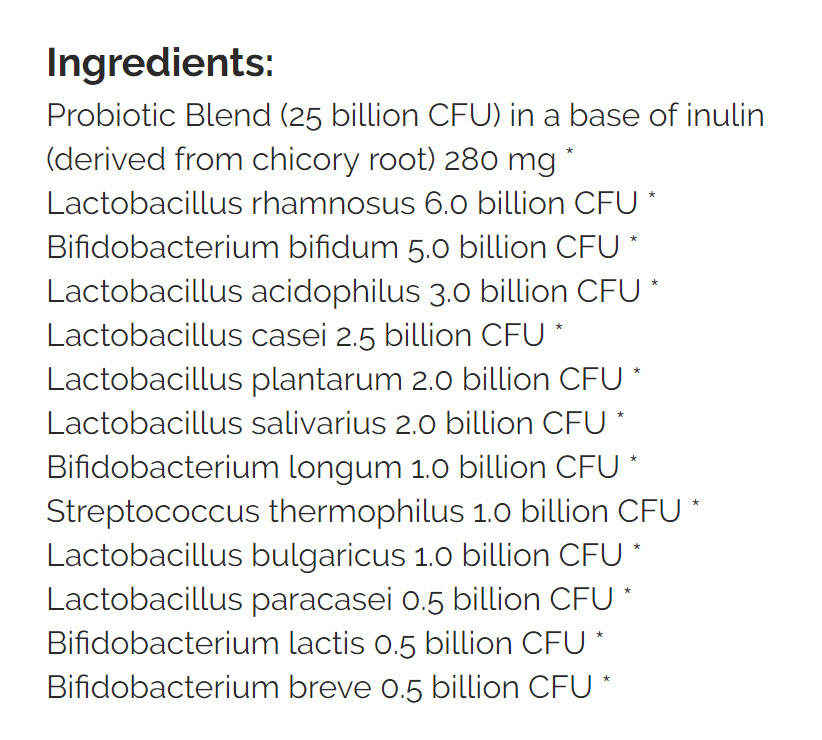
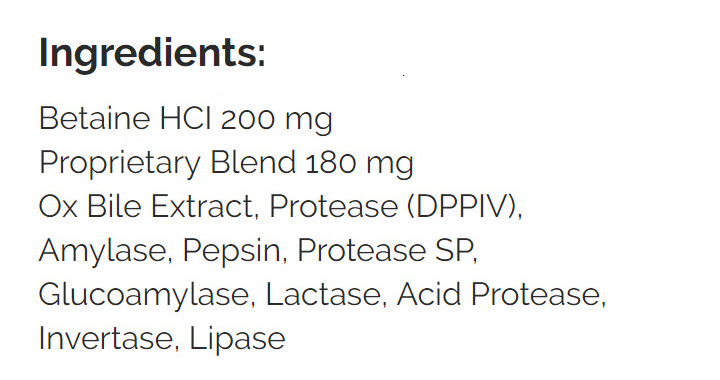
- GI: Lacto/Bifido probios blend, S. boulardii and digestive enzyme
- Rationale
- Fasting will evaluate if she might do well on IF and if foods are driving symptoms
- Iodine and female hormone herbs may balance hormone causing fibrocystic-like breast symptoms and general female hormone-mediated symptoms
- Probiotics and enzyme may improve GI symptoms
Visit 3 – Lab Interpretation and Treatment Evaluation
Lab Interpretation:
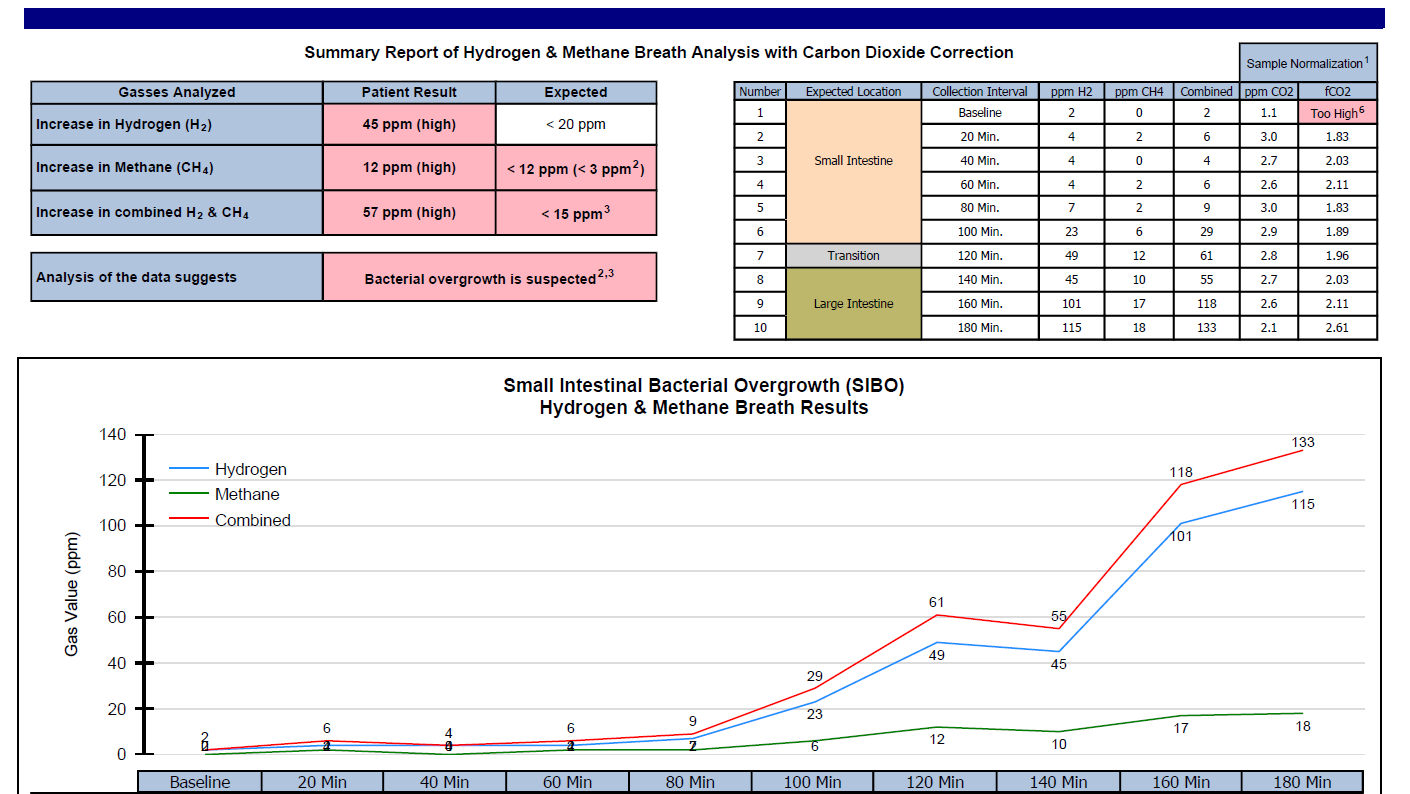
- Aerodiagnostics Lactulose SIBO breath test
- H2 23, CH4 6
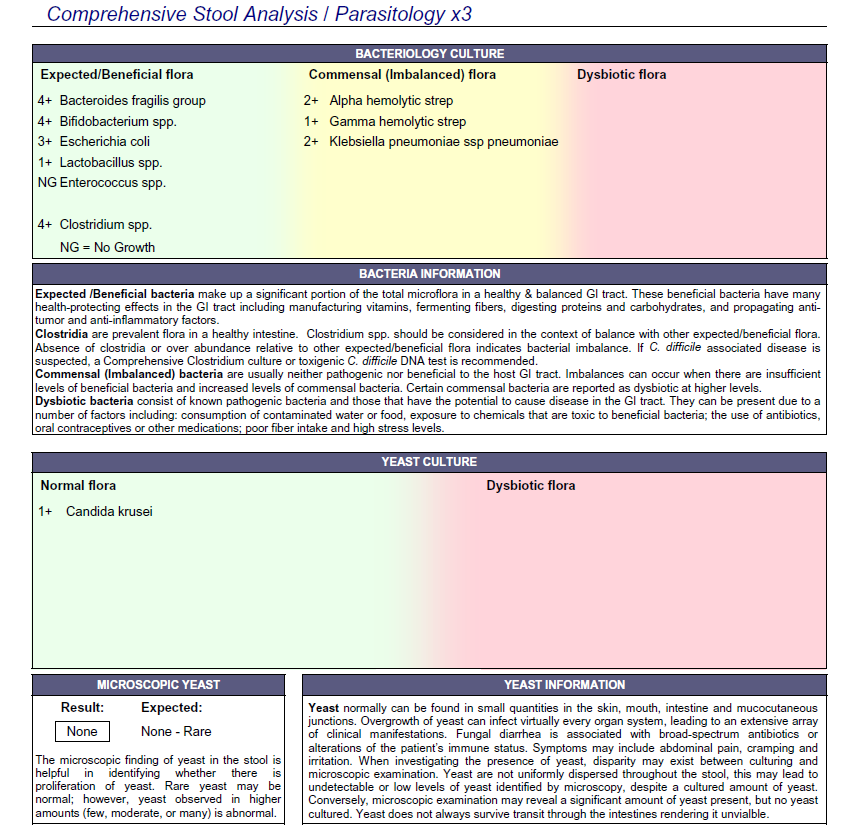
- Doctors Data Comp. Stool w/ Para 3x stool test
- Bact: commensal dysbiosis.
- Yeast: normal Candida krusei +1. RBC OnP 1x.
- LabCorp #1 blood, urine, stool & breath
- parietal cell ABs (APCA) 51-H
- Inflammatory Bowel Disease (IBD) Expanded Profile; ACCA, ALCA, AMCA, gASCA, pANCA. ACCA 220-H
- LabCorp #2 blood & urine
- UA- abnormal WBC Ketones
- Vit D 50.1-WNL
- IBS check- Through Quest
- CdtB 1.65-H, Vinculin – WNL
- Dx
- v. mild H2 SIBO. DD: mild bact/yeast dysbiosis. LC: APCA. IBSDetex: CdtB abs.
- Summary
- Essentially we found borderline positive SIBO and commensal dysbiosis. The overgrowth of commensals via stool testing is something I interpret with caution as the meaning of this is unclear.
- We found antibodies against her parietal cells (in the stomach) and the autoimmunity that underlies SIBO (CdtB antibodies).
Subjective Assessment:
- MF (broth, 2 days) – felt very weak and hungry, but body aches and GI SS gone.
- Initial program (on for 4 days) – energy improved.
- Ox bile – caused diarrhea.
- Overall today is better
- Improved:
- gain weight, fatigue, diarrhea. Gas/bloating, joint pain (still present).
- Same:
- Brain fog. Hair loss. Female. Fibro-breast.
- Worse:
- na
Impression:
- Catherine has been dx with SIBO, previously treated with Rifax followed by Habx and responded well but then relapsed. A low FODMAP/AIP diet has also been helpful, as have been enzymes. She may simply require a more thorough plan with follow up. Today’s +IBSDetex may indicate post-antimicrobial prokinetic – important. Labs today also show SIBO, bact/fung dysbiosis, and APCA. Her GI/joints responded well to MF but she was tired/weak. The initial program might be helping. Mind ddx if NR. Today; maintain current program and continuing B12 and LDN from the local doc. FU in 1-3 months wean off T3 and perform dietary reintro or treat SIBO/dysbiosis if indicated.
- Key point: How did she notice ox bile caused diarrhea? She had been taking supplemental bile historically, BUT I ask all patients to come off previous supplements when starting care. This is for a few reasons, one is because sometimes people are taking things they are reacting to but are unaware they are doing so. This ‘supplement holiday’ was a key aspect of pinpointing the root cause of her diarrhea.
Recommendations:
- Continue current plan
- Start on vitamin B12 weekly until stomach antibodies are normal, then revert to once monthly
- Keep up the good work!
- fu: 1-3 months
Visit 4
Subjective Assessment:
- Had a miscarriage recently, has a history of infertility
- Is doing “so much better”
- Digestive enzyme – rnxs, highly intolerant to bile
- Iodine – very helpful for fibro-breast. Progesterone balancing herbs – appear helpful
- Improved:
- gain weight (114), fatigue, diarrhea. Gas/bloating, joint pain (still present). Female. Fibro-breast. Brain fog.
- Same:
- Hair loss.
- Worse:
- na
Impression:
- Today Catherine is doing great and has experienced marked improvements in all CC (except hair loss). She is very happy. Is very reactive to bile, can’t even tolerate a small amount. Iodine and female hormone balancing herbs are helping fibro breasts. Got pregnant, which she hasn’t been able to do previously, but did have a miscarriage. We will maintain current program, then fu in 2 months and move to curtail program and broaden diet. Will also have her speak with prescribing provider about weaning off thyroid Rx, and speak with ClearPassage for fertility consult. Her miscarriage was disappointing but it is also an improvement relative to where she was. Her body may simply need more time before it can maintain a successful pregnancy.
Recommendations:
- Continue previously plan
- Have a consultation with ClearPassage regarding infertility
- Speak with your doctor about coming off thyroid hormone
- Keep up the good work!
- Avoid digestive enzyme with any bile
- fu: 2 months
Dr. Ruscio’s Comments
Catherine’s case offers a few important lessons.
1. Not all lab findings require treatment.
This was evidenced by the positive CdtB antibodies that did not require prokinetic therapy or cause her to experience a SIBO relapse. It is further supported by the ‘dysbiosis’ found on the stool profiles, that appear inconsequential.
2. Sometimes less is more.
While alternative medicine loves to use ‘digestive enzymes’ there is a time when these can cause reactions. Most namely bile can cause diarrhea, and HCl can cause stomach pain, nausea, bloating and gastritis.
3. Reading someone’s symptoms and the response is paramount.
The two keys to success with this case were predominantly observational and not based on objective lab data. They were a) the reaction to bile and b) the female hormone symptoms. This is important for clinicians to understand because patients will often come in viewing their illness through the lens of whatever predominates current discussions in healthcare. Right now, this is often SIBO, so patients will present with a SIBO-centric perspective. It is important for clinicians to be able to see through this and to what the true underlying cause is.
If the lab data here was used to guide treatment, without adequate consideration of the subjective picture, this would have unquestionably lead to overtreatment and poor results.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!