Practitioner Case Study – June 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Combination L-T3 and L-T4 Therapy for Hypothyroidism
- A Critical Appraisal of the Recent Reports on Sunbeds from the European Commission’s Scientific Committee on Health, Environmental and Emerging Risks and from the World Health Organization
- Elemental Diet and the Nutritional Treatment of Crohn’s Disease
- Rapid-Fire Research – Ultra-Concise Summaries of Noteworthy Studies
- Positive effects of resistant starch supplementation on bowel function in healthy adults: a systematic review and meta-analysis of randomized controlled trials
- Lubiprostone accelerates intestinal transit and alleviates small intestinal bacterial overgrowth (SIBO) in patients with chronic constipation
- Is thyroid autoimmunity itself associated with psychological well-being in euthyroid Hashimoto’s thyroiditis?
- Selenium supplementation could restore euthyroidism in subclinical hypothyroid patients with autoimmune thyroiditis
- Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Kim, 57yo, female
- Previous Dx
- Euthyroid Hashimoto’s
- Rx
- Lisinopril 5 mg/day-HBP
- Tirosint 63 mcg/day-Hashimoto’s
- Buspar 15 mg/day-Anxiety
- Chief complaints
- Constipation (3BM/wk), Hard/Compact, 10-IN
- Bloating, 5-IN
- Fatigue, 7
- Insomnia, 5
- Other signs and symptoms
- Allostatic load, mod – fatigue, fasting, sleep, cravings,
- Female, mild/mod – vag dryness, low libido, hot flash
Visit 1 (Day 1) – History and Exam:
Initial Impression
- Kim presents as a 57yo female with a paleo low FODMAP-like diet, with a good lifestyle and demeanor but who is overly involved and worried about her health. Fearful of foods, frustrated and the same applied to her TPO abs.
- She has been Dx euthyroid Hashimoto’s and sleep apnea. Is using CPAP, and is on Lisinopril 5 mg/day-HBP, Tirosint 63 mcg/day-Hashimoto’s, Buspar 15mg/day-Anxiety.
- Previous testing has found
- Diagnostic Solutions: C. diff. SIBO: H2 17, CH4 13 Bloods: TPO hover in thousands
- Onset:
- CCs started after 4x Abx for a sinus infection
- Her symptoms have improved from AIP, LF (autoimmune paleo, low FODMAP) and especially from gluten-free. Tirosint also helpful. Miralax was much more helpful than Mg/C but came off due to CBC findings. Thyroid Abs non-responsive to diet nor selenium, vitamin D.
- Kim has not treated GI dysbiosis (formerly found) other than with diet, probiotics, and fermented foods. She may do well from further treatment; namely Habx. She may also simply require a different method of constipation support; Miralax. Her MD upped the dose of Tirosint to help lower her historically high TPO abs, however, this might be causing fatigue.
- Diets are creating fear and resentment, appears to be following them too strictly. Has been on Buspar for a long time, however, she might not need this any longer with improving diet. May also have histamine intolerance, but careful with more dietary restrictions. Or, abdominal-pelvic adhesion and/or dyssynergic constipation are also possible.
- Since she has not done much for GI has much potential, especially if she simply needs Habx, broader diet, and low dose Miralax. Prognosis good to excellent.
Previous Diets
- Low FODMAP – helps constipation, bloating but feels too restrictive. AIP – very helpful, especially joints but depressed because she missed food. GF – improved joint pain.
Previous Treatments
- Tirosint – helps fatigue. Miralax (osm. lax) – helps constipation. Sleep apnea (CPAP) – helpful. Mg w vit. C – helps but not as much as Miralax. Buspar (anxiety) – helpful. Se and vit. D – did not improve thyroid Abs.
Visit 2 (A Few Days Later) – Testing and Initial Recommendations
Testing
- Tests ordered
- Aero Lactulose SIBO breath test
- BioHealth 401H stool test
- LabCorp #2 – see markers at next visit
- basics, additions
- fT3 dialysis/LCMS
- LabCorp #1 blood, stool, breath -– see markers at next visit
- full GI
- Rationale
- Given her digestive symptoms, a GI eval is warranted (SIBO, BioHealth, and LabCorp)
- Because I am suspicious that she either does not need thyroid Rx or is overdosed, I am ordering the more sensitive dialysis/LCMS testing for free T3
Recommendations
- Diet
- Please follow a loose paleo diet. Only avoid foods you have noticed do not agree with you. Experiment with nuts, beans/legumes, gluten-free grains and high FODMAP foods.
- Please do not follow the results of your Cyrex test, as we will work to broaden your diet.
- Please eat every 3-4 hours, most of the time.
- Lifestyle
- na
- Treatment
- Please be on the diet for 2 weeks before adding in the supplements, but continue diet until our follow up. Then be on the supplements for 3 weeks before following up. Please make a note of the change you noticed from diet versus supplements.
- First, perform a 4 day trial on peppermint. Then start on the rest of your program.
- Nutrient support:
- vitamin D/K, fish oil blend
- Adrenal:
- Preg, DHEA
- GI:
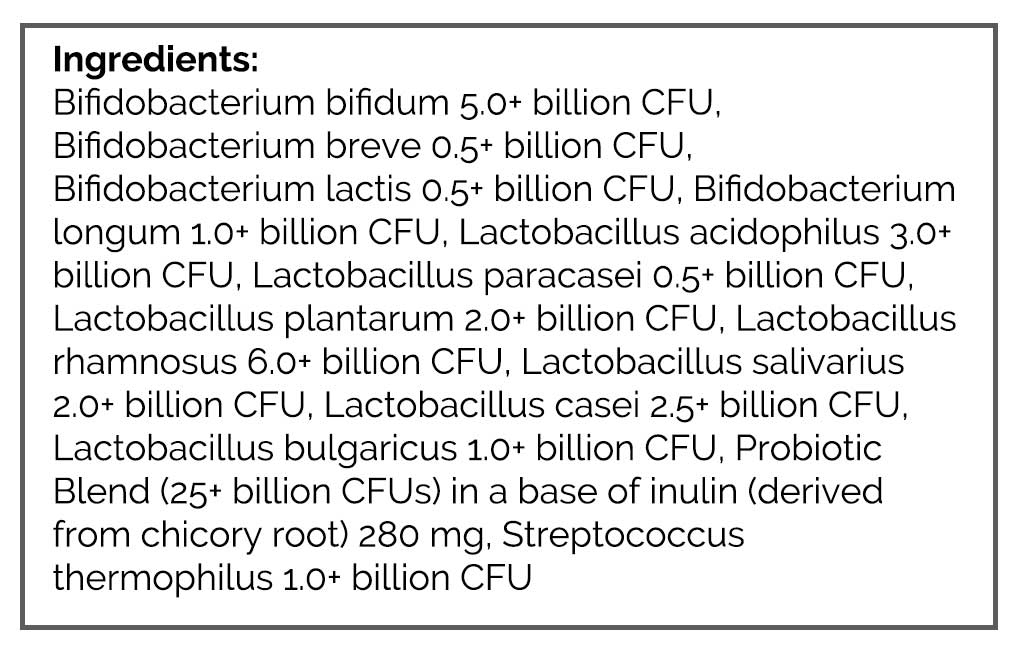
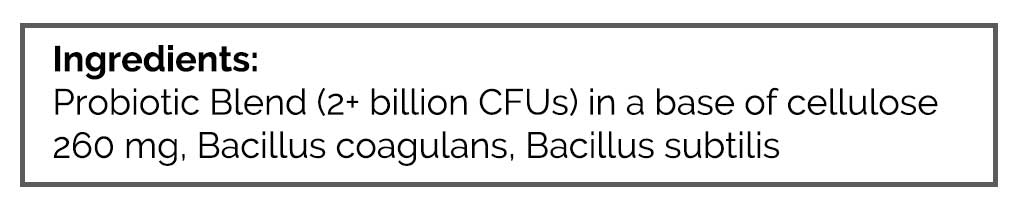
- Lacto-Bif probiotic, Soil-based probiotic, S. boulardii (all 1x/day).
- Fiber, Mag Citrate + Vitamin C and Miralax.
- Work to find the minimum dose of Miralax.
- FU: 6-7 weeks
- Rationale
- Kim was far too restrictive with her diet, so we advised her NOT to regard her food allergy testing and to work to broaden her diet.
- We also used frequent meals to stabilize blood sugar
- All 3 categories of probiotics were used, plus laxative and adrenal support
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Peppermint – no change
- Probiotics – helped bowels markedly
- Fiber – might constipate
- Eating more – feels good, makes her happy
- Decreased Tirosint dose – felt fine
- Overall “feels really good”
Lab Interpretation:
- Aero Lactulose SIBO breath test
- H2 15, CH4 2
- BioHealth 401H stool test
- Normal
- LabCorp #1 blood, stool, breath
- Normal
- LabCorp #2 blood & urine *Fasting
- UA -Abnormal, RT3 28.3-H
- Dx
- No diagnosis, high reverse T3 noted.
- Summary
- The high rT3 may be due to unneeded thyroid Rx but is not concerning at the moment.
Impression:
- Today Kim has done great from eating more, taking less and enjoying her life. Probios and Preg/DHEA very helpful for GI and energy. Fiber might constipate. Peppermint – no change. Also able to decrease Tirosint. Today labs are generally UR. Will continue with the current plan, sans peppermint, and then fu in 6 weeks to do program wean.
Recommendations:
- Continue previous recommendations.
- Starting
- Stop peppermint now
- Keep up the good work
- FU: 6 weeks
Dr. Ruscio’s Comments
This case is a strong illustration of how important it is to identify patients who have gone overboard with health research and are inadvertently making themselves sick. Kim could have very easily been pulled deeper into the ‘sickness’ mentality. In fact, our first visit was a bit tense because ‘she was expecting more after seeing an expert’. She was a bit let down that I did not advise digging deep into further testing or provide more elaborate treatment recommendations. She was expecting this due to her functional medicine programming.
Kim noted that she was feeling better than she had in several years, after taking less medication and broadening her diet. If I had said ‘she had SIBO’ due to her methane of 4, or a thyroid problem due to her high reverse T3, I would have been doing her a huge disservice. She had the tendency to expect the worst and for her path to be challenging, however, Kim was much healthier than she realized. The ‘treatment’ she needed was a responsible narrative regarding her health, her labs and a treatment program that alleviated the unnecessary burden dietary restrictions plus provided a small degree of support.
Don’t miss these cases. They will not respond to more treatment, because they do not require it. You will save them much time, money and heartache if you can identify this out of the gate.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!