Practitioner Case Study – July 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- The prevalence, incidence and natural course of positive antithyroperoxidase antibodies in a population-based study: Tehran Thyroid Study
- A concise review of Hashimoto thyroiditis (HT) and the importance of iodine, selenium, vitamin D and gluten on the autoimmunity and dietary management of HT patients. Points that need more investigation
- Effect of free triiodothyronine concentration on the quality of life of patients treated with levothyroxine
- Rapid-Fire Research – ultra-concise summaries of noteworthy studies
- N-acetylcysteine as a powerful molecule to destroy bacterial biofilms: A systematic review.
- Female hormones influence the vaginal microbiota.
- Functional 13C-urea and glucose hydrogen/methane breath tests reveal a significant association of small intestinal bacterial overgrowth in individuals with active Helicobacter pylori infection.
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Janet, 57yo female
- Previous Dx
- Chronic combination SIBO. IBS check +, very high vinculin abs.
- Rx
- Coreg 12.5 mg qd – Cardiomyopathy, Rifaximin (daily) 200 mg qd – SIBO, Imuran 50 mg qd – SIBO, Zenpep – SIBO
- Chief Complaints
- Nausea, 7-CO
- Intestinal Spasms, 5-INT
- Fatigue, 7-CO
- Achiness/ Flu-Like Symptoms, 6-INT
- Bloating & Burping, 3-CO
- Urgent Bladder, 5-INT
- Other symptoms
- Underweight
- Insomnia
Visit 1 (Day 1) – History and Exam
Initial Impression
- Janet presents as a 57yo female with a good diet, lifestyle, support structure and outlook on her health.
- She has a history of cardiac issues and cannot use prokinetic Rxs. She has been struggling with her CCs for several years with no known trigger.
- Has been Dx and treated for SIBO. Rifaximin helps but then regresses. Habx appear most helpful. Diet helps but she is very restricted now, cannot reintroduce and this is a problem as she is underweight.
- Has been treated by Pimentel and is now on Imuran as a treatment for very high Vinculin abs. However, says better SS improvement with Dr. Keller recommendation of Allicillin and ParaBiotic. Ginger also helpful.
- I anticipate she will do well with our standard GI care and may need: semi-elemental diet (to help in weight gain and gut healing), low dose cyclical Habx, probiotics, fungal treatment.
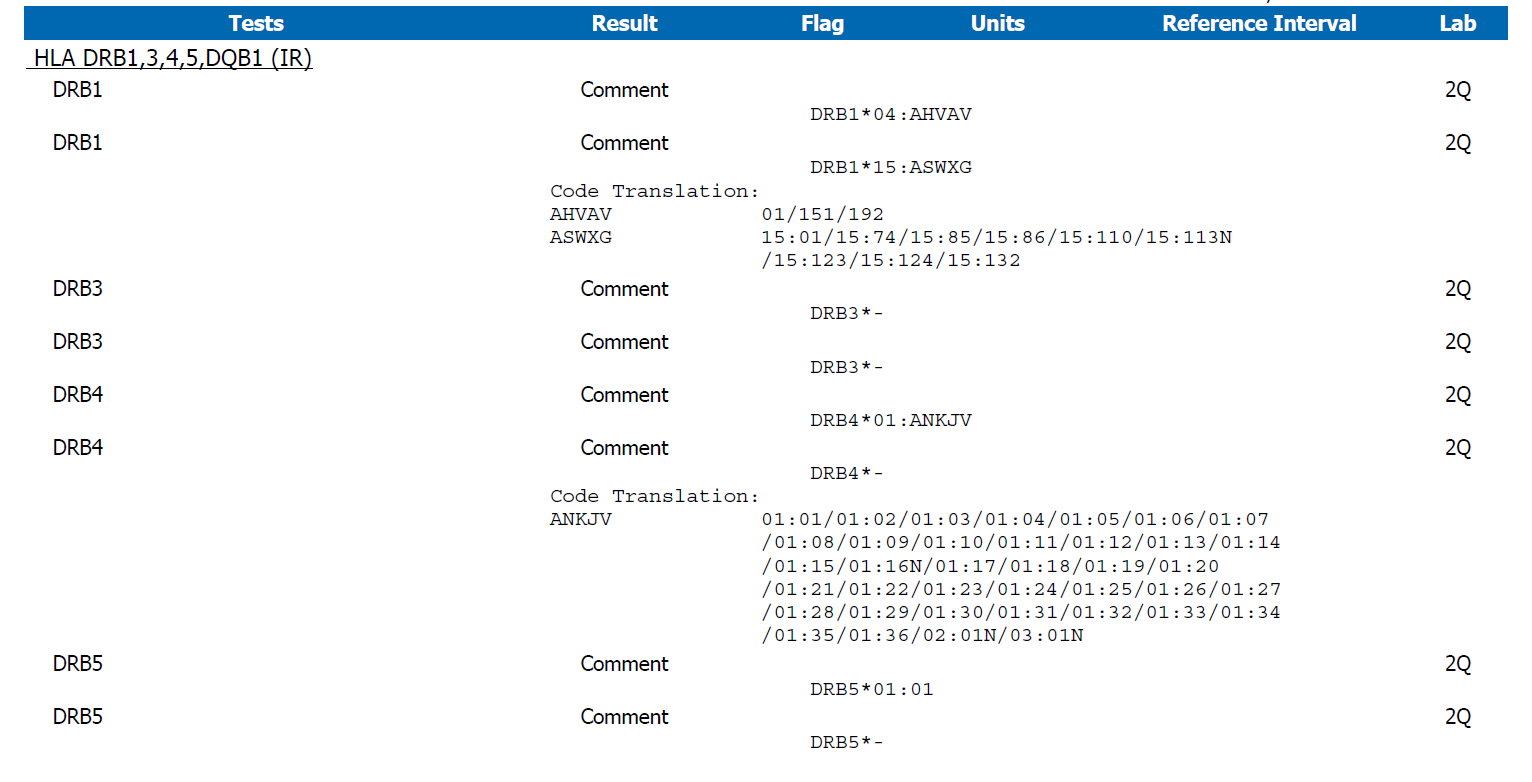
- She has a strong history suggestive of CIRS and perhaps this is what is driving her high levels of Vinculin AI? Will perform testing.
- Other Ddx possible but not highly probable. Will try HCl again for nausea, consider adhesions, histamine intolerance and gastritis if non-responsive.
- Prognosis fair to good.
- Previous testing:
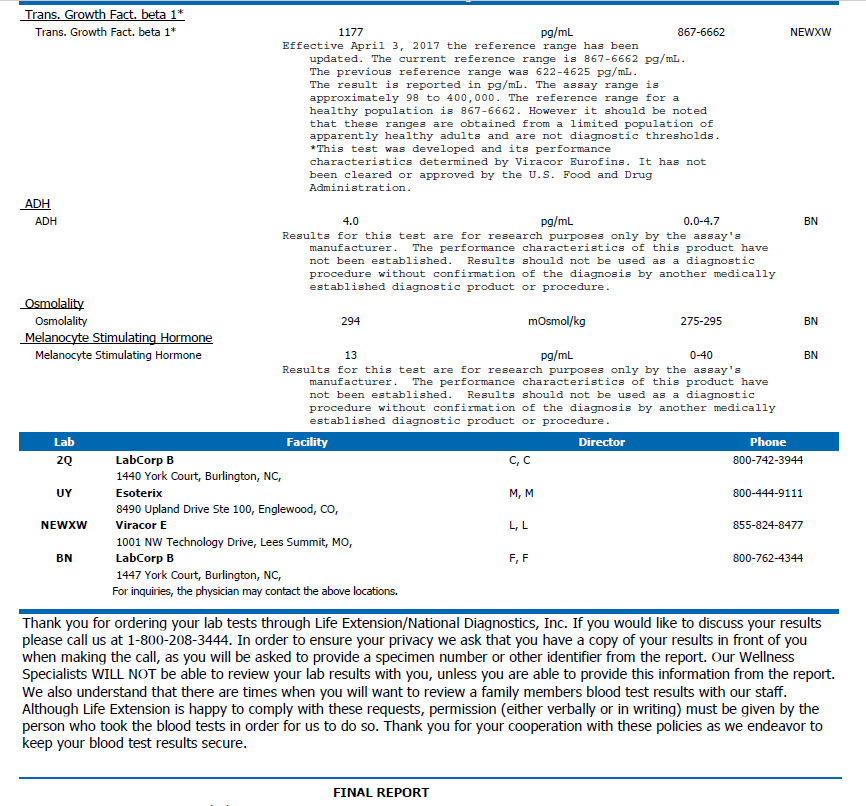
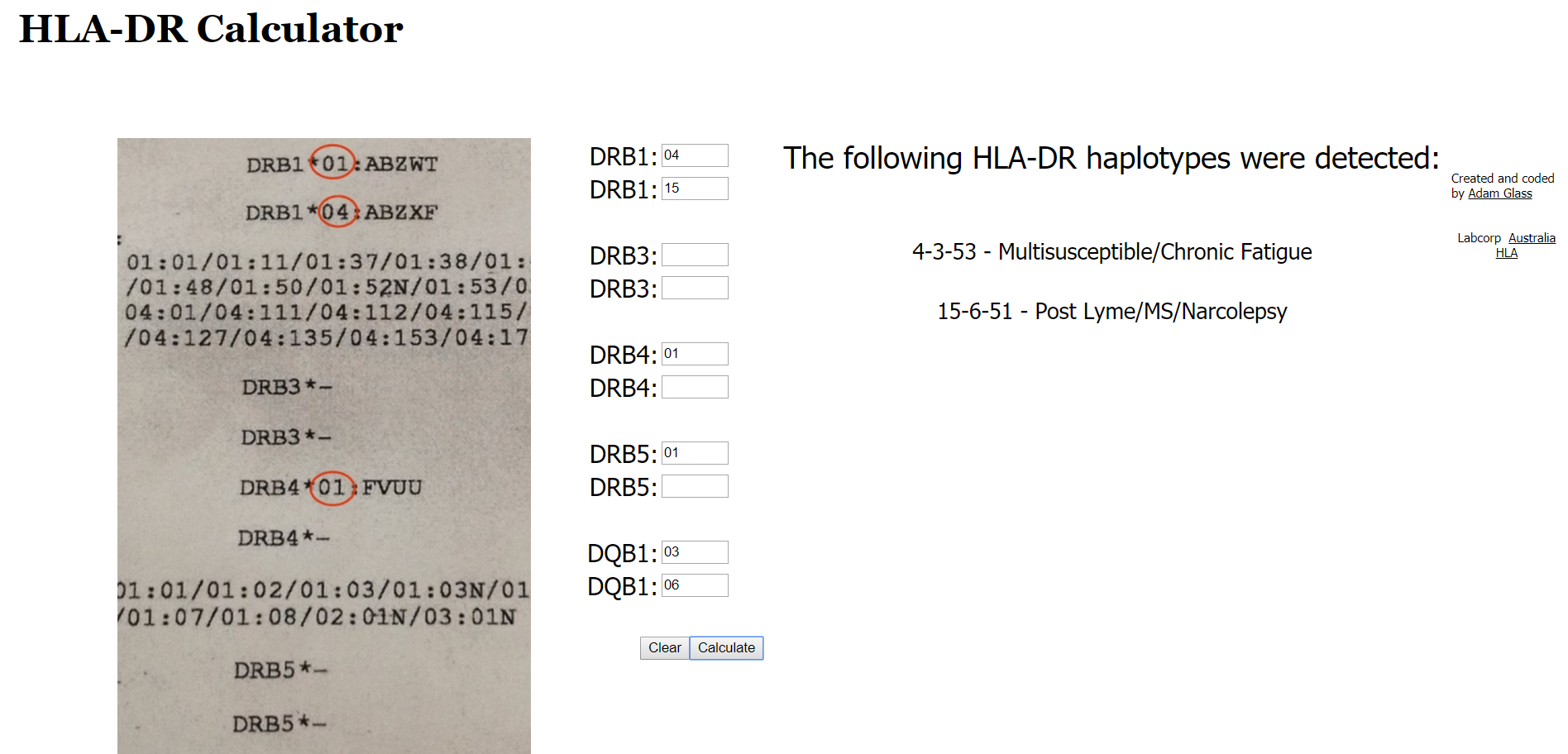
- SIBO. IBS check + CdtB, Vinculin. Colon/endo – wnl. “Dreaded CIRS genome and high TGFb H”.
- Prior treatments:
- Ginger – helps nausea. Allicillin – helpful. ParaBiotic – helps. Rifaximin – helped then regressed. Imuran – not sure. Enzymes (Zenpep) – MR. HCl – aggravates bladder.
- Starches – nausea. SIBO diet or Paleo diet – helps symptoms but causes weight loss. Fasting – feels better.
- Notes/DDX
- SIBO (PI)
- H2S SIBO, SIFO
- Dysbiosis
- GI infection
- CdtB/Vinculin Abs
- APCA
- CIRS** highly supported
- Histamine intolerant
- Gastritis, ulcers, high HCl
- Abdominal pelvic adhesions *not highly supported*
- Semi-sedentary
Visit 2 (A few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Doctors Data Comprehensive Parasitology 3x stool test
- LabCorp #1 – full GI workup
- LabCorp #2 – comprehensive blood/urine testing
- Quest – IBSDetex
- Life Extensions mold panel – Life Extension Mold & Biotoxin Panel
- Rationale:
- Retest SIBO. Test for other GI dysbiosis/infection. Perform comprehensive blood chemistry for any previously unidentified imbalances, and to screen for anemia.
- Reassess anti-vinculin/CdtB antibodies. Check for mold/biotoxins.
Recommendations
- Dietary
- Please continue with your previous paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Experiment with intermittent fasting; 2 larger meals a day instead of 3 meals a day.
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- NRT: vitamin D/K
- GI:
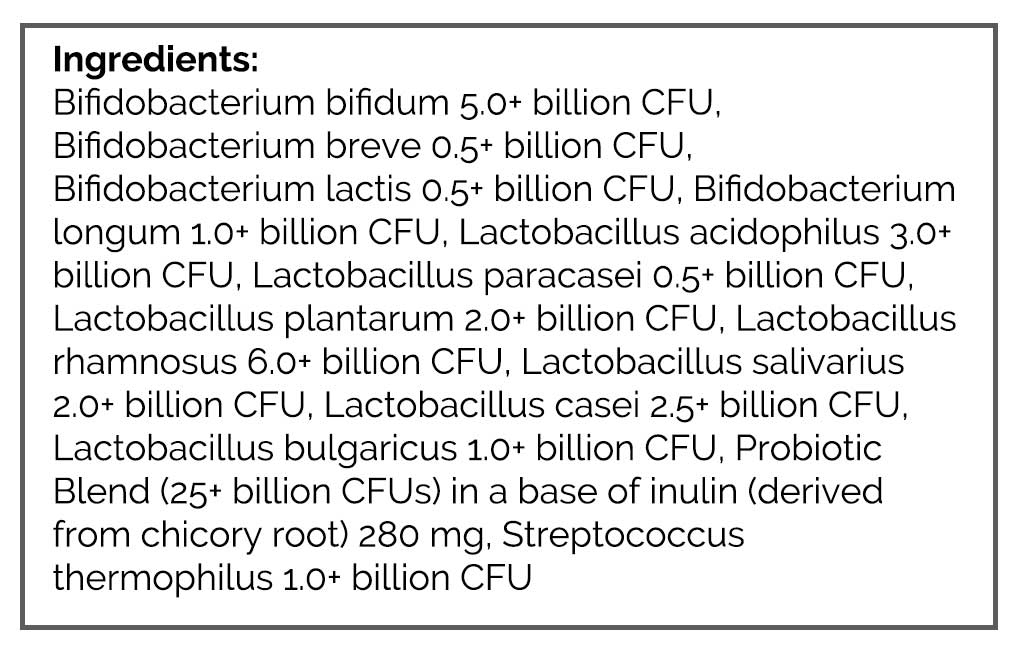
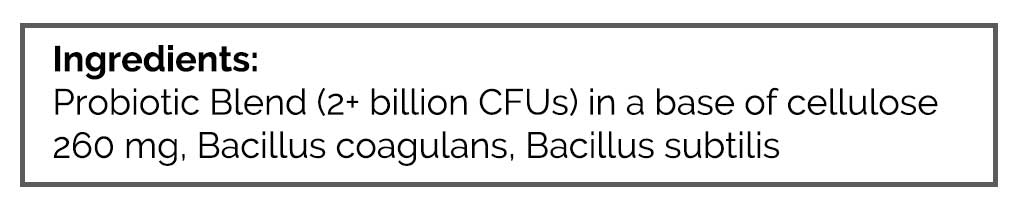
- Lacto-Biff blend, S. boulardii, and soil-based probiotic formula
- Liver-gallbladder support formula
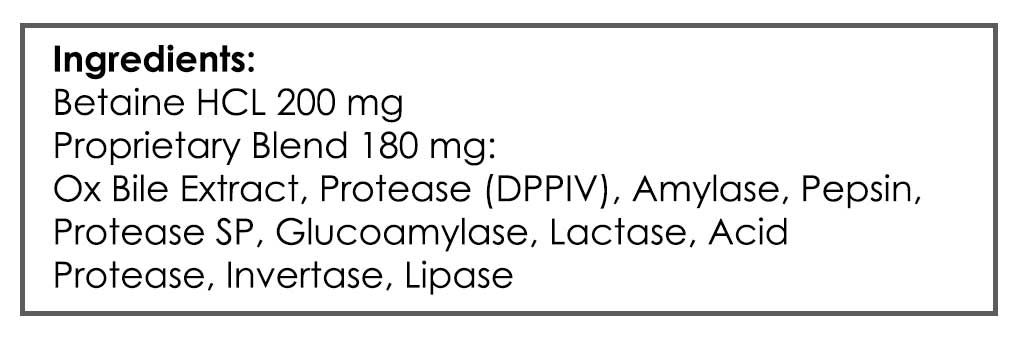
- Betaine HCl
- Be on the probiotics for 1.5 weeks before starting the Betaine HCl
- Rationale
- Fast Tract Diet may allow her to discover additional safe carb sources
- Periodic intermittent fasting may help with GI healing
- Some activity is needed
- Vitamin D can help with autoimmunity and IBS
- Probiotics can be anti-SIBO and improve GI health globally
- Liver support may help with liver damage caused by Imuran
- A tolerable dose of HCl may help with any malabsorption, which she exhibits signs of due to weight loss. Since she reacts to this, we want to start it in isolation.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment
- Overall about the same.
- Tried FTD (Fast Tract Diet) score to increase CHO and did not help.
- Intermittent fasting – helpful.
- Lacto-Biff probiotic – rxn. S. boulardii – thinks might help. Soil-based – has not tried.
- Has not tried – HCl or liver-gallbladder support.
- Imuran appears to be slightly decreasing IBS check results.
Lab Interpretation
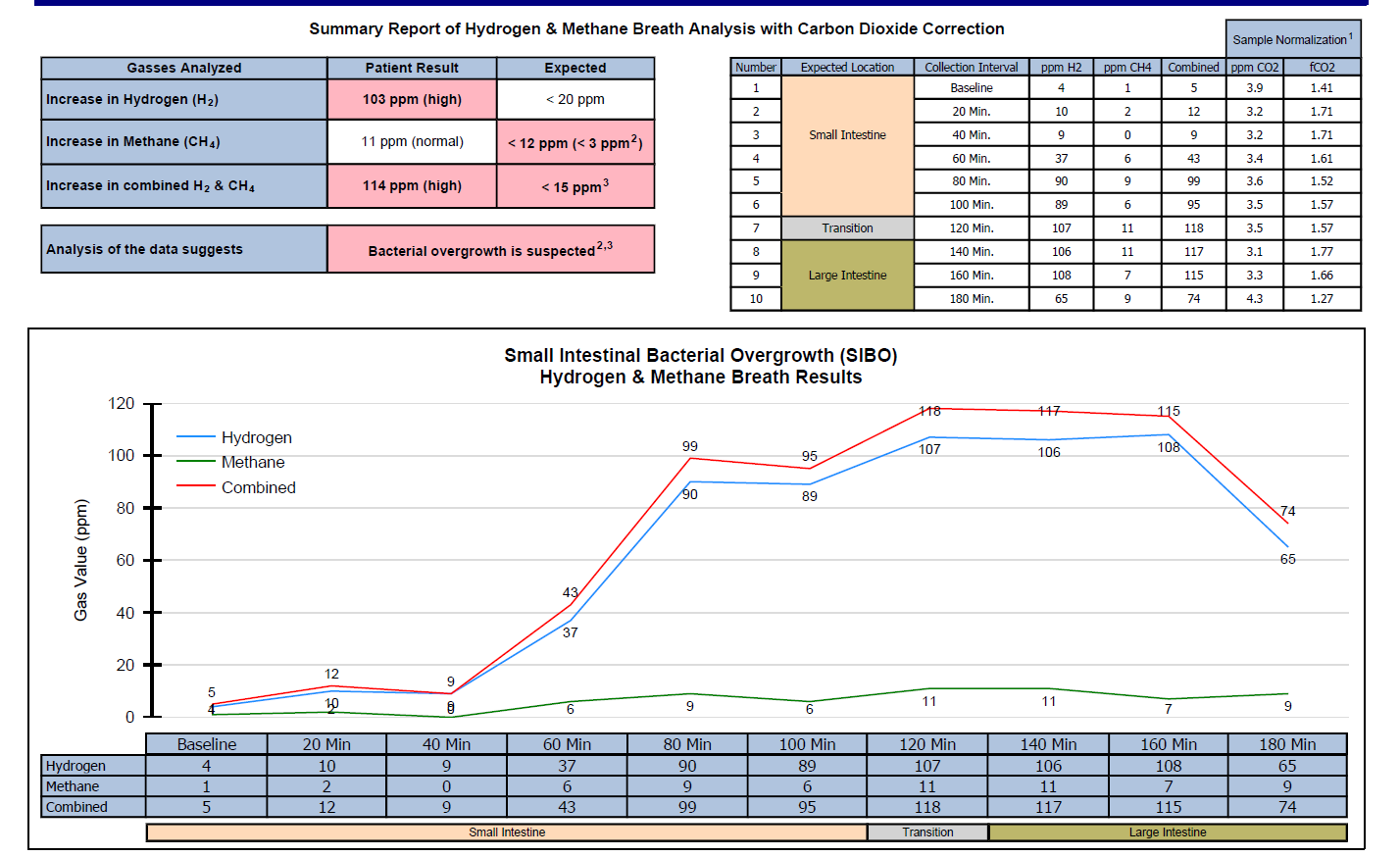
- Essentially we see a pattern of bacterial and fungal dysbiosis. Mold/biotoxin risk appears low.
- Dx
- Severe H2 SIBO, methane producer. DD: Citrobacter and yeast. LC: Campylobacter +indicans.
- Summary
- Aerodiagnostics Lactulose SIBO breath test
- H2 90, CH4 9
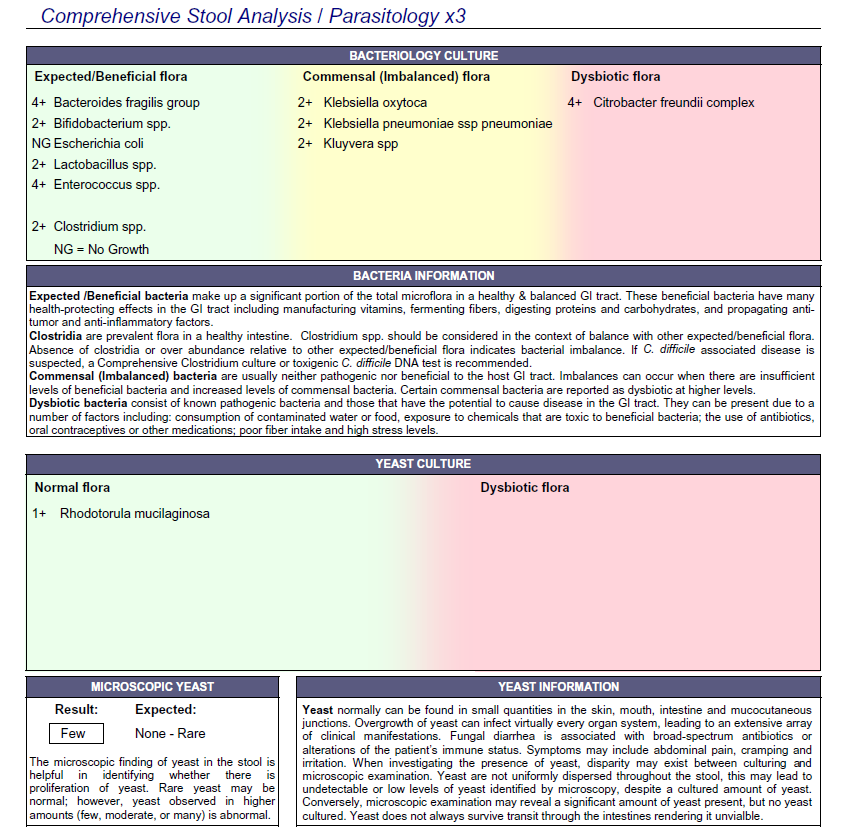
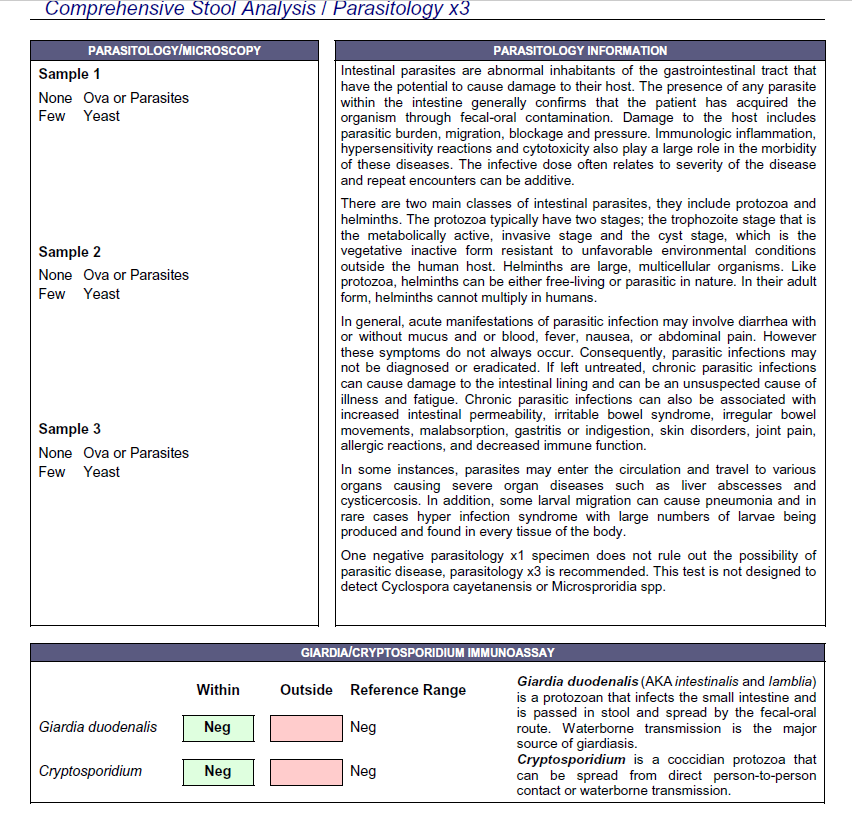
- Doctors Data Comprehensive Parasitology 3x stool test
- Dysbiotic bact: Citrobacter freundii complex +4. 3 commensals overgrown.
- Yeast 3x – microscopy
- LabCorp #1
- Stool Culture, complete Campylobacter – Abnormal
- Indican, urine qualitative: Positive Abnormal
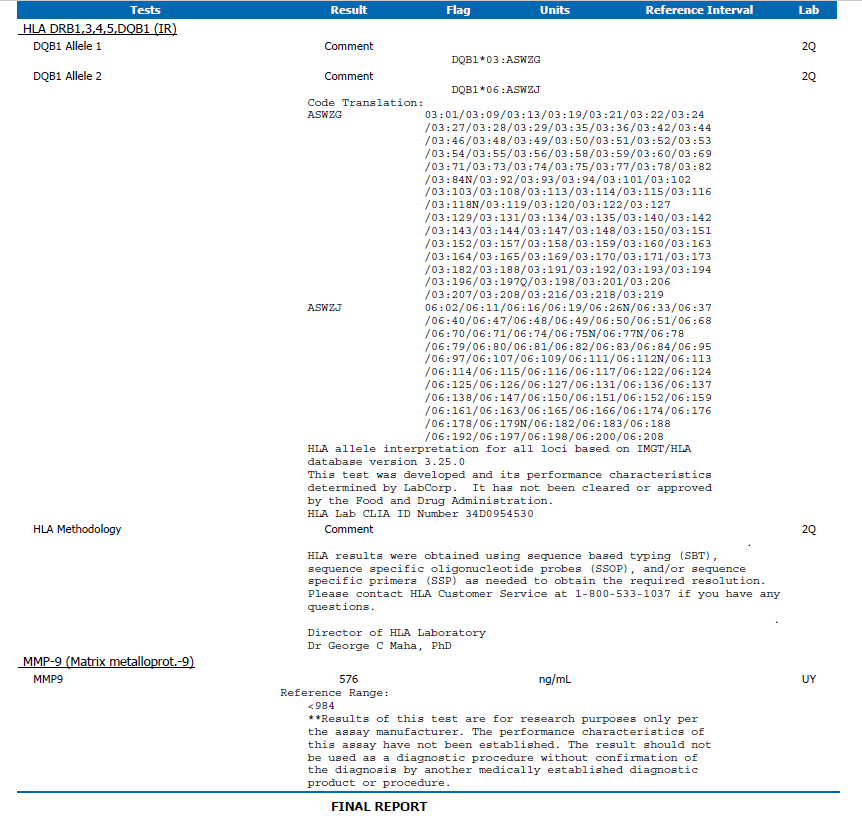
- LabCorp #2
- Basics, additions HgA1C 6-H, LDL 117-H
- Quest- IBSDetex
- Not drawn
- Life Extension Mold & Biotoxin Panel
- See below: Multi-susceptible/Chronic Fatigue, no other flags. Impression: low risk.
- TGFB was 3,800 in the past, now wnl.
- Aerodiagnostics Lactulose SIBO breath test
Impression
- 6/28/17 – Pimentel’s immunosuppressive drug use for high Vinculin has not been as effective as prior Habx therapy. He is giving because can’t due Rx prokinetic due to a cardio contraindication. As per my initial impression, I anticipate she will do well with our standard GI care and may need: SED (weight gain and gut healing), low dose cyclical Habx, probiotics, fungal treatment. Labs show a low likelihood of CIRS, in my opinion, but I will consider referral to expert later if she is non-responsive to GI therapies. They also show SIBO still present, but along with yeast and Campylobacter. Today will start with finishing trial of items from the initial program, then start Habx. Then after Habx consider low dose cyclical (LDC) Habx and intermittent SED (semi-elemental diet) use.
Recommendations
-
- Dietary
- Please continue with your previous paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals per day.
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week
- Treatment
- GI:
- S. boulardii
- Liver-gallbladder support formula
- Betaine HCl
- GI:
- Starting
- Continue experimenting with S. boulardii
- Continue experimenting HCl, LVGB
- Stop vitamin D now
- After this start on the antimicrobials
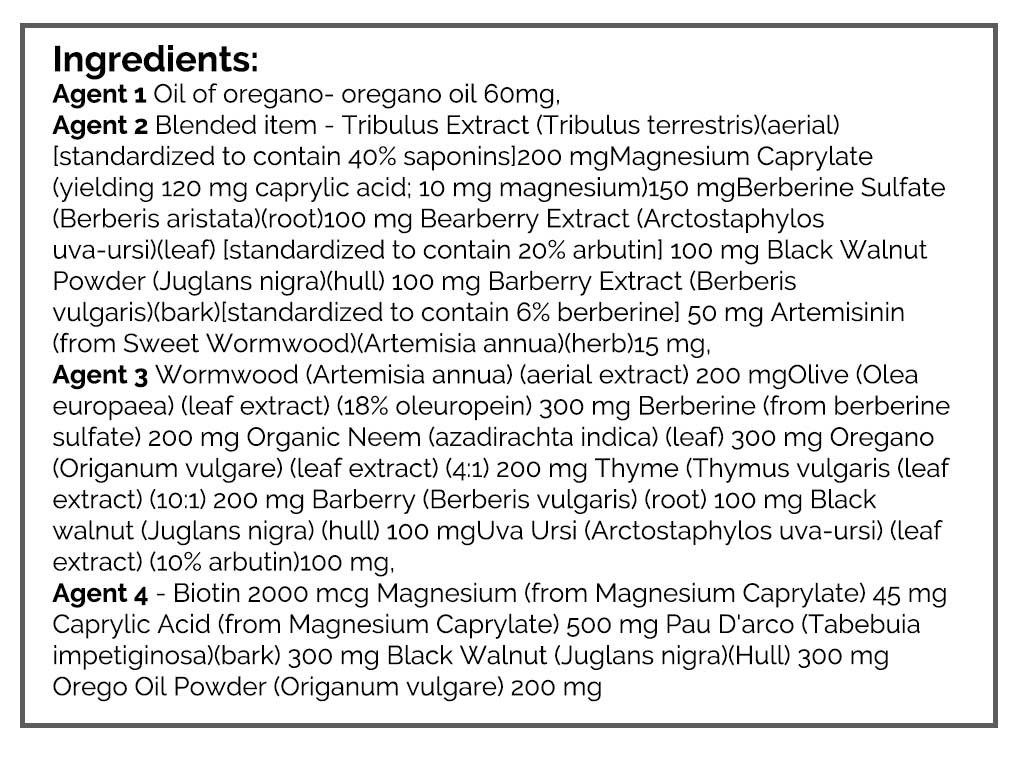
- GI: Herbal antimicrobial protocol
- FU: 4 weeks into the antimicrobial program, in 6 weeks
- Dietary
Visit 4
Subjective Assessment
- Started with Rifaximin, had a few days of die off, then started on antimicrobial blend – slight die off then OK. Is now on full month 1 protocol, and this is tolerable. Feels like Habx is helping – brain fog, energy, bowel consistency.
- Today is clearly better than the last visit.
- Improved:
- Brain fog, energy, bowel consistency. Nausea. Spasms. Urgen bladder. Achiness/flu-like. Insomnia.
- Same:
- Weight
- Worse:
- na
Impression
- 10/20/17 – Janet started with Rifaximin after seeing Dr. Pimentel, had a few days of die off but otherwise NR. Then started on Habx – slight die off then started to feel significantly better. Today is much improved. We will continue with the antimicrobial protocol, and will also have her bring more CHO into her diet. Then fu 4-6 weeks. Then after Habx, consider LDC Habx and intermittent SED use. Finally consider anti-hist protocol, Helminths, asking cardio about LDN, FMT or CIRS referral. Or consider 1) Perform 2-4 day trial with HCl, 2) trial of IBgard.
Recommendations
- Dietary
- Please continue with your previous paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals per day.
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- GI:
- S. boulardii
- Liver-gallbladder support formula
- Betaine HCl
- GI:
- Continue
- Experimenting with S. boulardii
- Experimenting HCl, LVGB
- GI: Herbal antimicrobial protocol
- Starting
- Push to continue to expand your diet to include more carbs: rice, potato, quinoa, corn…
- fu: 4-6 weeks
Visit 5
Subjective Assessment
- Just getting over a head cold
- Has ‘been doing really good’
- Still on Habx
- Improved:
- Gained 4-5 lbs, nausea, food sensitivities, insomnia, intestinal spasms, fatigue, bloating/burping, achiness/flu-like, urgent bladder
- Same:
- na
- Worse:
- Has head cold
Impression
- 11/17/17 – Today Janet continues to improve from Habx, all CCs have improved and this might be the only treatment needed. Today will start on 1/2 dose of current protocol, then fu in 4-6 weeks. Then either come off or consider 2nd-month Habx protocol. Note: we had only used 1st-month protocol formulas since she was responding so well. We will discontinue S. boulardii, HCl and LVBG as they did not appear to be causing improvement.
Recommendations
- Dietary
- Please continue with your previous paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals per day.
- Push to continue to expand your diet to include more carbs: rice, potato, quinoa, corn…
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- GI:
- See below
- GI:
- Starting
- Discontinue experimenting with S. boulardii
- Discontinue experimenting HCl, LVGB
- Start on a half dose of the antimicrobials
- Keep up the good work
- F/U: 1.5-3 months
Visit 6
Subjective Assessment
- Coming off Habx – caused regression (I did not instruct, she elected to try)
- Feels like she might be sensitive to fats
- HCl or ACV – rxn urgent bladder
- When flared has: nausea, fatigue, achy, brain fog and low mood
- Felt best at a semi-low dose of Habx
- Improved:
- Nausea (not 100%). Slightly better: food sensitivities, insomnia, intestinal spasms, fatigue, bloating/burping, achiness/flu-like, urgent bladder
- Same:
- Weight (115)
- Worse:
- Has head cold
Impression
- 1/17/18 – Janet is still better than BL but has regressed since coming off the Habx, she also notices she is fat sensitive when regresses. Today will start back on higher dose Habx and retest IBSDetex to get a comparison so as to assess if Pimentel’s Imuran is working. Will fu in 6-8 weeks while still on Habx. Consider other treatment options if relapsing and/or more improvement needed. Consider natural prokinetic post Habx and/or LDC Habx.
Recommendations:
- Dietary
- Please continue with your previous paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals per day.
- Push to continue to expand your diet to include more carbs: rice, potato, quinoa, corn
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- GI:
- See below
- GI:
- Starting
- GI: Habx, full dose
- F/U: 6-8 weeks
- Testing
- Quest – IBSDetex
Visit 7
Subjective Assessment
- Habx – feeling a lot better.
- Upon reintroduction some foods problematic – eggs, honey: achy, tired, foggy. High fat intake, or high fiber intake (brown rice noodle, quinoa). Granola.
- Improved:
- All, other than flares from food intro reactions. “QOL is a lot better”.
- Same:
- NA
- Worse:
- NA
Lab Assessment
- IBS Detex
- CdtB 0.44. Vinculin 1.69
Impression
- 2/28/18 – Todays IBSDetex shows no longer has CdtB antibodies, but does have Vinculin, however they are improved. Janet has globally continued to improve. However, she does notice some foods, especially grains and eggs aggravate. Also, high-fat meals. Sounds like she is eating the same thing every day and this is causing acquired intolerances, and/or that she may be bile deficient. Today will start rotation and on pancreatic enzyme + bile.
Recommendations:
- Dietary
- Please continue with your previous Paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals.
- Push to continue to expand your diet to include more carbs: rice, potato, quinoa, corn…
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- GI:
- See below
- GI:
- Starting
- Continue with a lower dose of antimicrobials.
- GI: Bile Acid, Zenpep (from the previous prescription)
- Eat with a food rotation
- F/U: 1.5-3 months
Visit 8
Subjective Assessment
- Is now off Imuran – feels better overall.
- Shaking feeling, racing heart after some meals.
- The cardiologist has found falling ejection fraction.
- Zenpep 45 min before a meal – helpful.
- Bile acid – did not start.
- Rotation – partially helpful.
- Improved:
- All CCs are still improved.
- Same:
- Weight (115).
- Worse:
- Shaking feeling, racing heart (after some meals).
Lab Assessment:
- Nurse Practitioner Testing
- Pancreatic enzymes – wnl, HgA1c – wnl, insulin – wnl. High C-peptide.
- Wnl – within normal limits
- Pancreatic enzymes – wnl, HgA1c – wnl, insulin – wnl. High C-peptide.
Impression
- 5/2/18 – Has maintained all previous improvements, but is now having episodes of shaking and racing heart. Cardio feels this is due to the medication change and is taking steps to resolve. NP found high C-peptide and suspect this might be diabetes or pancreatic insufficiency. Janet has responded to Zenpep. Today will start on more Zenpep and/or bile and will start on liver gallbladder support again. Will continue LDC Habx but will rotate to different antimicrobial agents now.
Recommendations
- Dietary
- Please continue with your previous Paleo/low FODMAP-like diet. But, look into the Fast Tract Diet’s FP calculator as a method of increasing your daily carb intake.
- Continue to experiment with intermittent fasting where you eat 2 larger meals a day instead of eating 3 meals per day.
- Push to continue to expand your diet to include more carbs: rice, potato, quinoa, corn…
- Eat with a food rotation
- Lifestyle
- Please obtain activity, preferably outside in nature, at least 3 times per week.
- Treatment
- GI: LDC Habx
- GI: Bile Acid, Zenpep (from the previous prescription)
- Starting
- Switch to a different antimicrobial protocol
- Start liver-gallbladder support
- F/U: 4-8 weeks
Dr. Ruscio’s Comments
Janet’s case is a clear example of why it is important to focus on fundamentals and not ‘reinvent the wheel’. Yes, we want to be thorough in our evaluation and, as an example, check for CIRS because it was supported. However, what led to improvement with Janet was not an experimental immune treatment for her motility autoimmunity nor was it CIRS detox therapy. Janet improved from simple herbal antimicrobials, expanding her diet, digestive support, and a food rotation. There may be a time and place for more experimental therapies, and that is fine. Just make sure not to overlook simple and fundamental treatments. Also, remember that we all have our strengths and weaknesses. Dr. Pimental has done volumes for advancing the knowledge base in SIBO, and his Imuran treatment may be helpful for other patients. For Janet however, natural treatments were the key to success.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!