Practitioner Case Study – January 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Abnormal breath testing in IBS: a meta-analysis
- Therapy options in irritable bowel syndrome
- Effect of rifaximin treatment on anti-vinculin antibodies in IBS with diarrhea
- A meta-analysis of Hashimoto’s thyroiditis and papillary thyroid carcinoma risk
Practitioner Question of the Month
Practice Tip
![]()
Case Study
Dr. Ruscio’s Note: This was a guest case study from Dr. Farshid Sam Rahbar, who is a gastroenterologist who is also interested in Lyme and the Lyme-SIBO connection.
Patient Info:
- James, 45yo, male
James was not aware of his first patient visit, as his wife Susan attended alone to seek a professional opinion. Susan explained that her husband was a chronic sufferer of a ‘mystery illness,’ and that he had given up on seeing doctors as no one had been able to help. James was now convinced that he was dying; he referred to himself as a ‘genetic failure,’ and his symptoms were worse than he had ever had. This visit marked Susan’s last attempt at seeking help.
Visit 1 – History from Wife
At the time of this visit, James was 45 yrs old. He grew up in Ohio and lived a very active ‘outdoors’ type of youth, hiking and camping in nature with his friends. By his mid-20s, James moved to Los Angeles, where he was a social butterfly and a ‘brilliant aspiring accountant.’ Susan and James met in college, they fell in love, and were married within months.
Susan reported that within a few years James had ‘transformed’ into a completely different person. He was unable to complete his studies due to a severe debilitating ‘fatigue.’ He developed more and more strange low-grade symptoms, and over the next 10 years, James saw more than 20 specialist physicians in America as well as Europe, and the recurring diagnosis through the exclusion of serious pathology was that his issues were likely psychological.
But James’ symptoms involved multiple body systems and they progressively worsened with time. He had severe constipation, abdominal bloating, and anorexia. On occasion he would curl up screaming in pain, clutching at his abdomen. James would refuse to go to urgent care and would wait for the pains to subside, which would happen after around 5 hours.
James also suffered severe headaches. He would report nondescript chest pains, chest tightness, multiple migrating joint pains, transient rashes on his distal limbs, impaired cognition, and insomnia. He had become nervous when he previously was a ‘laid back’ kind of guy, and as a result of the above, he was also severely depressed. James had also become housebound.

Plan
- Urgent new patient visit for James.
Visit 2 – Patient attends visit, Exam, and Lab Testing
Patient Visit and Medical History
James was a charismatic and kind-natured man who spoke slowly and carefully. He filled in the gaps from his wife’s account of events, and proceeded to describe at great length his battle with this ‘mystery illness.’ The additional details are as follows:
James had traumatic brain injury twice in his teens, both of which were high impact head injuries without LOC. He had ‘mono’ during his college days, and remembered the day it happened remarkably well. James had woken up “feeling the worst that I ever had.” During this visit, he realized that he had not felt well since that day and that it was also when his anxiety first developed.
James elaborated on the vigor of his youth and how this ‘severe fatigue’ allowed his previous aspirations to just ‘slip away.’ Now he has excessive daytime sleepiness and is able to sleep 18 hours in a night, but still wakes up feeling fatigued. He can take 6 Adderall at one sitting with no improvement in his energy levels. Additionally, James can no longer multitask and describes a good day as walking to the local store to pick up a few groceries.
His abdominal pains can be 10/10, they are periumbilical and associated with distension; James is chronically severely constipated. Endoscopy, colonoscopy, and abdominal ultrasounds have all been ‘normal,’ and he has not had a CT scan. The unwitnessed ‘collapses’ have come on ‘out of nowhere,’ and all James could contribute to this was that he wakes up on the floor without any recollection of what had happened. He has treatment-resistant depression; SSRIs and tricyclics have had a poor effect, and Suboxone is all that has helped.
The main goal that James set during this visit was ‘to understand why this is happening.’
Exam
James had a grossly normal examination. Pertinent findings included obesity, a low grade lower abdominal tenderness, peripheral edema with associated hair loss and discoloration of the skin. His Rhomberg test was negative.
Impression
James presented with digestive systems in a setting of multi-system involvement. His gastrointestinal symptoms indicated intestinal malabsorption, likely caused by SIBO or SIFO. Gastric bile reflux was likely a part of the anorexia and nausea. In light of the diverse systemic symptoms, neurologic involvement, and that he grew up on the East coast, the possibility of chronic tick-borne disease with cerebral involvement was a likely consideration. Endocrine, neurological, and cardiac causes also had to be ruled out.
Plan
Dietary Recommendations:
- Anti-reflux measures. Eat slowly, chew well, chew xylitol gum for 5-10 minutes after meals. Do not eat or drink for 2 hours before bed.
Testing:
- Blood Tests
- Testosterone screen. ACTH. Cortisol. DHEA, DHEA-S. Pregnenolone. Estradiol. Dihydrotestosterone. IGF1. IGFBP3. PSA. Zinc, Copper, Magnesium, Lead, Mercury. ANA + cascade. Companion infections. Ceruloplasmin. Borrelia, Bartonella, and Babesia screen. Specialist Gluten testing.
- Urinalysis with reflex to culture
- Comprehensive stool analysis
- Micronutrient urine testing
- SIBO breath test
Specialist Referral:
- Sleep study analysis for apnea/narcolepsy
- Cardiology review for syncope episodes
- Neurologist to investigate traumatic brain injuries
Suggested investigations that were deferred by patient:
- CT Abdomen
- EGD
Follow-up – 3 weeks or sooner
Visit 3 – Lab Tests Interpretation, Specialist Referral Opinions, and Treatment Evaluation
Specialist Opinions:
The neurologist believed that seizures were a possibility, and MRI brain and EEG were performed as per epilepsy protocol. The EEG was NORMAL in both the awake and drowsy state, MRI head was normal, and the pituitary gland was unremarkable.
The cardiologist cleared syncope as well as other cardiac causes. The Sleep Study findings were consistent with narcolepsy.
Lab Test Results:
- SIBO Breath test – negative
- Gluten screen – negative
- Stool testing: no fungus, low SCFAs, high secretory IgA
- Some micronutrient deficiencies
- Multiple companion infections
- Borrelia, Babesia, and Bartonella – negative through the traditional lab
- Vitamin D deficiency
Additional testing ordered:
- FSH, LH, Prolactin, ACTH, 24-hour urinary cortisol
- Free T3 and Total T3
- Complement cascade
- T Cell subsets
- IgG subclasses
- Specialist Lyme testing INCLUDING RELAPSING FEVER GROUP
- Mycotoxins
Supplement Recommendations:
- Uncompressed multivitamins
- Benfotiamine
- Vitamin D – 5000 units daily
- Zinc carnosine
- Colostrum
- Magnesium
- Probiotics
- Omegas
- Antioxidants
Follow-up – 3 weeks or sooner
Visit 4 – Lab Tests Interpretation, Treatment Evaluation
Lab Results:
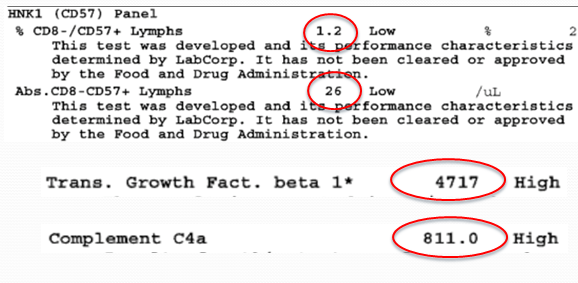
Low CD57, High TGF Beta 1, and Complement C4a
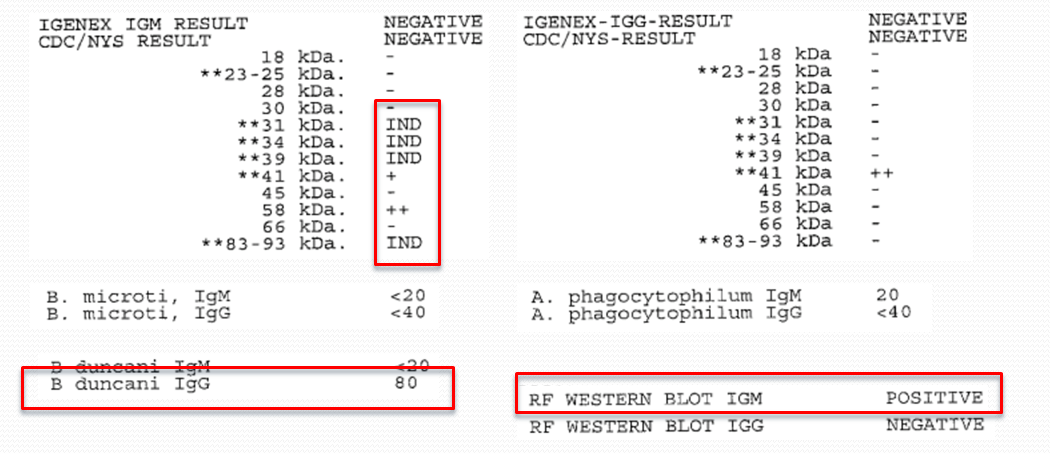
Tick-borne testing – positive for relapsing fever
Mycotoxin analysis – equivocal gliotoxin only
Fungal nasal swab analysis – negative for fungus or mold
Lab Result Interpretations:
- HLA testing: matched 15-6-51 – Post Lyme/MS/Narcolepsy
- Mycotoxins urinalysis was negative
- Low complement factors evident
- Sinus cavity negative for fungus/mold
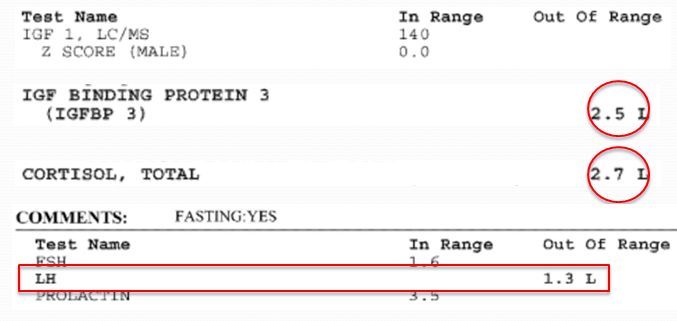
- IGF1 was low normal – but IGF-BP3 was low
- Low TSH
- Normal Estradiol, Prolactin, ACTH, and Cortisol was inappropriately low
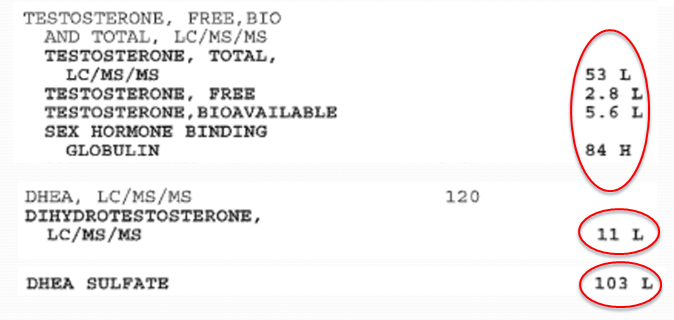
- Low testosterone – this required ultrasound of testes and GH stimulation test as well as a replacement
- Evidence of Babesia dancani exposure and relapsing fever Borreliosis
Working Diagnosis:
Probable panhypopituitarism, with hypogonadism, and HPA axis dysregulation.
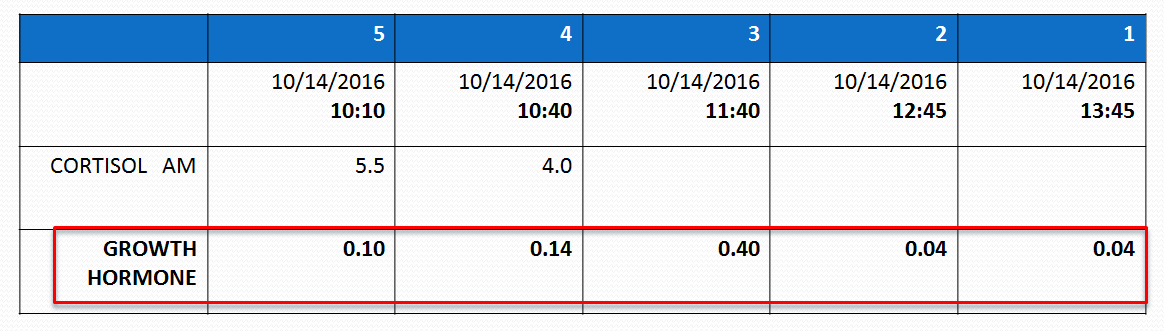
Visit 5 – Growth Hormone Stimulation Test
A GROWTH HORMONE STIMULATION TEST was performed.
Result
Abnormal – no response to a stimulus.
Treatment
James was placed on growth hormone, cortisol, and testosterone replacement. He was referred to a Lyme specialist and received treatment for Lyme with Rocephin IV.
Visit 6 – Emergency Visit
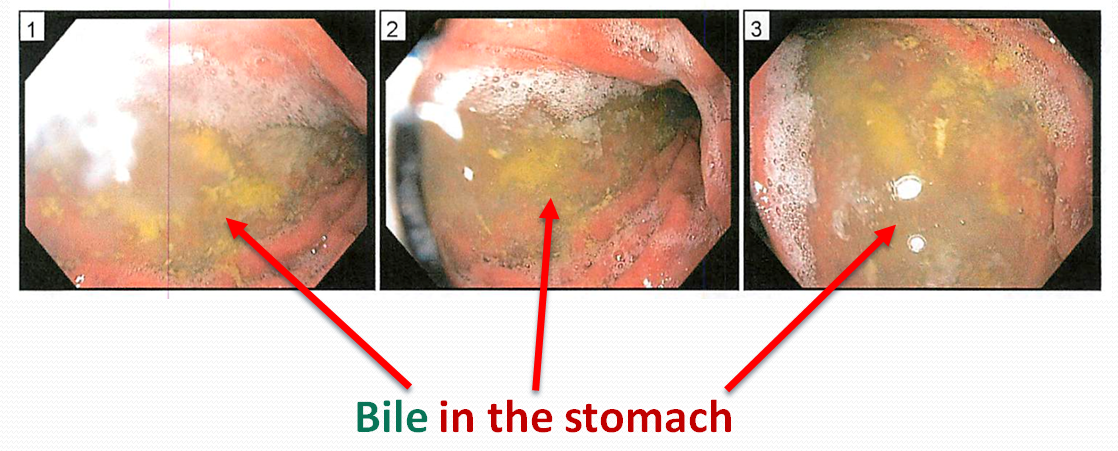
During IV ABX treatment, although improvements were being made, James developed another episode of severe abdominal pain and underwent endoscopy.
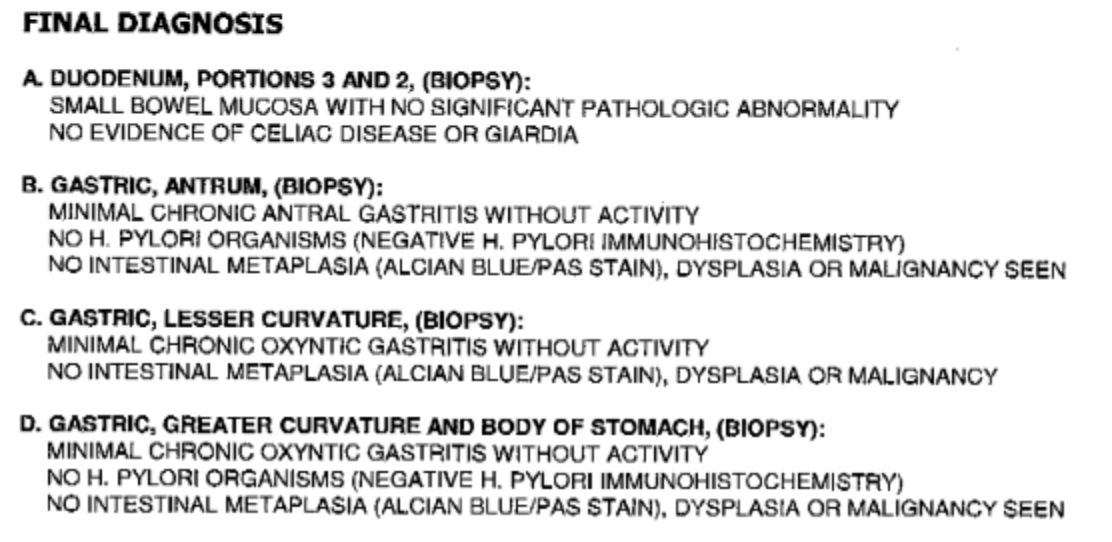
Biopsy Results
Findings
There was evidence of reflux esophagitis. James was provided a short course of anti-reflux treatment with good results. We speculate the bile in the stomach was likely secondary to small bowel dysbiosis of fungal origin due to long-term use of antibiotics.
James continues to see a Lyme-literate physician, and his GI symptoms have stabilized with anti-reflux measures and antifungal therapy.
Dr. Ruscio’s Comments
It was interesting to see the process and workup Dr. Rahbar goes through. Keep Lyme and Lyme co-infection in mind in patients that are otherwise non-responsive. I myself am curious as to the results this patient experienced as treatment progressed. I will ask Dr. Rahbar to update us in the comments section soon.
You can see more from Dr. Rahbar from his interview on our podcast or at his website.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!