Practitioner Research Review – January 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Abnormal breath testing in IBS: a meta-analysis.
https://www.ncbi.nlm.nih.gov/pubmed/20467896
Study Purpose
- Assess breath testing results in those with IBS.
Intervention:
- Meta-analysis of 11 studies.
Main Results:
- “breath testing was more often abnormal among IBS subjects than healthy controls (OR = 4.46).”
- Studies have documented that breath testing can predict who will respond to antibacterial therapy and that test results improve as a patient’s symptoms improve.
- In one of these, normalization of the breath test with antibiotics predicted a greater proportion of subject response to treatment. In the other study, subjects responding to the antibiotic rifaximin had a significantly greater reduction in hydrogen compared to non-responders.
Additional Results:
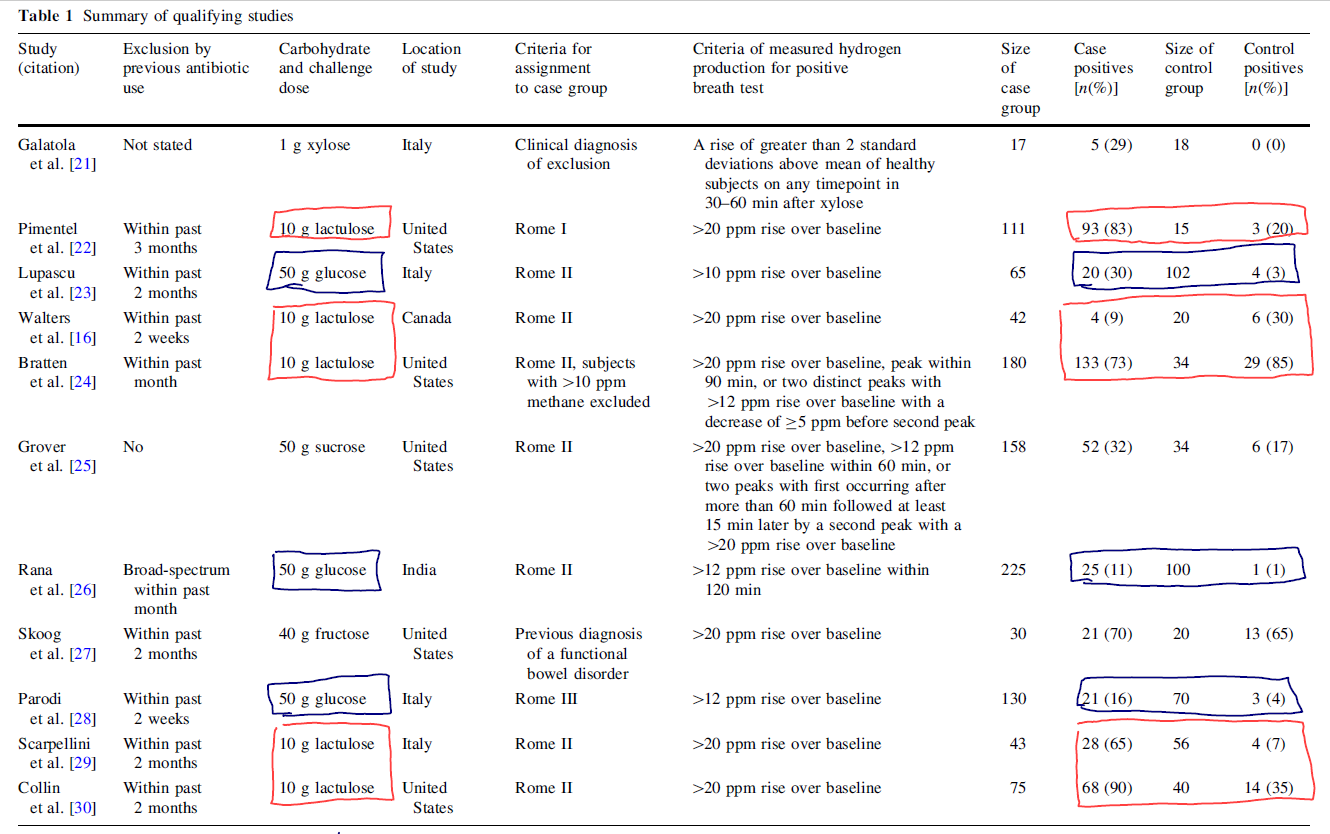
- Below is a chart wherein I have highlighted a side-by-side comparison of lactulose and glucose testing (blue squares = glucose, red = lactulose). In these studies, frequency of positive tests results in those with IBS were compared to healthy controls. If you compared the ‘case positive’ to ‘control positive,’ you can easily see that healthy controls are positive more often when using lactulose as compared to glucose. This is where the main criticism for use of lactulose comes from.
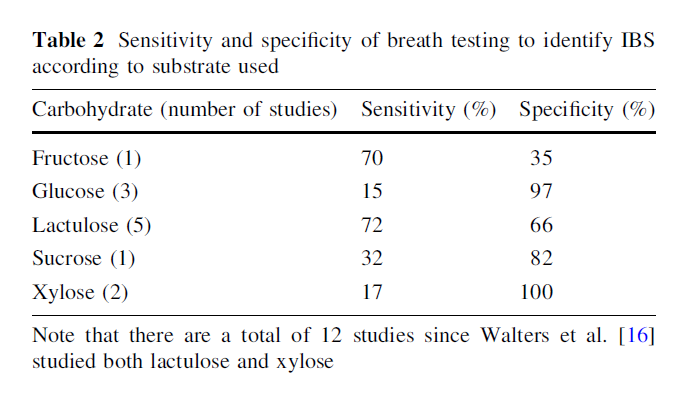
- However, conversely, the glucose test may miss some cases as it has a low sensitivity (see second image, table 2). Either test can work clinically, it’s just important to be aware of the potential for false positives with lactulose. Meaning, not everyone who tests positive requires treatment and treatment should be a clinical call taken on a case by case basis.
- Rapid transit may be the reason for false positives with lactulose testing.
- “In the setting of rapid transit, lactulose could reach the colon and occur at a time less than 90 min in this circumstance.”
Authors’ Conclusion:
- “This study demonstrates that the breath test findings in IBS appear to be valid. While this meta-analysis does not suggest that the breath test findings imply SIBO, the abnormal fermentation timing and dynamics of the breath test findings support a role for abnormal intestinal bacterial distribution in IBS.”
- Or said another way, “The results demonstrate that a ‘positive’ breath test is more common in IBS patients compared to controls, irrespective of definition.”
Interesting Notes:
- Most of the lactulose studies used a 90-minute cutoff, and this is likely why the North American Consensus paper recommended a 90-minute cutoff.
Clinical Takeaways:
- Breath testing for SIBO has been validated to identify ‘dysbiosis,’ but not SIBO per se. Positive test results may predict which patients are the best candidates for antibacterial therapy.
Dr. Ruscio’s Comments
The text I highlighted from the authors’ conclusion is important to bear in mind. The main point is that current evidence suggests dysbiosis is involved in IBS, and not necessarily SIBO per se.
“These data support the utility of breath testing in IBS, at least as a confirmation that abnormal fermentation patterns seen on test results seem indicative of some bacterial derangement in IBS. However, the proof that this is due to SIBO is still controversial.”
And at the end of the day, testing may still help us identify patients who should undergo anti-bacterial treatment.
“breath testing in IBS has more theoretical utility in identifying patients with the potential to benefit from antibiotic therapy.”
To say SIBO breath testing has no utility, however, is clearly not an evidence-based nor a well-informed statement. That being said, the data here are not perfect, so we should remain open-minded on future findings.
Therapy options in irritable bowel syndrome.
https://www.ncbi.nlm.nih.gov/pubmed/21389791
Study Purpose
- To review the effectiveness of available therapies in IBS.
Intervention:
- Review of 121 trials in IBS from the last 35 years. Non-systematic.
Main Results:
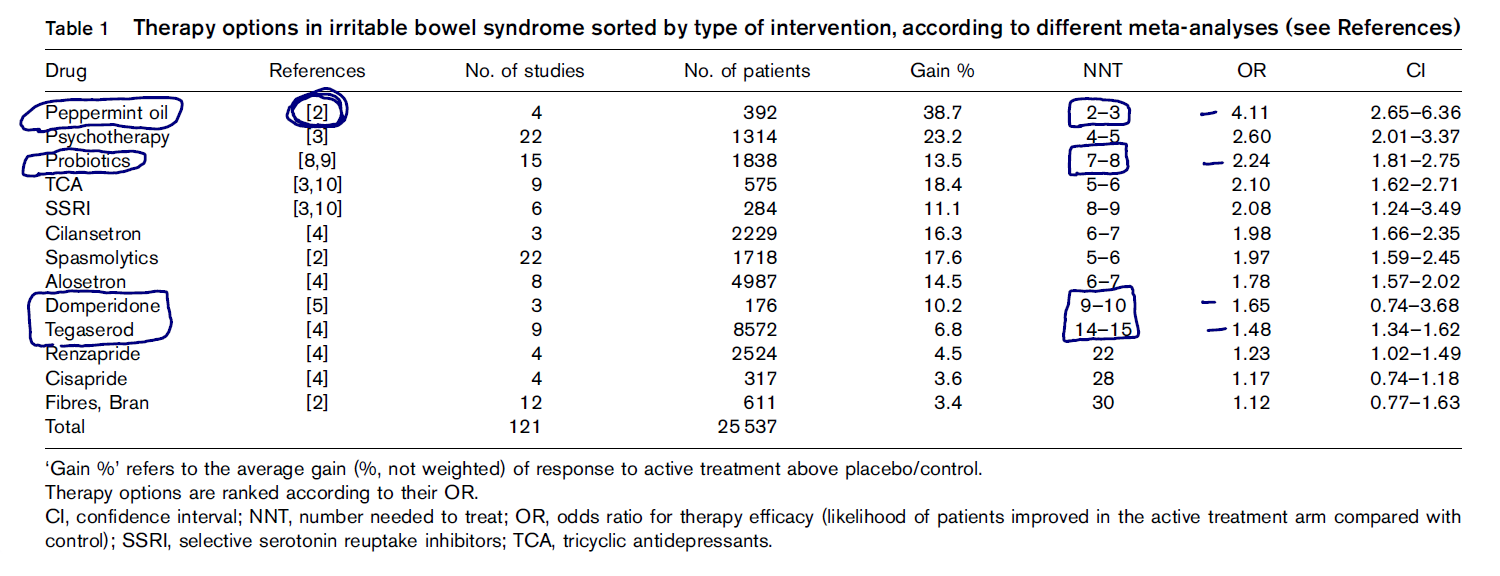
- Natural treatments were found to be the most efficacious, namely peppermint oil.
- “Highest efficacy is currently found for peppermint oil, followed by psychotherapeutic and psychopharmacological interventions and probiotics.”
- Peppermint oil, physiotherapy, and probiotics had equal or better Number Needed to Treat scores (NNT).
- Essentially, NNT equals the number of patients you must treat with a therapy to see a positive outcome. So, for every 2-3 patients you treat with peppermint oil, you will see one positive response. This is far better than some of the other drug therapies listed.
- Fiber scored poorly, not surprising as fiber can flare IBS. However, these results may be skewed if the bran was only insoluble bran, which is what I think they mean here. Soluble fiber, especially in constipation-type IBS, can be helpful.
Additional Results:
- Remember the best evidence for Iberogast is in dyspepsia (indigestion).
- “Other phytopharmaka such as Iberogast, which is a mixture of nine herbal residuals, have been shown to be of therapeutic value in functional dyspepsia [13], another functional gastrointestinal (GI) disorder, by relaxing the gastric smooth muscle tone [14] and improving adaptation to food load [15], but its efficacy in IBS and in lower GI dysfunction has not yet been shown.”
Authors’ Conclusion:
- “first-line therapy may include probiotics and eventually also fiber supplements – despite their low efficacy – because of their low side-effects in patients with constipation-predominant IBS, and antispasmodics and peppermint oil for patients with diarrhea-predominant IBS or with alternating bowel habits.”
Interesting Notes:
- N/A
Clinical Takeaways:
- Natural therapies may be the most efficacious therapies for IBS.
- Peppermint oil and probiotics are two of the safest and most effective therapies.
Dr. Ruscio’s Comments
Nothing shocking here, natural medicine wins for IBS. If you haven’t experimented with peppermint oil, it is worth considering. More to follow on this in a coming podcast.
Effect of Rifaximin Treatment on Anti-Vinculin Antibodies in IBS With Diarrhea
http://www.gastrojournal.org/article/S0016-5085(16)32371-X/abstract
Study Purpose
- Assess if treatment with rifaximin would decrease anti-vinculin antibodies.
- Anti-vinculin antibodies can lead to altered motility and subsequent SIBO.
Intervention:
- “A subset of IBS-D subjects recruited from a large-scale multicenter clinical trial for IBS-D (TARGET 3).”
Main Results:
- Rifaximin did not impact antibodies.
- “Among these 102 subjects, 25 (24%) were positive for anti-vinculin antibodies (titer ≥1.68 for OD). Rifaximin did not appear to have a significant effect as anti-vinculin antibodies before (1.25±0.78) and after rifaximin (1.24±0.98) were similar (P=0.77) by paired t-test. In addition, among only positive test results (n=25), there was no significant change in test levels.”
Additional Results:
- N/A
Authors’ Conclusion:
- “This is the first study to assess the effect of rifaximin on a newly validated biomarker for IBS diagnosis based on the development of autoimmunity. Rifaximin treatment had no effect on these antibody measurements or the determination of a positive test result.”
Interesting Notes:
- N/A
Clinical Takeaways:
- Rifaximin does not improve anti-vinculin antibodies.
Dr. Ruscio’s Comments
I must admit I was surprised by these findings. I would assume that a therapy that reduces dysbiosis and symptoms (rifaximin or herbal antimicrobials) would improve immune function in the GI. Perhaps if the retesting time was extended we would see improvement in the antibodies, meaning perhaps the retesting was performed too quickly here.
In any case, this is good for clinicians to be aware of. Also, bear in mind that we still have not established how to treat these antibodies, so be cautious. Cautious in the sense that the IBS Check or IBS Detex testing has utility as a screening tool, but does not direct the clinician to any treatment. The speculation that a positive antibody test would predict the need for prokinetic therapy seems plausible, but has not yet been proven.
A meta-analysis of Hashimoto’s thyroiditis and papillary thyroid carcinoma risk.
https://www.ncbi.nlm.nih.gov/pubmed/28977955
Study Purpose
- Assess risk of thyroid cancer in those with Hashimoto’s.
Intervention:
- A meta-analysis of 27 studies and over 76,000 patients.
Main Results:
- Having Hashimoto’s increases risk of thyroid cancer.
- “The overall pooled odds ratio (OR) of the PTC risk for HT (HT versus non-HT) was 2.12.”
Additional Results:
- Inflammation may be the reason for increased cancer risk.
- “The relationship between inflammation and PTC is complex and still not completely understood [33]. Tamimi et al. found a significantly higher rate of lymphocytic infiltrate in patients with PTC, and the activated inflammatory response present in HT may create a favorable setting for malignant transformation [34]. The inflammatory response may cause DNA damage through the formation of reactive oxygen species, resulting in mutations that eventually lead to the development of PTC.”
Authors’ Conclusion:
- “Our meta-analysis confirmed that HT predisposed patients to the development of PTC.”
Interesting Notes:
- “Papillary thyroid carcinoma (PTC) is the most prevalent thyroid cancer and it represents 80-90% of all thyroid cancers.”
Clinical Takeaways:
- Those with Hashimoto’s are at increased risk for thyroid cancer.
- Thyroid cancer screening in this population appears warranted.
Dr. Ruscio’s Comments
You may have heard me make the remark that those seeking natural medicine care for their thyroid health should not turn a blind eye to conventional medicine, and cite the example that those with Hashimoto’s have an increased risk of thyroid cancer and therefore should not forgo any recommended conventional screenings. This meta-analysis supports that statement. To provide additional clarity here, I will review practice guidelines for thyroid cancer screening in a coming issue of the Review.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!