Practitioner Case Study – October 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Thyroid Antibody Interpretation, Selenium Supplementation, and the Gut-Thyroid Connection
- Folic Acid Reduces Stroke in Those with High Cholesterol and MTHFR
- Folic Acid Reduces Stroke in Those with High Homocysteine and MTHFR
- Helminth Therapy to Stabilize Mast Cells
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Moriah, 5yo girl
- Dx: SIBO
- Rx: N/A
- Chief complaints:
- Food sensitivities, 10-CO
- Gas, 8-INT
- Diarrhea, 8-INT
- Mood swings, 8-INT
- Red cheeks, abdominal pain, eczema
Visit 1 (day 1) – History and Exam:
Moriah is a generally healthy 5yo girl, with a good diet and lifestyle. She has a supportive mother with good outlook on her health.
She has been dx with SIBO, but not treated. Is very reactive. Has responded very well to low FODMAP with SCD. She reports reactions to FODMAPs, carbs, probiotics, dairy, fermented foods, and Amoxicillin…
Has not yet been treated for SIBO, but should do well with treatment as she exhibits many signs of SIBO, histamine intolerance, and CHO malabsorption. She also may have D/L-lacticacidosis and enzyme insufficiency.
Challenge will be finding treatment she tolerates, but if/when we do I suspect she will respond well. She may do better with Rx instead of herbal Abx due to reactivity, mind this.
IBD is also potential. Should do well with the standard model if we can find a tolerable treatment. FMT might be a consideration if not. Prognosis fair to good.
Initial impression
- Moriah presents with a presentation type I have seen in a number of young children: IBS-like symptoms presenting with histamine intolerance symptoms. These cases oftentimes respond well to simple treatment plans. This is because they are so reactive that the less-is-more approach works better as it reduces reactions.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- SIBO breath test – she already performed with outside doc
- LabCorp Panel
- Full GI workup
- D-Lactate, urine
- D-Lactate, plasma
- Rationale
- This should be self-explanatory. We want to rule out SIBO or other GI dysbiosis or infection that might be driving her CCs.
Recommendations
- Continue with your previous Low FODMAP w/ SCD
- Perform a 1 week trial of the low histamine diet in combination with the above, continue if it helps.
- After a 1 week trial of this diet, add in the supplements. Be on supplements for at least 2 weeks before following up.
- Nutritional Support: Vitamin D/K
- GI: Digestive enzyme, acid and bile blend; Vitamin C
- Experiment with an OTC anti-histamine if the supplements are not helpful.
- FU: 4 weeks
- Rationale
- A low FODMAP diet can lower histamine, so we want to continue with this. But since she is still exhibiting histamine intolerance symptoms, we can go a step further by performing a trial of full-on low histamine diet.
- We partition the start of diet and supplements to isolate for effect.
- Moriah’s symptoms could be due to enzyme deficiency, so a trial is warranted.
- Vitamin C and anti-histamines can lower histamine.
Visit 3 (day 30) – Lab Interpretation and Treatment Evaluation
Lab Interpretation:
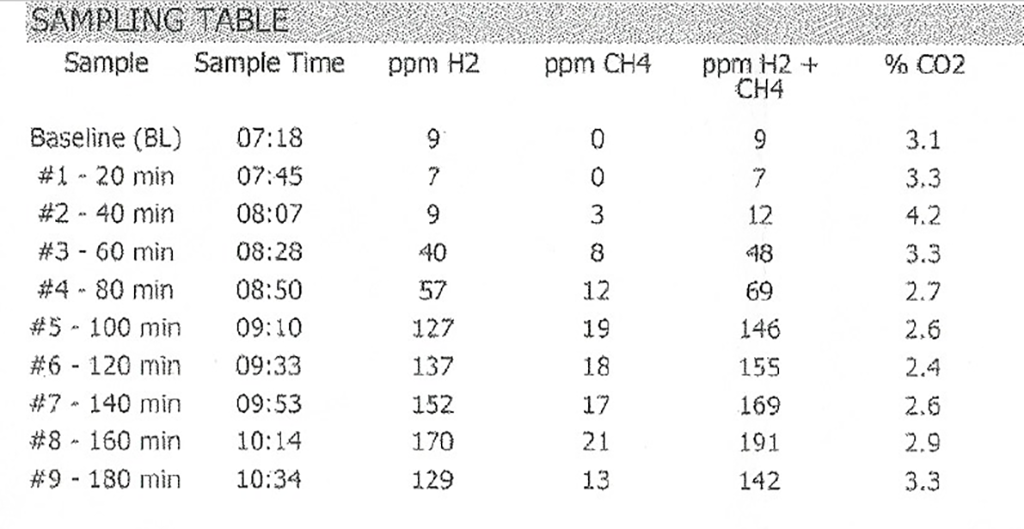
- SIBO breath test
- H2 127, CH4 19
- Quest
- Normal, see below. A blank marker means it was not performed.
- Summary
- SIBO positive. I used 100 min cutoff; however, for a 5-year-old the 80 cutoff might be more befitting. Either way, she is positive.
- Lactates were not performed.
Subjective Assessment:
- Benadryl – responded very well
- Low histamine diet – hugely helpful
- Enzyme/acid & Vitamin C – likely did not help
- Improved:
- Gas, diarrhea, red cheeks, abd pain, eczema, mood swings
- Same:
- Food sensitivities
Impression:
- Moriah has previously responded well to low FODMAP w/ SCD, and had rxns to probio and fermented foods. SIBO recently dx, today’s Quest panel is UR. Low histamine hugely helpful, Benadryl also helped. Since she is SIBO treatment naïve, I anticipate very good response if we can find tx that is tolerated as is very reactive. High D-lactate and histamine, highly supported. Today we will start herbal Abx.
Recommendations:
- Continue previous plan
- Low histamine diet
- Nutritional Support: Vitamin D/K
- GI: Digestive enzyme, acid and bile blend; Vitamin C
- Experiment with an OTC anti-histamine if the supplements are not helpful.
- GI: Herbal Abx; Allicillin and Oregano. Take WITH food. Use 1/2 adult dose, which is listed in your notes.
- FU: 4-5 weeks
| D-Lactate, urine | ||
| D-Lactate, plasma | ||
| Stool Culture, complete | WNL | |
| Clostridium difficile Toxins A and B, EIA | WNL | |
| H. Pylori stool antigen | WNL | |
| H. Pylori IgA, IgG, IgM | ||
| H. Pylori Breath Test | WNL | |
| Yersinia Enterocolitis IgM, IgG, IgA | WNL | |
| Yersinia Stool Culture | WNL | |
| Ova and Parasites 3x Examination w/o Giardia | X2 only performed -WNL | |
| GIARDIA AND CRYPTOSPORIDUM Ag | WNL | |
| Yeast Only, Culture w Reflex to ID (stool) | WNL | |
| Candida Antibodies, IgA, IgG, IgM, ELISA | WNL | |
| Toxoplasma gondii Antibodies, IgG | WNL | |
| Toxoplasma gondii Antibodies, Quantitation, IgM | WNL | |
| Toxoplasma gondii, PCR (whole blood) | WNL | |
| E histolytica, Amebic Antibodies | WNL | |
| Trichinella (Tissue Worm) Ab, SIgA | ||
| Ascaris (Roundworm) Ab, IgE | WNL | |
| T. solium (Tapeworm) Ab, serum (aka Cysticercus Ab, serum) | WNL | |
| Indicans, urine qualitative | Borderline – 1+ | |
| Benzoate | ||
| Eosinophil Cationic Protein ( Eos. protein X) | WNL | |
| White Blood Cells (WBC), Stool | WNL | |
| CRP (c-reactive protein) (non-HS) | WNL | |
| Calprotectin, Fecal | WNL | |
| ESR (Sedimentation Rate, Modified Westergren) | WNL | |
| Lactoferrin, Quantitative, Stool | WNL | |
| Occult Blood, Fecal, Immunoassay | ||
| parietal cell ABs (APCA) | WNL | |
| IBS | WNL |
Visit 4 (day 60)
Subjective Assessment:
- Herbal Abx Allicillin and Oregano: tolerated, but no major improvement as reached peak improvement from the initial program at last visit.
- Is no longer using Benadryl.
- All improvements maintained from the last visit.
- Improved:
- Gas, diarrhea, red cheeks, abd pain, eczema, mood swings
- Food sensitivities
- Same:
- N/A
Impression:
- Moriah has maintained her peak level of improvement from the last visit, and may have improved slightly from Habx today, but minimally. Since she responded so well to initial program of reduced histamine, lactate, and FODMAP, further Habx are not needed today. Will stop Habx today and then FU in 6-8 weeks and start in on dietary reintro followed next by program curtail. Will not retest due to age. Will test vitamin D today per request of other doc who is treating with high dose vitamin D.
Recommendations:
- Stop the antimicrobials
- Continue previous plan
- Low histamine diet
- Nutritional Support: vitamin D/K
- GI: Digestive enzyme, acid and bile blend; Vitamin C
- FU: 6-8 weeks
Dr. Ruscio’s Comments
Moriah was a great case that illustrated how impactful the identification and management of histamine intolerance and elevated D/L-lactate can be when treating SIBO. These can often co-present with SIBO. It is also very important to mention that the histamine intolerance and high D/L-lactate were determined without lab testing.
Also, recall most of the benefit was from diet and not from the addition of herbal Abx. Why did the diet seem particularly effective here? Moriah’s mom noticed that when she started Moriah on the low histamine diet, it required her to cut out many high histamine foods that she kept trying to feed Moriah because she read about how ‘healthy’ they were. This mostly included soups and fermented foods.
The next step is to keep Moriah on this plan for a couple months, and then gradually work into a reintroduction. She will likely be able to eat many more foods, but will do best if she avoids drifting back to a high histamine diet. After this, we will work to reduce her supplements, and hopefully get her on nothing in the long term.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!