Practitioner Research Review – November 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
![]()
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Adrenal fatigue does not exist: a systematic review.
https://www.ncbi.nlm.nih.gov/pubmed/27557747
Study Purpose:
- To assess if fatigue or energy levels have a correlation to cortisol levels.
Intervention:
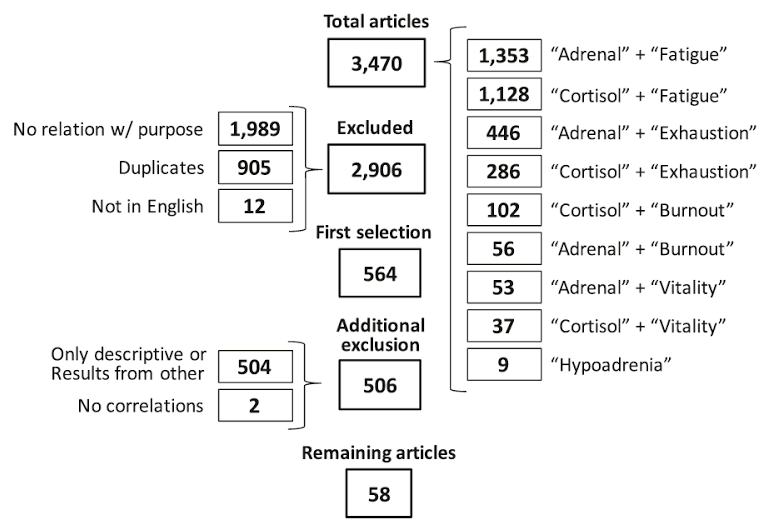
- A systematic review of the literature, 58 studies
- If you have a look at this table, you can appreciate how much work goes into a systematic review. 3,470 articles came up in the researcher’s initial search. Then, after excluding for irrelevant or poor quality studies, 58 high quality studies remained.
Main Results:
- In short, cortisol testing shows a poor correlation to fatigue irrespective of testing methodology used.
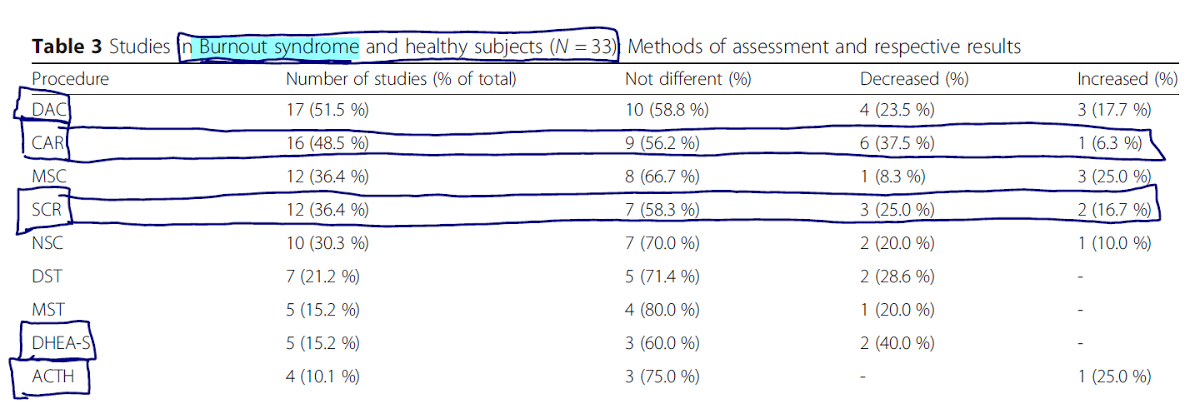
- By far “the most assessed exams (aka most studied tests) were ‘Direct Awakening Cortisol’ (n=29), ‘Cortisol Awakening Response’ (n=27) and ‘Salivary Cortisol Rhythm’ (n=26).”
- Abbreviations DAC, CAR, SCR
Cortisol Awakening Response (CAR) results summary
- In fatigued but otherwise healthy populations, approximately
- 50% of studies showed normal tests, 25% of studies showed diminished response, and 15% of studies showed heightened response.
- “Among the 27 studies that employed CAR, fourteen (51.9 %) showed a normal response, nine (23.3 %) had a diminished delta cortisol, and four (14.8 %) demonstrated an increased delta cortisol.”
- Note: “Delta cortisol is the difference between two measurements at waking and again 30 min later,” as this is not usually measured in FM salivary cortisol kits.
- 50% of studies showed normal tests, 25% of studies showed diminished response, and 15% of studies showed heightened response.
Salivary Cortisol Rhythm (SCR) results summary
- In fatigued but otherwise healthy populations, approximately
- 60% of studies showed normal results, 25% of studies showed impaired rhythm, and 11% of studies showed impaired production.
- Sixteen (61.5 %) studies showed no difference between fatigued and control patients, whereas seven (26.9 %) demonstrated an impaired decrease in the circadian SCR. The remaining three (11.6 %) studies disclosed a more pronounced decrease in cortisol level.
- *Note: this was usually run as a 3 point test.
- 60% of studies showed normal results, 25% of studies showed impaired rhythm, and 11% of studies showed impaired production.
Direct Awakening Cortisol (DAC) results summary
- In fatigued but otherwise healthy populations, approximately
- 65% of studies showed normal results, 14% of studies showed elevations, and 20% of studies showed reduced response.
- “inconsistent results were observed: normal results were found in nineteen (65.5 %) studies, elevated levels were shown in four (13.8 %), and reduced levels in six (20.7 %)”
- 65% of studies showed normal results, 14% of studies showed elevations, and 20% of studies showed reduced response.
Other testing methods results summary
- In fatigued but otherwise healthy populations, approximately:
- ACTH testing
- 83% of studies found no correlation.
- ACTH stimulation testing
- 33% of studies (1 study) showed increased response, and 67% of studies (2 studies) showed decreased response.
- *This 67% supports concept of adrenal fatigue.* However, it was found in 2 studies.
- 24 hour urinary free cortisol
- One of three studies found no correlation. Two of these three found decreased cortisol in fatigued subjects.
- DHEA-S
- Four studies (66.7 %) found no correlation with DHEA-S, whereas two (33.3 %) found lower levels in chronic exhausted patients.
- A few other, less commonly used methods, were assessed.
- Generally speaking, 50-80% of the time testing had no correlation to fatigue.
Cortisol testing in those with Burnout Syndrome:
- See table below – essentially over 50% of the studies found no difference in cortisol testing results in those with Burnout Syndrome.
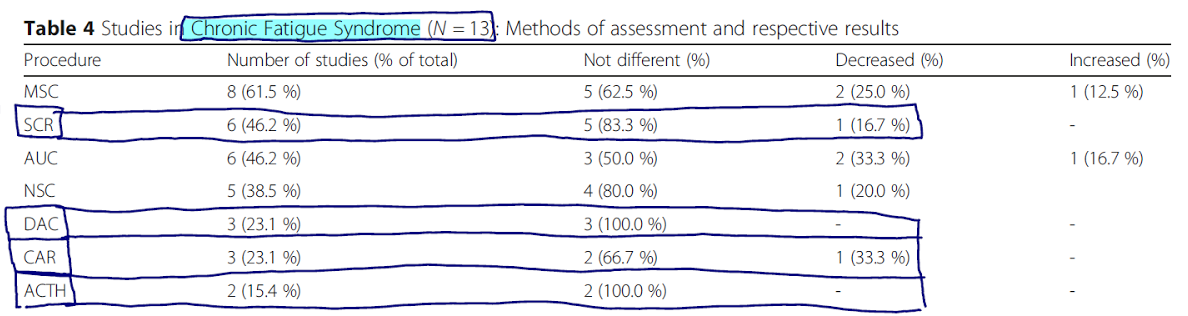
Cortisol testing in those with Chronic Fatigue Syndrome:
- See table below – essentially over 65% of the studies found no difference in cortisol testing results in those with Chronic Fatigue Syndrome.
Additional Results:
- The gold standard for assessing HPA axis function is either the insulin tolerance test or the LPS stimulation test. Neither of these were tested to correlate findings to fatigue.
- The term burnout might be a far better term for the field to be using for a few reasons. It’s what is more often used in the scientific literature:
- “Despite the widespread use of the term ‘adrenal fatigue’ by the general media and certain health practitioner groups, in this systematic review, only ten citations [113–122] were found with this exact expression and they were all only descriptive and did not perform any test regarding the HPA axis and ‘adrenal fatigue’. Studies that tried to correlate the HPA axis and fatigue states used the term ‘burnout’ instead of ‘adrenal fatigue’ to denote adrenal depletion.”
- Popular questionnaires, like that of Dr. Wilson, have not been validated and are not used anywhere in the scientific literature.
Authors’ Conclusion:
- “This systematic review proves that there is no substantiation that ‘adrenal fatigue’ is an actual medical condition.”
Interesting Notes:
- The authors offer the following DDX when considering “adrenal fatigue”
- “(1) sleep obstructive apnea syndrome; (2) adrenal insufficiency; (3) mental illnesses; (4) excessive working (overwork); (5) night-shift workers; (6) other hormonal deficiencies; (7) liver and kidney dysfunctions; (8) heart conditions; (9) chronic pulmonary obstructive disease; (10) autoimmune diseases.”
Clinical Takeaways:
- Adrenal fatigue and the corresponding correlation between fatigue and cortisol levels is not supported.
- Clinicians should focus on the underlying cause of symptoms (lifestyle, diet, gut health, inflammation, thyroid, male/female hormones, infection, etc.…) and forgo adrenal assessments.
- Burnout Syndrome might be a better term to use and to study to help our fatigued patients.
Dr. Ruscio’s Comments
You have likely heard me say I do not perform adrenal testing in my clinic. This study reinforces a major reason why; the test results and the patients often do not match. Fatigue is a very real thing, however looking to an adrenal test to resolve the fatigue may be misguided.
Also, keep in mind adrenal testing did not correlate with fatigue when assessing cortisol via multiple types of tests… so it’s likely not the test’s fault, but rather the issue is the condition we are trying to diagnose doesn’t exist.
What is also interesting is the finding that in chronic fatigue syndrome over 65% of studies show no correlation between fatigue and adrenal testing. This, to me, is a good reminder that fatigue is not solely an endocrine phenomenon.
Burnout Syndrome might be a far better label for what we are trying to describe. There are some very impressive data here. Also, it suggests that the patient needs to reduce their stress load (which could include internal stress), instead of ‘treating adrenal fatigue.’
Intestinal dysbiosis and probiotic applications in autoimmune diseases.
https://www.ncbi.nlm.nih.gov/pubmed/28556916
Study Purpose:
- Assess relationship between intestinal dysbiosis, probiotics, and autoimmune disease.
Intervention:
- Review, non-systematic
Main Results:
Association Data (Type 1 Diabetes)
- As you can see below, it’s hard to take much away from association data. This is why I caution against making treatment decisions based upon association data.
- “T1D children had decreased microbiota diversity compared with controls and had a reduction in the Firmicutes/Bacteroidetes ratio.”
- “Murri and colleagues (2013) evaluated the gut microbiota in a cohort of 16 T1D children and 16 controls and showed an increased abundance of Clostridium, Bacteroides and Veillonella in patients compared with controls. Furthermore, the Firmicutes/Bacteroidetes ratio and levels of Lactobacillus, Bifidobacterium, and Prevotela were decreased in these patients.”
- “Davis-Richardson and colleagues (2014) evaluated stool samples isolated from 29 seroconverted T1D-disease and 47 healthy controls and observed a high abundance of Bacteroides dorei and Bacteroides vulgatus in seroconverted T1D patients eight months prior to B-cell autoimmunity.”
- “Kostic and colleagues (2015) evaluated stool samples from 33 children genetically predisposed to T1D and reported alterations in microbiota alpha-diversity between and within the children over time.”
- “They also observed a decrease in the number of Gram-negative members and an inverse correlation between Lachnospiraceae and Ruminococcaceae with Enterobacteriaceae, a Gram-negative aerobe. In addition, they reported that early commensals are aerobic, whereas later microbes appear to be anaerobic.”
- Note: one study did show that treatment with insulin normalized the gut microbiota in type 1 diabetic children, so the above changes may not be causal.
- Let’s now focus on the clinical trials detailed in this review.
Probiotics Treatment Data (All Conditions)
- Type 1 Diabetes – Early probiotic administration (before 27 days of age) can decrease the risk of type 1 diabetes.
- “In humans, a TEDDY study group evaluated probiotic supplementation for children with genetic risk for T1D during their first year of life. This multicentre prospective cohort study (United States, Finland, Germany, and Sweden) investigated 7,473 children ranging from four- to ten-years-old in age. Early probiotic administration was correlated with a decreased risk of islet autoimmunity when compared with the group that received probiotics after 27 days of life or no supplementation.”
- MS – Probiotics improved disability, insulin resistance, and inflammatory markers in MS.
- “In humans, Kouchaki and colleagues (2016) reported improved EDSS, insulin resistance and a decrease in inflammatory markers in MS patients treated with probiotic supplementation containing Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus fermentum and Bifidobacterium bifidum. This randomized double-blind placebo-controlled clinical trial analysed probiotic intake for 12 weeks in 60 MS patients.”
- Rheumatoid Arthritis – Mixed data, but trials have shown improvement in disease activity and function.
- “In a double-blind, placebo-controlled trial, the oral administration of Lactobacillus rhamnosus and Lactobacillus reuteri for three months to 29 RA patients did not improve the disease, measured by the ACR20. However, the authors reported functional improvement within the probiotic supplementation group compared with the placebo group.”
- “Vaghef-Mehrabany and colleagues (2014) investigated the role of Lactobacillus casei intake in 46 RA patients for eight weeks. This randomized, double-blind placebo-controlled trial showed improvement in disease activity score, increased levels serum IL-10, and decreased levels of TNF, IL- 6 and IL-12 in treated patients.”
- “Another clinical trial with the same study design evaluated the administration of Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium bifidum for eight weeks in 60 RA patients. Probiotic intake improved DAS28.” (DAS28 is a disability index).
Additional Results:
- “Intestinal dysbiosis observed in autoimmune diseases is associated with decreased bacteria function and diversity, impaired gut barrier function, increased inflammation and decreased Treg cells in the gut.”
Authors’ Conclusion:
- “Emerging findings associate intestinal dysbiosis with autoimmune diseases pathogenesis.”
Interesting Notes:
- “In humans, the intestinal microbiota tends to stabilize and reaches greater diversity at approximately three years of age…”
- “The most prevalent genera in the adult human gut are represented by Gram-positive bacteria, such as Clostridium, Bifidobacterium, Lactobacillus, Ruminococcus, Streptococcus, and Gram-negative bacteria, such as Bacteroides and Escherichia.”
Clinical Takeaways:
- Dysbiosis may be involved with autoimmune disease, and treatment of dysbiosis may improve autoimmunity.
- Probiotics may prevent type one diabetes when administered before 27 days of age.
- Probiotics may improve disability and/or disease activity in MS and RA and are worth a therapeutic trial…
- …using a formula containing a mixture of Lactobacillus and Bifidobacterium strains.
Dr. Ruscio’s Comments
More data being published showing the importance of gut health in autoimmunity.
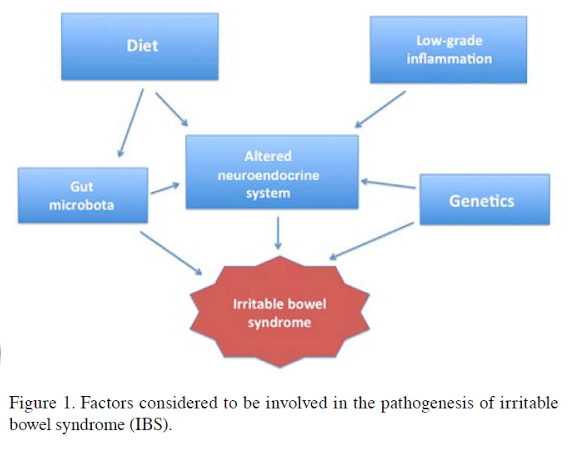
Effect of diet and individual dietary guidance on gastrointestinal endocrine cells in patients with irritable bowel syndrome (Review).
https://www.ncbi.nlm.nih.gov/pubmed/28849091
Study Purpose:
- To review the impact of diet on the intestinal endocrine cells in IBS.
Intervention:
- Review, non-systematic
Main Results:
- Intestinal endocrine cells are different in those with IBS compared to healthy controls.
- “…the densities of different types of GI endocrine cells in the different parts of the GI tract are abnormal in patients with IBS.”
- These differences affect motility and pain reception.
- “Such alterations are responsible for abnormal functions of the GI tract, such as visceral hypersensitivity, dysmotility and abnormal secretion, all of which are characteristics of IBS.”
- “The GI endocrine cells are scattered among the epithelial cells lining the GI lumen (61,119-121). They comprise almost 1% of all epithelial cells in the GI tract and are considered to be the largest endocrine organ in the body.”
- These intestinal endocrine cells sample the intestinal contents and release hormones in response.
- “The GI endocrine cells project specialized microvilli into the GI lumen to sense the luminal contents (mainly nutrients) and release specific hormones into the lamina propria.”
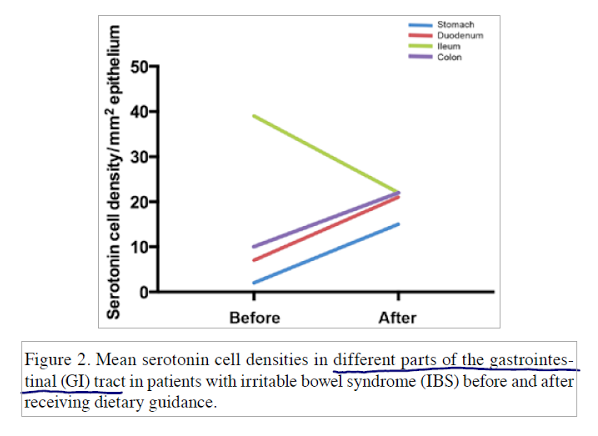
- A low FODMAP diet can lead to a normalization (increase) in serotonin (and other cells) cell density in IBS patients.
- ‘the densities of cells are abnormal in the stomach, duodenum, ileum and colon of patients with IBS, and dietary guidance tends to change these densities toward the values measured in healthy control subjects.’
- “The densities of serotonin cells in the duodenum and ileum changed significantly… toward that measured in healthy control subjects.”
Additional Results:
- The low FODMAP diet may be less helpful for constipation compared to diarrhea.
- “IBS symptom questionnaire, improve significantly after receiving dietary guidance, particularly the symptoms of pain (52,166) and diarrhea (166), but not constipation”
- IBS patients may have higher levels of commensal bacteria that are responsible for fermentation of FODMAPs and fiber.
- “The gut microbiota in patients with IBS comprises fewer Lactobacillus and Bifidobacterium spp. and more Clostridium spp. that ferment FODMAPs and fiber and produce gas, leading to luminal distension with symptoms of abdominal pain and bloating (93-95).”
- “Patients with IBS tend to have low intakes of calcium, potassium, magnesium, vitamin A, vitamin B12 and vitamin B2.”
Authors’ Conclusion:
- “Providing individual dietary guidance about a low FODMAP intake, high soluble‑fiber intake, and changing the proportions of protein, fat and carbohydrates helps to reduce the symptoms experienced by patients with IBS and to improve their quality of life. These improvements are due to restoring the densities of the GI endocrine cells back to normal. The reported observations emphasize the role of GI endocrine cells in the pathophysiology of IBS and support the provision of dietary guidance as a first‑line treatment for managing IBS.”
Interesting Notes:
- Over 90% of IBS patients will react to problematic foods within 3 hours of ingestion.
- “The time delay between the consumption of food until the appearance of IBS symptoms varies, with 28% of patients experiencing symptoms within 15 min of eating, and 93% reporting that the symptoms become more severe between 15 min and 3 h.”
- “The estimated prevalence of IBS ranges between 5 and 20% of the population worldwide.”
- While IBS does not contribute to death or develop into more serious conditions, the accompanying morbidity can rival that of serious diseases with considerable costs to society.
- “It is known that IBS neither increases mortality (40) nor develops into serious diseases, such as cancer or inflammatory bowel disease (41,42). However, the morbidity associated with IBS can be as serious as that for major chronic diseases, such as congestive heart failure (43), hepatic cirrhosis (44), renal insufficiency and diabetes (11), with considerable costs to society (17,45-48). Patients with IBS tend to be less productive at work or school due to frequent absences (6,13,36,49,50), changing or losing jobs and turning down promotions.”
- Soluble fiber is better for IBS than insoluble fiber.
- “Fiber has been used as a bulking agent in the treatment of IBS (74,96). Consuming water‑soluble fiber tends to improve the symptoms of IBS compared to consuming water-insoluble fiber (74,97‑99). Indeed, consuming water‑insoluble fiber may actually worsen the symptoms of IBS (74,97) by causing increased bloating and abdominal discomfort (100). For example, it is recommended for patients with IBS to consume psyllium (mostly water‑soluble fiber) rather than bran (water‑insoluble fiber) in order to alleviate their symptoms (100).
Clinical Takeaways:
- A low FODMAP diet may repair the changes in the intestines that cause IBS.
Dr. Ruscio’s Comments
Very important findings in this review. They suggest that a low FODMAP diet could repair changes in the intestinal endocrine that underlie IBS. This is especially important when having a conversation with a patient that is concerned that a low FODMAP diet will ‘damage their microbiota.’
We have clear clinical trial evidence which shows a low FODMAP diet is effective for IBS. This review now adds exciting mechanism data which imply that improved health of the intestines might be why the diet works so well.
The diet used was a low FODMAP diet that also increased protein and reduced fat and insoluble fiber. Does this mean this exact diet must be followed to produce these results? In my opinion, no. I say this because there are many other studies which have used a standard low FODMAP and produced the same symptomatic improvement. I have reached out to the author and will hopefully be able to pick his brain more on this soon.
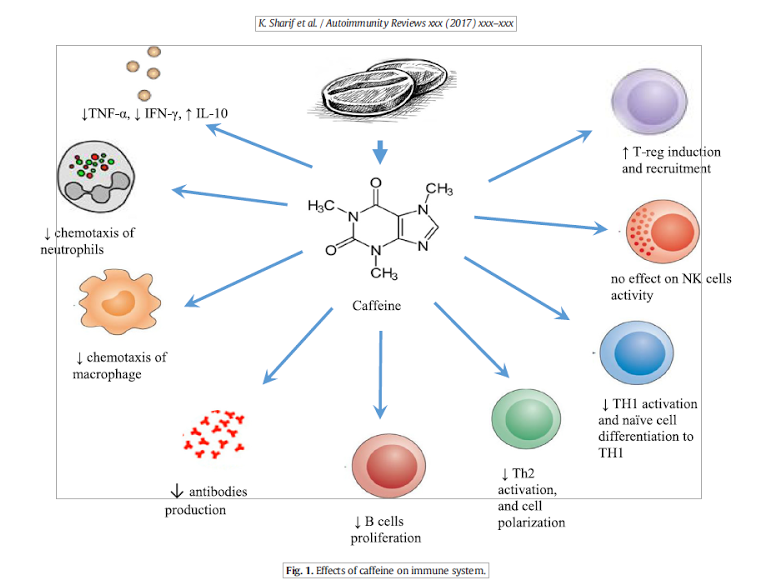
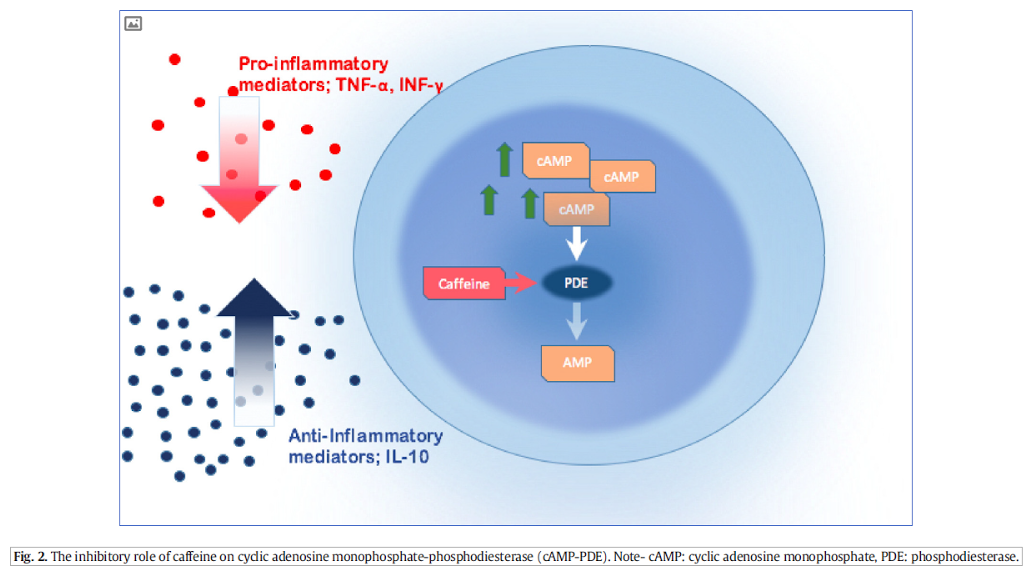
Coffee and autoimmunity: More than a mere hot beverage!
https://www.ncbi.nlm.nih.gov/pubmed/28479483
Study Purpose:
- Assess the impact of coffee on autoimmune conditions and the immune system.
Intervention:
- Review, non-systematic
Main Results:
Impact on autoimmune diseases
- Coffee may increase risk of
- Rheumatoid arthritis
- Type I diabetes
- Latent autoimmune diabetes in adulthood (LADA) aka ‘type 1.5 diabetes’
- Coffee may decrease risk of
- Ulcerative colitis
- Multiple sclerosis
- Coffee appears to have no effect on
- Lupus
- Psoriasis
- Crohn’s disease
- Celiac disease risk
- No good data on thyroid AI
Other effects of coffee
- Cross reactive with gluten – may increase celiac disease activity.
- *Very important* When digging into the details regarding the above point, it appears that only instant coffee reacts, because it is often contaminated with gluten. When non-instant, regular coffee or espresso was tested there was no reactivity.
- “Anti-gliadin bounded with gliadin at 100% rate. In comparison, anti-gliadin reacted with two different instant coffee preparations at a rate of 23%, both of which were made from Arabica coffee beans.”
- “Espresso preparation as well as Turkish and Israeli prepared coffee did not show any reaction with anti-gliadin. Therefore, it appears that pure coffee is safer than instant coffee preparations for patient with celiac disease.”
- Decreases Levothyroxine absorption.
- Decreases insulin sensitivity.
- Decreases response to Methotrexate in RA treatment.
Additional Results:
- “Caffeine acts in an anti-inflammatory way on multiple components of the immune system.”
- While the data are not consistent, some large studies have shown an overall decreased risk of death with coffee consumption.
- “Many scientific evidences showed that coffee consumption (either caffeinated or decaffeinated) was significantly inversely associated with total mortality in large population-based studies.”
- https://www.ncbi.nlm.nih.gov/pubmed/21432699
- https://www.ncbi.nlm.nih.gov/pubmed/16507475
Authors’ Conclusion:
- “Coffee consumption has an immunomodulatory action and is postulated to induce an anti-inflammatory state.
- Coffee intake has been shown to increase the risk of RA and T1DM occurrence, while decreasing the risk of PSC and MS development.
- MS patients could benefit from coffee consumption due to its role in mitigating disease progression.
- Hashimoto’s disease patient on levothyroxine supplementation therapy should avoid concomitant coffee consumption due to the possible impact on drug absorption.
- It might be advantageous for RA patients treated with methotrexate to avoid coffee consumption because of its postulated impact on drug efficacy.
- Celiac patients who have clinical symptoms albeit adhering to a gluten-free diet may improve after replacing their coffee preparations with blends characterized by lower reactivity with anti-gliadin peptide, for example espresso.
- T1DM patients should decrease their coffee consumption due to their lowered insulin sensitivity and impaired glycemic control.”
Interesting Notes:
- Coffee contains compounds that are health promoting.
- “Caffeine, for example, besides being the most frequently ingested psychoactive molecule [1], has important anti-apoptotic effects. Moreover, coffee contains lipidic molecules, like cafestol and kahweol, and antioxidant substances, such as polyphenols [2], which have an indispensable role in scavenging free radicals as well as in inducing the activation of DNA repair and detoxification enzymes [2]. In addition, coffee includes many anti-mutagens that prevent malignant cell transformation leading to a decrease in the risk of developing colorectal cancer, liver, renal, pancreatic cancer as well as other solid tumors”
- However, it also contains some unhealthy compounds.
- “On the other hand, coffee contains some carcinogens, like glyoxal, methylglyoxal, ethylglyoxal, propylglyoxal, diacetyl, acetol and other dicarbonyls and tannin, among others, which could counteract the positive effects of anti-mutagens.”
- Here are two interesting diagrams from the study. When looking at all these mechanisms, one might easily conclude that anyone with an AI condition should drink coffee… However, this is why looking to the outcome data is so important. Irrespective of these mechanisms, the outcome data shows coffee increases risk of some AI diseases.
Clinical Takeaways:
- See authors’ conclusions above.
Dr. Ruscio’s Comments
Two things here stand out:
- It may only be instant coffee that cross-reacts with gluten, and this appears to be due to contamination in the coffee, not the coffee itself.
- Perhaps we see the increased risk of RA because some with RA have NCGS. Since instant coffee can cross react with gluten, perhaps drinking instant coffee is akin to eating gluten for those with NCGS-fueled RA?
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!