Practitioner Case Study – November 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Adrenal fatigue does not exist: a systematic review.
- Intestinal dysbiosis and probiotic applications in autoimmune diseases.
- Diet’s (Low FODMAP) effect on intestinal endocrine cells in IBS.
- Coffee and autoimmunity: More than a mere hot beverage!
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Nishant, 24yo male
- Previous Dx:
- SIBO and IBS
- Rx:
- N/A
- Chief complaints:
- Gas, bloating, indigestion
- Stomach/colon gurgling and nervous feeling
- Constipation – never feeling completely empty
- Extreme sensations surrounding stomach, goosebumps and chills when stomach problems are bad
- Anxiety, headaches
- Fatigue, brain fog
Visit 1 (day 1) – History and Exam:
Nishant presents as a generally healthy and articulate 24yo male with good lifestyle and diet.
He has GI SS (signs and symptoms) and neuro SS, his GI SS have been minimally responsive to Xifaxin, Flagyl, and HAbx, and responded better to VSL#3 and Citrucel. He has tested + for SIBO 2x and for dysbiosis via Doctor’s Data. Diet has offered only mild relief, low FODMAP/SCD.
He may simply need more follow through on GI and/or to try different treatments: extended Abx, Abx w/ antifungals, different HAbx, elemental diet… Histamine may also be an issue, as might blood sugar regulation. There is a slight chance of other ddx like gastritis or ulcer.
GI MD workup was all normal. Has done some work with ND, but NR to HAbx and gut healing supps.
Prognosis fair to good.
Previous Diets
- Candida diet (no sugar, carbs) – no change, lost weight
- Low FODMAP – slightly helpful
- Low FODMAP w/ SCD – helpful
Previous Treatments
- Citrucel – aids bowels
- Peppermint tea – helps
- HCl – no change
- VSL#3 – helpful
- Enzymes – no change
- Xifaxin 14d – slight help
- Flagyl – no change
- Atrantil – slight help
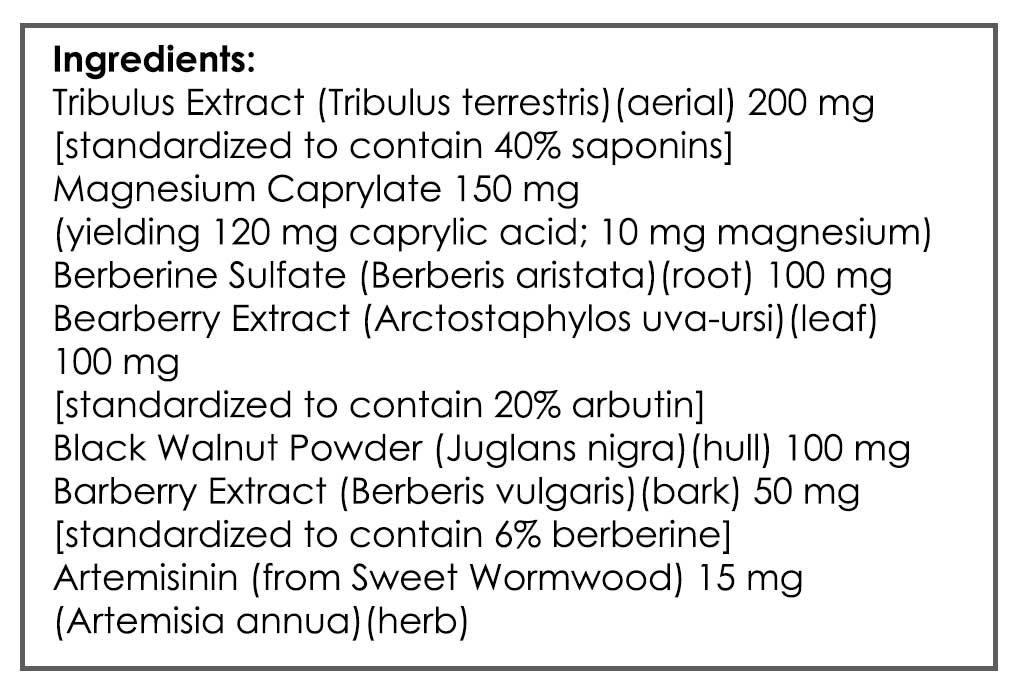
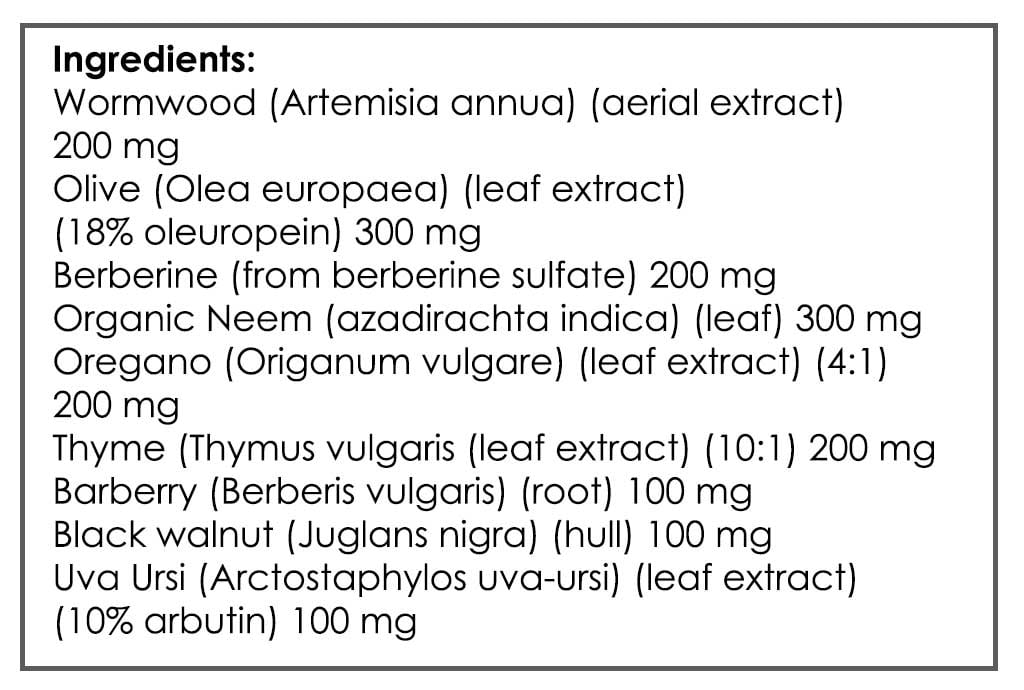
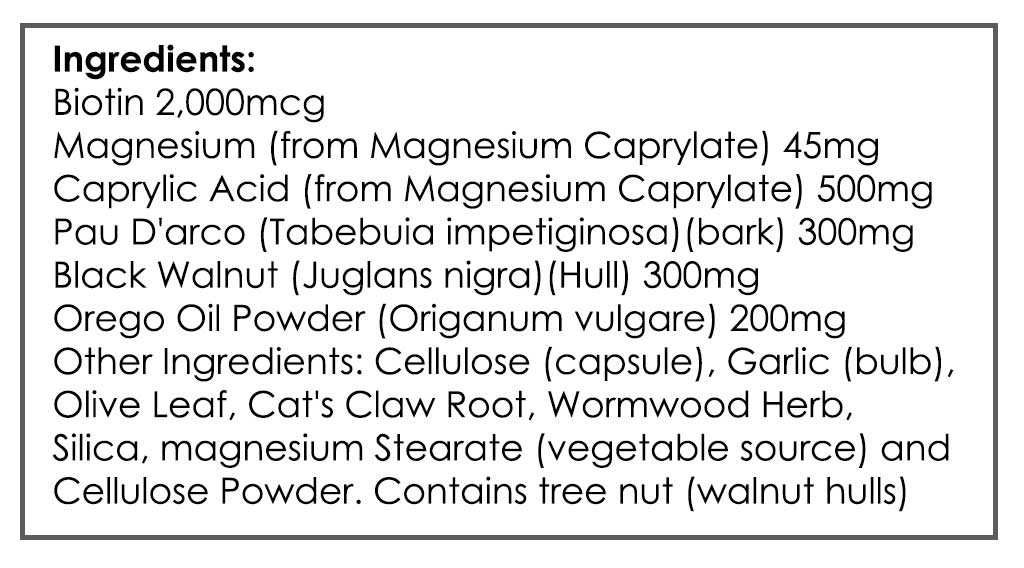
- HAbx (CandaClear Four, Berberine, Neem, Grapefruit Seed Extract) – rxns
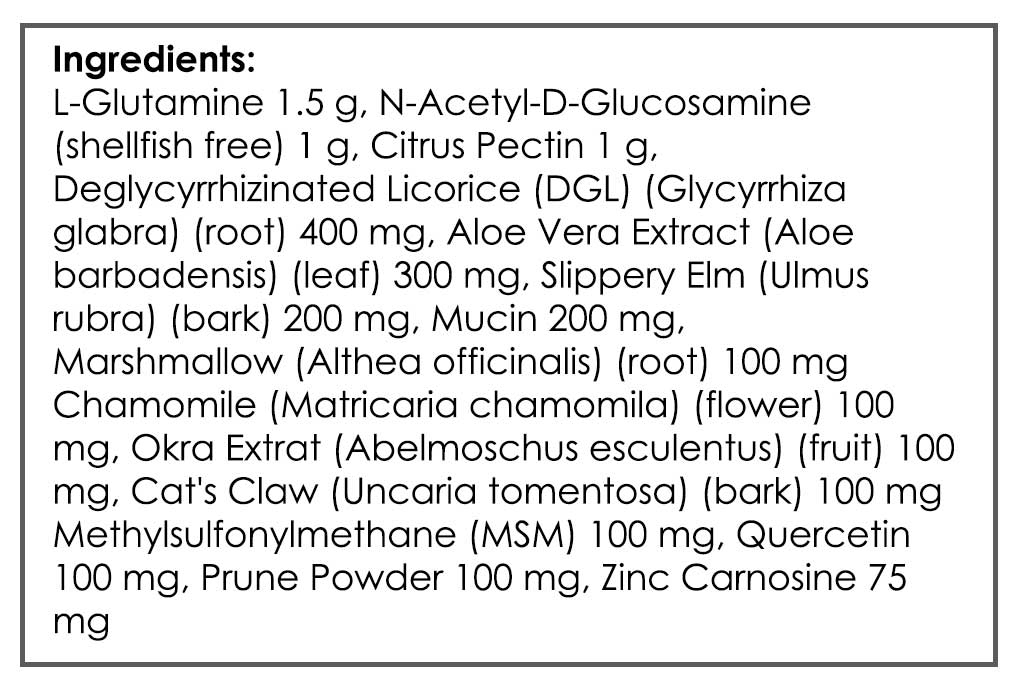
- L-Glutamine/GI Revive – no help
Initial Impression
- Again, Nishant may need more follow-through on his GI care, or different treatments for his GI. Histamine load, blood sugar regulation, and gastric health may also need to be addressed.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests ordered
- Aerodiagnostics Lactulose SIBO breath test
- LabCorp 1 – blood and urine panel (markers to follow)
- LabCorp 2 – GI panel (markers to follow)
- Rationale
- Rule out SIBO relapse and other GI dysbiosis. Also check for hypothyroid, anemia, low vitamin D, etc.…
Recommendations
- For the first week, experiment with low histamine diet, then
- Please perform the Modified Fast for 2-4 days (see website for PDF), then
- Please follow the low FODMAP w/ SCD diet as best you can. You can eat rice, potatoes, and gluten-free bread if they are tolerated to help keep on weight. After 1.5 weeks on this diet, add in the supplements in the program.
- Eat frequent meals, every 3-4 hours.
- Start going to bed before 12 for 1 week.
- Discontinue coffee for 1 month.
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
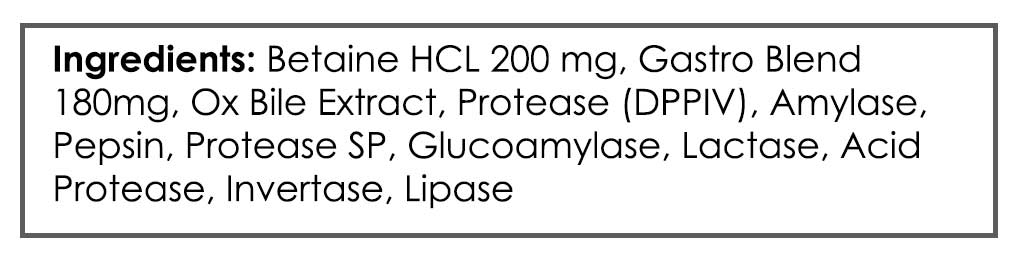
- GI: Enzyme/acid formula, Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
- Rationale
- To evaluate impact of low histamine diet, fasting, and another trial of low FODMAP w/ SCD diet. Also impact of probiotics with enzymes/acid.
Visit 3 (day 30) – Lab Interpretation and Treatment Evaluation
Lab Results:
- See full results below.
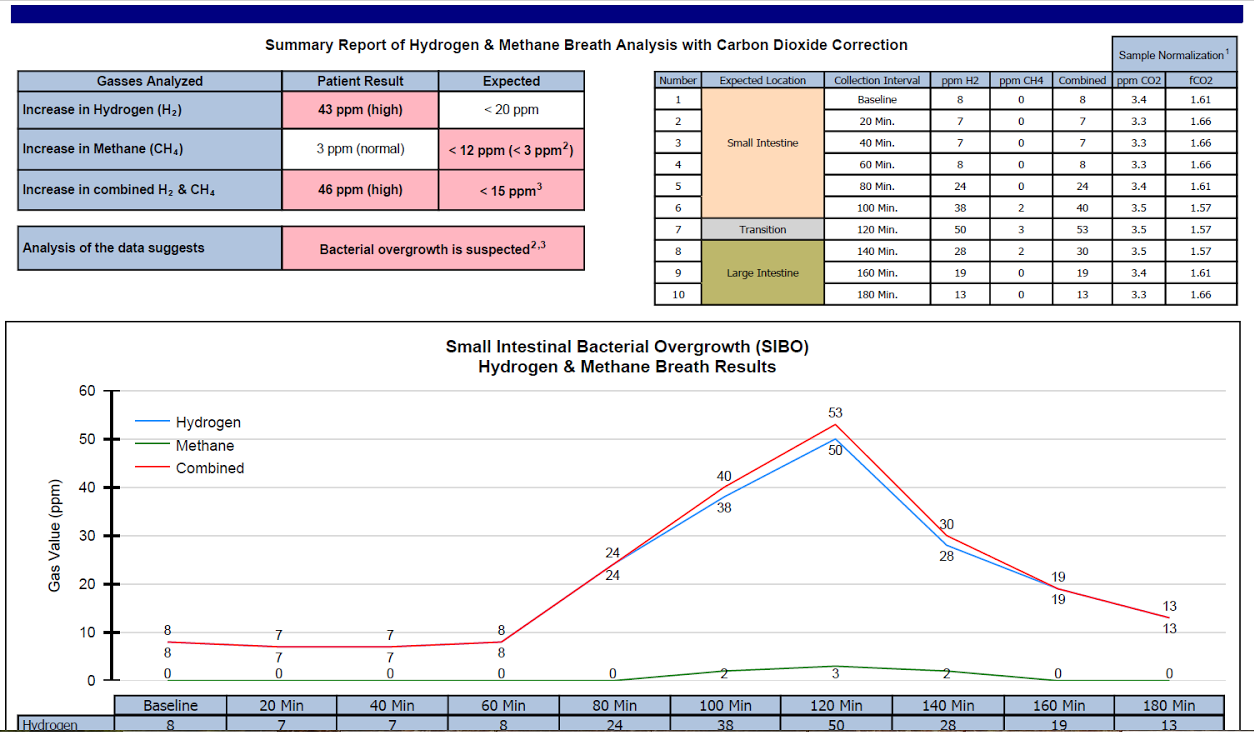
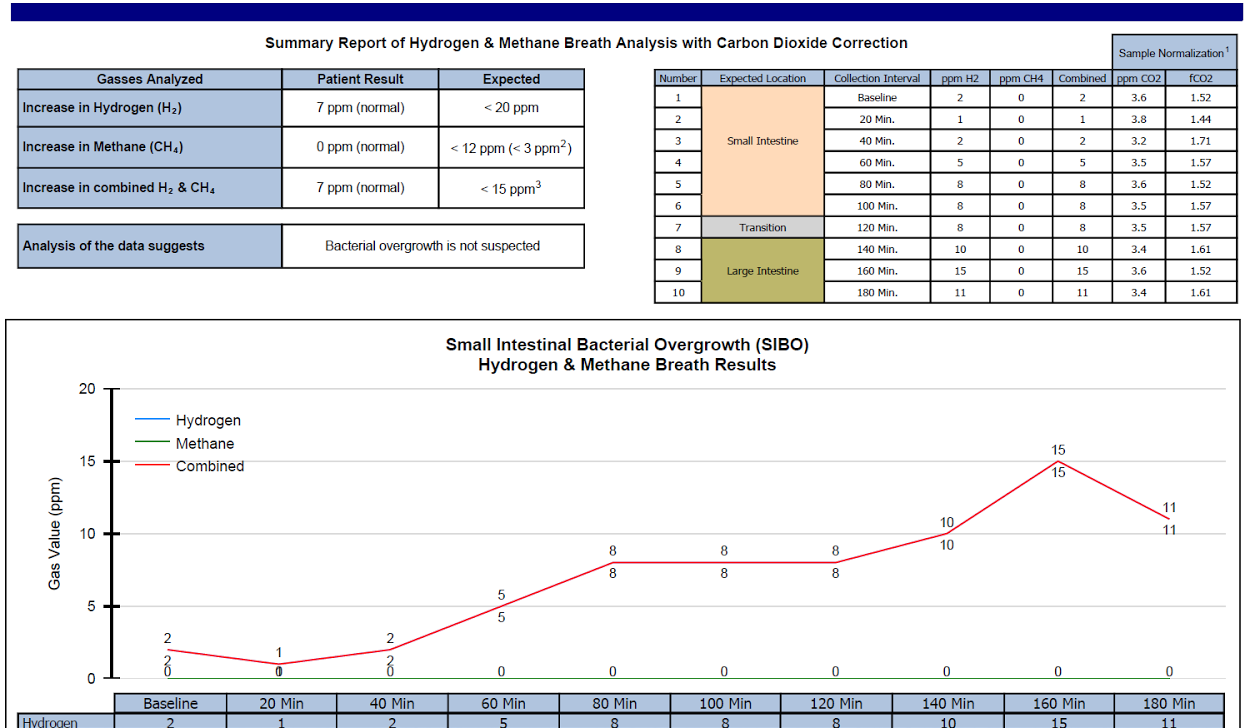
- Dx
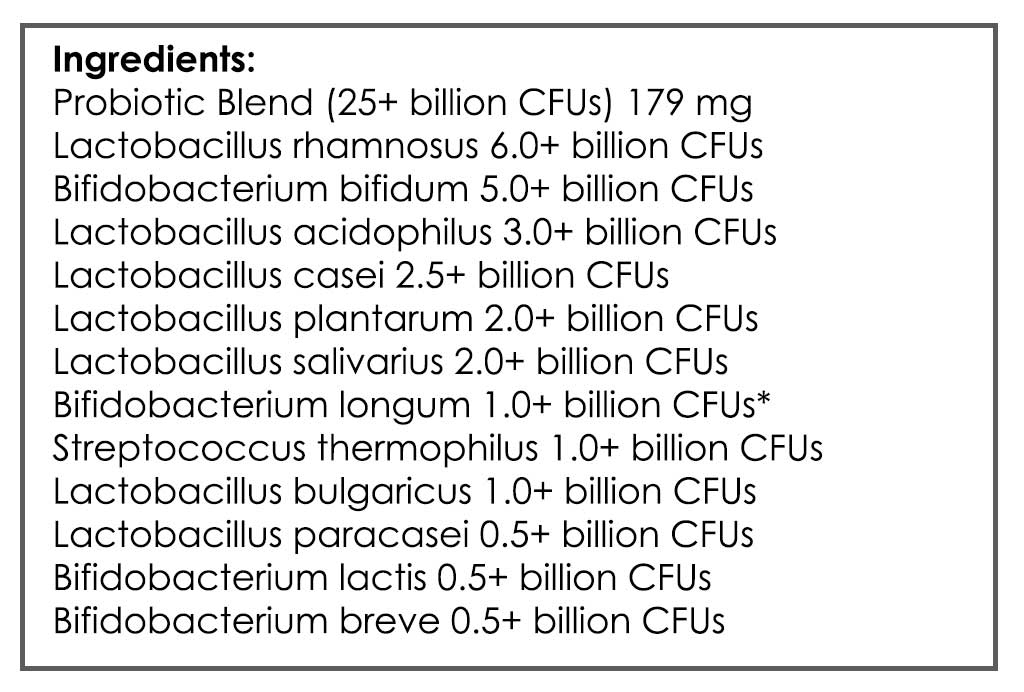
- Moderate hydrogen predominant SIBO. Potential candida or SIFO.
- Summary
- Lactulose SIBO breath test
- H2 64, CH4 7, combo 71
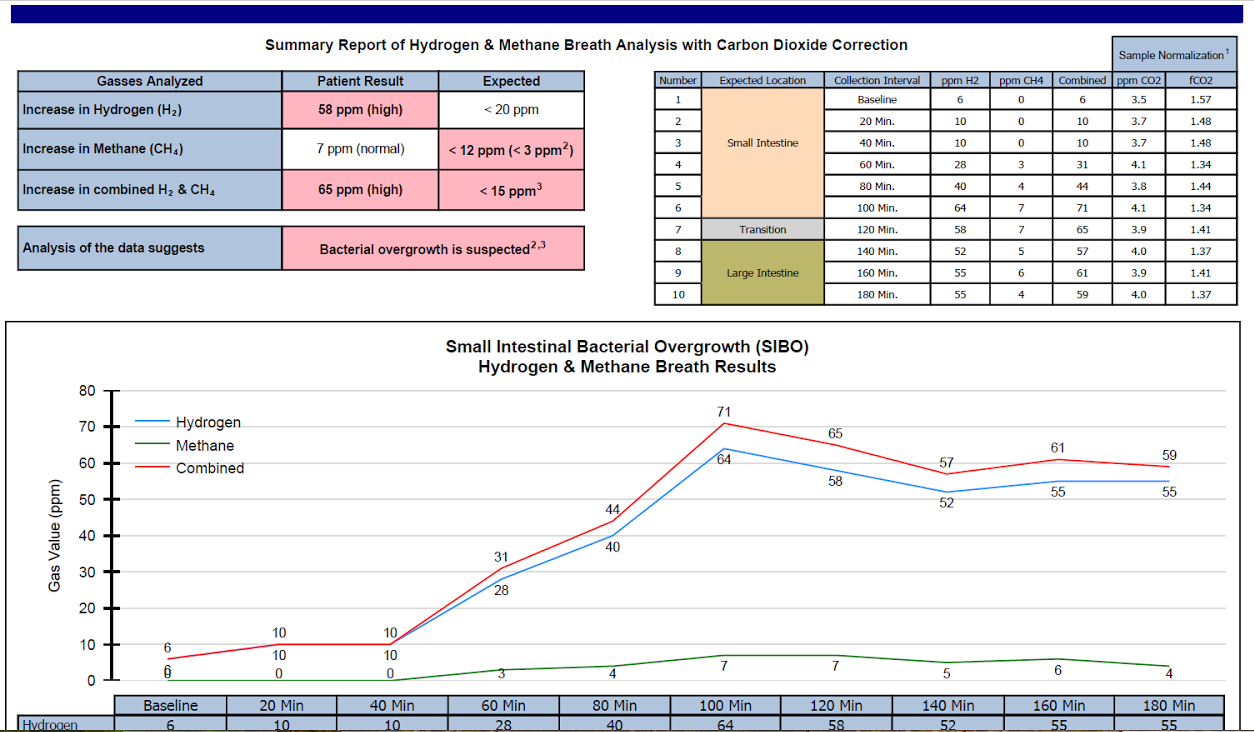
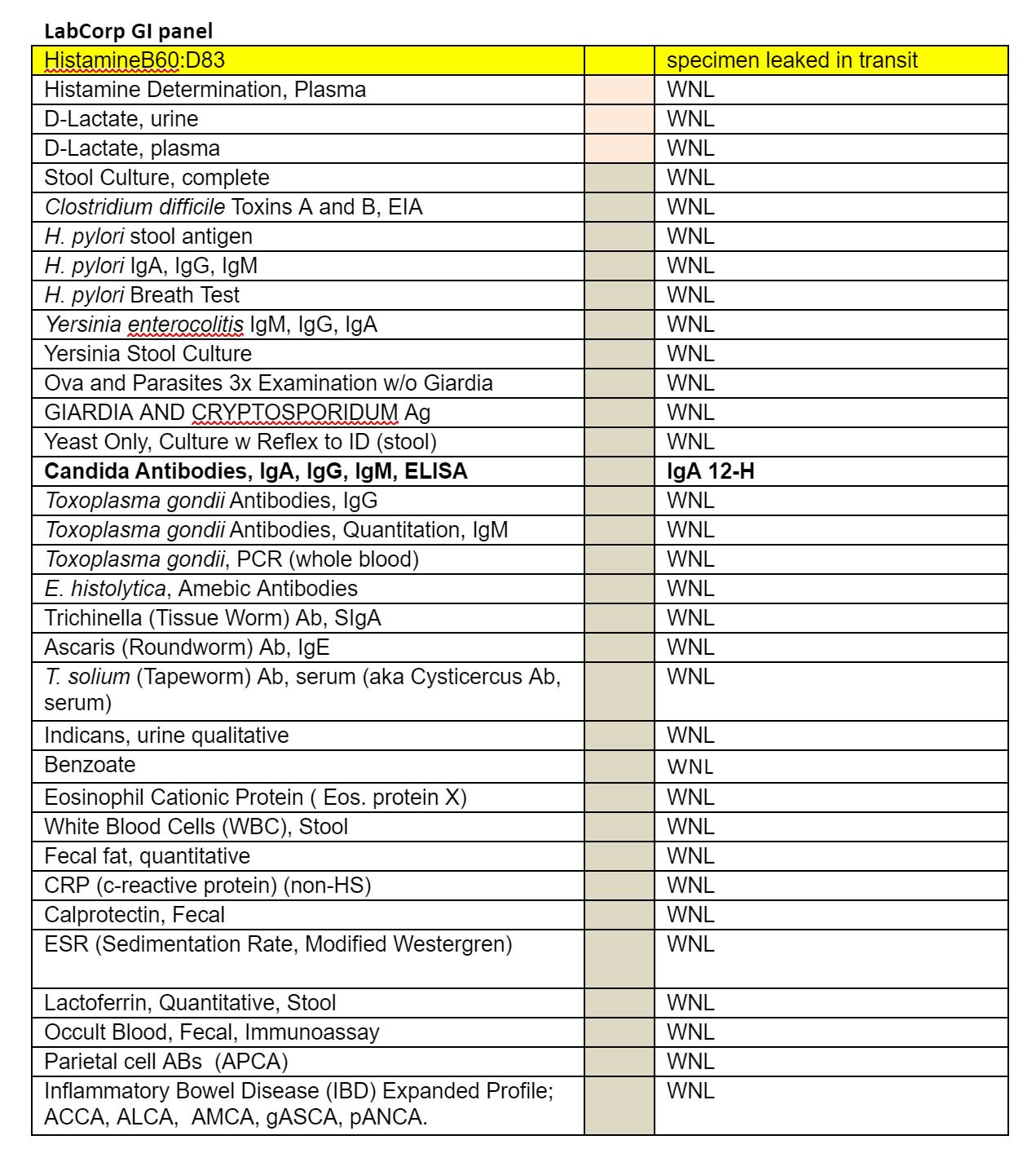
- LabCorp #2 Blood & Urine
- Hemo A1C 5.7-H, Creatinine 1.30-H, Phosphorus 5-H
- LabCorp #1 blood, urine, stool & breath
- Candida Antibodies, IgA, IgG, IgM, ELISA, IgA 12-H
- Lactulose SIBO breath test
Subjective Assessment:
- Low histamine – no change
- Modified Fast (MC 4 days)
- Improved: fatigue, chills/goose bumps, brain fog
- Rxn: bloating, gas
- Low FODMAP w/ SCD (with some CHOs) – helpful
- Coffee avoidance – helped reflux
- Has not yet started on supplemental program
- Improved:
- Fatigue, chills/goosebumps, reflux, brain fog
- Same:
- Gas/bloating/indigestion, headaches
- Worse:
- N/A
Impression:
- 1/11/17 – Nishant is improved today and has responded well to modified fasting and diet. Since Nishant has been previously minimally responsive to HAbx/SIBO Abx, we will explore other treatment options today: elemental diet. Should this fail, we may simply need more/different HAbx/Abx treatment. Mind other ddx also, ulcer chiefly. If using HAbx, use single ingredient, as he did have rxns to HAbx previously. Rifaximin/Fluconazole may be good option. Starting elemental diet today, and he would like to retest SIBO after treatment.
Recommendations:
- When eating food, please continue the low FODMAP w/ SCD diet as best you can. You can eat rice, potatoes, and gluten-free bread if they are tolerated to help keep on weight.
- Continue to try and go to bed before 12 for 1 week.
- Continue to avoid coffee.
- Continue
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
- GI: Enzyme/acid formula, Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
- Starting
- First perform a few weeks on the supplemental program, then
- Perform 2 weeks on the elemental/semi-elemental diet.
- NRT: Whey, and Pea Protein
- Follow up: 4-5 weeks
LabCorp GI panel
Visit 4 (day 60)
Subjective Assessment:
- Low FODMAP/SCD diet – slightly helpful
- Supplement program – slightly helpful
- Semi-elemental diet (SED)
- Rxn: GI turbulence, diarrhea, headaches
- Full elemental diet (ED)- seems more well tolerated
- Overall is slightly improved, but this is confounded by rxns to SED/ED
Impression:
- 2/24/17 – Nishant has improved more today with low FODMAP/SCD and initial supplement program. SED/ED is causing reactions, which we are troubleshooting (by changing form, and taking with oregano). Today we will have him beta test full HAbx should he be non-responsive to oregano alone. If non-responsive, also consider Rifax/Flucon, or other ddx.
Recommendations:
- Continue
- Previous plan
- Elemental/semi-elemental diet – up to 3 weeks in total
- NRT: Whey, and Pea Protein
- Starting
- HAbx (oregano only) during Elemental
- Lifestyle: regular exercise (weight lifting), walking in nature
- Should this not be as effective, you can start on the full anti-microbial program
- If this is effective, transition to hybrid use of the elemental diet
- Perform retesting once complete with exclusive elemental diet
- Follow up: 2 weeks after retesting is performed
- Testing
- Lactulose SIBO breath test
- LabCorp
- Candida antibodies
- Candida stool
Visit 5
Retesting Results
- Aerodiagnostics Lactulose SIBO breath test
- H2 38, CH4 2, combo 40.
- LabCorp
- did not perform – candida retesting
Subjective Assessment:
- Elemental (2 weeks) – was tolerable; helped gas/bloating/indigestion, reflux; fatigued
- Is able to tolerate some coffee
- Then went back to diet, retested, then started slowly onto HAbx
- Hybrid elemental diet – did not use due to cost
- Overall better than at last visit
- Improved:
- Gas/bloating/indigestion (30% better from last visit)
- Gaining weight
- Chills/goosebumps
- Fatigue
- Reflux
- Brain fog
- Same:
- N/A
- Worse:
- Bladder urgency (has had on/off for a while, before starting treatment)
- Night sweats
Impression:
- 3/31/17 – Nishant is continuing to improve (both labs and SS) from full elemental diet for 2 weeks, and then diet with HAbx base protocol. His labs have also improved. Today we will continue on full HAbx since he is just starting, and then at follow up decide to either end after 1 month or continue to full 2 months. He is very meticulous, so mind this and encourage him to reintroduce once he has hit max improvement.
Recommendations:
- Continue previous plan
- When eating food, please continue the low FODMAP w/ SCD diet as best you can. You can eat rice, potatoes, and gluten-free bread if they are tolerated to help keep on weight.
- Continue to try and go to bed before 12 for 1 week.
- Continue to avoid coffee.
-
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
- GI: Enzyme/acid formula, Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
-
- Full HAbx: oregano and herbal blend **4 agents all together
- Lifestyle: regular exercise (weight lifting), walking in nature
- Follow up: 4 weeks
Visit 6
Subjective Assessment:
- Not feeling well – symptoms are about the similar to before starting the ED
- HAbx caused stomach irritation, which then subsided
- Has now been on full dose of HAbx for 3 weeks
- Improved:
- Gas/bloating/indigest, acid reflux, fatigue (improved relative to baseline, but still present and debilitating occasionally though)
- Goosebumps correlating with stomach problems
- Same:
- Fatigue
- Worse:
- Headaches
Impression:
- 5/3/17 – Nishant is regressing today, and might be due to Rxn to HAbx, which he has reported in past. Today will finish 2nd month HAbx and then perform retest SIBO and candida. Consider other ddx also: gastritis/ulcer; another trial of low hist.
Recommendations:
- Continue previous plan
- When eating food, please continue the low FODMAP w/ SCD diet as best you can. You can eat rice, potatoes, and gluten-free bread if they are tolerated to help keep on weight.
- Continue to try and go to bed before 12 for 1 week.
- Continue to avoid coffee.
-
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
- GI: Enzyme/acid formula, Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
-
- Full HAbx: oregano and herbal blend
- Lifestyle: regular exercise (weight lifting), walking in nature
- Starting
- Start taking your antimicrobials with food
- Use the lowest end of the probiotics dose range
- Wait 1 week until starting on these recommendations and then experiment with modified fasting using bone broth or water fasting as an intermittent fast
- Retesting
- Aero SIBO
- Previous LC candida antibodies
- Candida Antibodies, IgA, IgG, IgM, ELISA
Visit 7
Retesting Results
- Aerodiagnostechs SIBO
- H2 8, CH4 0
- Previous LabCorp Candida Antibodies
- not performed
Subjective Assessment:
- HAbx w/ food – helped stomach
- HAbx base 2nd month – NR
- Did not fast b/c fearful of reactions
- Improved:
- Fatigue
- Knot in stomach (after coming of HAbx)
- Same:
- Gas/bloating/indigestion
- Chills/goosebumps
- Headaches
- Brain fog
- Worse:
- Acid reflux
- Food reactivity
Impression:
- 6/21/17 – Today’s labs show SIBO cleared; since we treated with HAbx, this has likely addressed any SIFO, but LC retesting not performed to aid in interpretation. In spite of improved labs, Nishant is minimally improved today, so SIBO likely wasn’t main or only issue. Also, is exhibiting SS that support ulcer/gastritis, so today will start on 1) a trial of herbal upper GI prokinetic and 2) 2 different natural acid lowering compounds and 1 gut repair formula. Will also start food reintro.
Recommendations:
- Continue previous plan
- When eating food, please continue the low FODMAP w/ SCD diet as best you can. You can eat rice, potatoes, and gluten-free bread if they are tolerated to help keep on weight.
- Continue to try and go to bed before 12 for 1 week.
- Continue to avoid coffee.
-
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
- GI: Enzyme/acid formula, Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
-
- Lifestyle: regular exercise (weight lifting), walking in nature
-
- Use the lowest end of the probiotics dose range
- Starting
- Stop full HAbx: oregano and herbal blend
- Stop the digestive acid/enzyme formula
- If you elect to start your food (FODMAP/SCD) reintroduction, do so before you start today’s protocol
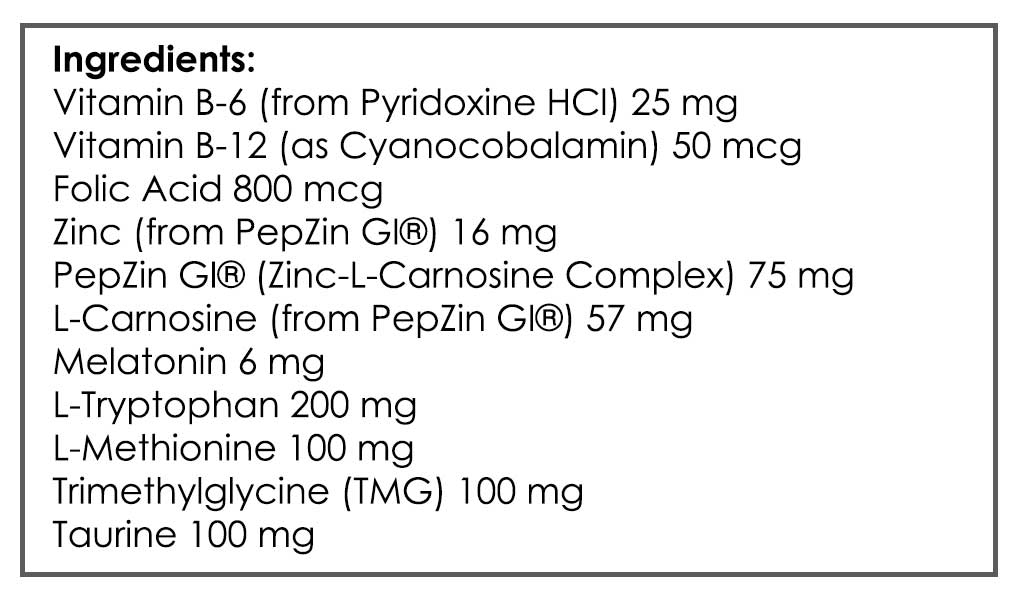
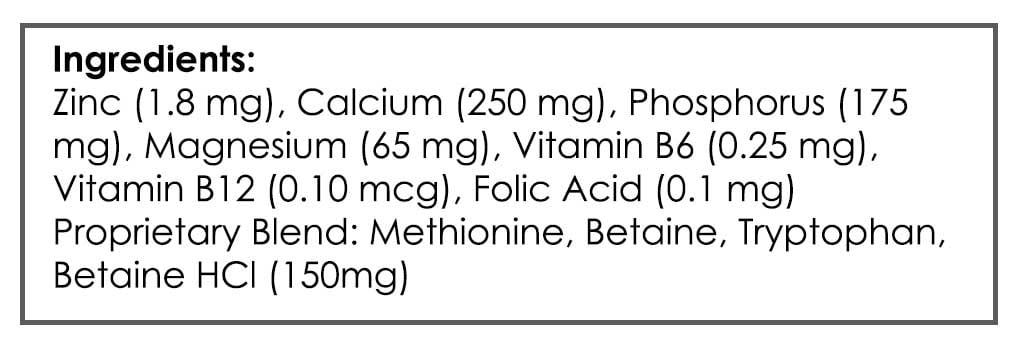
- GI: GI soothing compound, 2 natural acid lowering compounds
- I know you’re dying to know what the exact compounds are here, however it is irrelevant once you read the next visit. Also, CME rules restrict me from listing specific product names (working on getting CEU/CMEs for the Review).
- Follow up: 6 -8 weeks
Visit 8
Subjective Assessment:
- GI soothing compound and acid reducing compounds – did not try
- Nexium (2 weeks trial) – helped upper GI (reflux, chills/goosebumps)
- Nexium symptoms came back after stopping – now back on Nexium
- Diet is now broadened – helped fatigue
- Improved:
- Fatigue
- Reflux
- Chills/goosebumps
- Brain fog & headaches
- Hot at night
- Same:
- Gas/bloating
- Worse:
- N/A
Impression:
- 9/1/17 – Today Nishant has responded very well to Nexium and broader diet. It appears this was the missing piece, and eating an overly restrictive diet was impairing energy. Also, it appears HAbx were likely flaring gastritis. Will maintain current plan and have him finish course of Nexium with GI. Then follow up and work to minimize program and address any lingering symptoms.
Recommendations:
- Continue previous plan
- Continue to try and go to bed before 12 for 1 week.
- Continue to avoid coffee.
-
- NRT: Vitamin D/K, Magnesium, Omega 3-6-9 blend
- GI: Lacto/Bifido blend, S. boulardii
- GI: Continue with VSL#3 and Citrucel
-
- Lifestyle: regular exercise (weight lifting), walking in nature
- Use the lowest end of the probiotics dose range
- GI: GI soothing compound, 2 natural acid lowering compounds
- — I know you’re dying to know what the exact compounds are here, however it is irrelevant once you read the next visit. Also, CME rules restrict me from listing specific product names (working on getting CEU/CMEs for the Review).
- GI: GI soothing compound, 2 natural acid lowering compounds
- Starting
- Continue to broaden your diet
- GI: GI soothing compound, 2 natural acid lowering compounds
- Follow up: 2-3 months
Dr. Ruscio’s Comments
Treating SIBO here resulted in partial improvement that one would expect to see. Outside of the SIBO treatment, there are three key takeaways here:
- Some patients require a short term of acid lowering and may benefit from acid lowering Rx (I know, blasphemy).
- Herbal antimicrobials can irritate the lining of the stomach and therefore flare gastritis or ulcers.
- An overly restrictive diet can be a serious problem.
It’s important to be on the lookout for gastritis/ulcers, because spotting this prevented us from doing more SIBO or dysbiosis testing/treatment. How do we know Nishant had gastritis? Technically we don’t. However, a reasonable perspective with gastritis is ‘the treatment is the test.’
Nishant was also borderline orthorexic because of all the reading he had been doing. I had always encouraged him to not be 100% with the diet and to test the boundaries, but he never fully did this until late in our work together. When he finally did expand his diet, this had a marked effect on his fatigue and brain fog. So don’t forget that an overly restrictive diet can be problematic also.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!