Practitioner Case Study – December 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- The risks and benefits of sun exposure 2016, review.
- What is the clinical role of oral liquid preparations in the treatment of patients with hypothyroidism?
- The effect of the apolipoprotein E genotype on response to personalized dietary advice intervention: findings from the Food4Me randomized controlled trial.
- The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS.
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Kim, 36yo female
- Previous Dx
- “Pancreatic insufficiency” by her naturopath
- Rx
- N/A
- Chief complaints
- Pain (lower abd.)
- Bloating
- Irregular bowels; constipation/diarrhea
- Food allergies
- Symptoms expressed in paperwork but not listed as CCs
- Fatigue, insomnia, anxiety/depression
- Female: irregular cycles, pain/cramping, PMS
Visit 1 (4/28/17) – History and Exam:
Initial Impression
Kim presents as a pleasant 36yo female with a good diet, lifestyle, and outlook on her health. Since age 19 she has been suffering from her CCs, which are mainly GI in nature. They started with no known cause.
GI MD workup was all normal but was dx with SIBO. SIBO diet was helpful, Rifax was slightly helpful. HAbx did not help. Fasting is also helpful. Kim is extremely gluten sensitive. She has seen some response to diet and Abx but has slowly regressed. I anticipate Kim will respond well once we establish a more comprehensive care plan for her. She may do better with Abx.
No unusual ddx, but consider SIFO and/or H2S SIBO if non-responsive. Also, adhesions due to an appendectomy, miscarriage, and inflammation. Also, pancreatic insufficiency, sleep disorder breathing… see list.
She has a good attitude and support structure, but issues have been long-standing. Prognosis fair to good.
Previous Diets
- GF/DF/low CHO/egg free – helps
- Fasting – v. helpful
- Low FODMAP w/ SCD – v. helpful
Previous Treatments
- Rifax (2x) – helped slightly, but then SS returned
- HAbx – non-responsive
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Optional: Doctors Data Comp. Stool w/ Para 3x stool test
- LabCorp full GI panel
- LabCorp general health panel
- Rationale
- We, of course, want to quantify if she still has SIBO
- A stool panel can be helpful to rule out concomitant dysbiosis or infection like fungus or H. pylori. I often order a second stool/GI workup but list it as optional for the patient. They then decide based on cost and their motivation level. For me, it’s helpful, but not fully needed so I leave it as optional.
- We also want to check for things like anemia, vitamin D, hypothyroid, etc. with the general health/wellness panel.
Recommendations
- Please perform the Modified Fast for 2-4 days (see website for PDF), then
- Start on the Low FODMAP plus SCD diet, see website for PDF. You can continue to fast during the day and consolidate your meals for lunch/dinner.
- Be on this diet for 2 weeks before starting on your supplement plan.
- Discontinue coffee.
- Be on the below supplement plan for 3 weeks before following up.
- Nutritional support: vitamin D/K
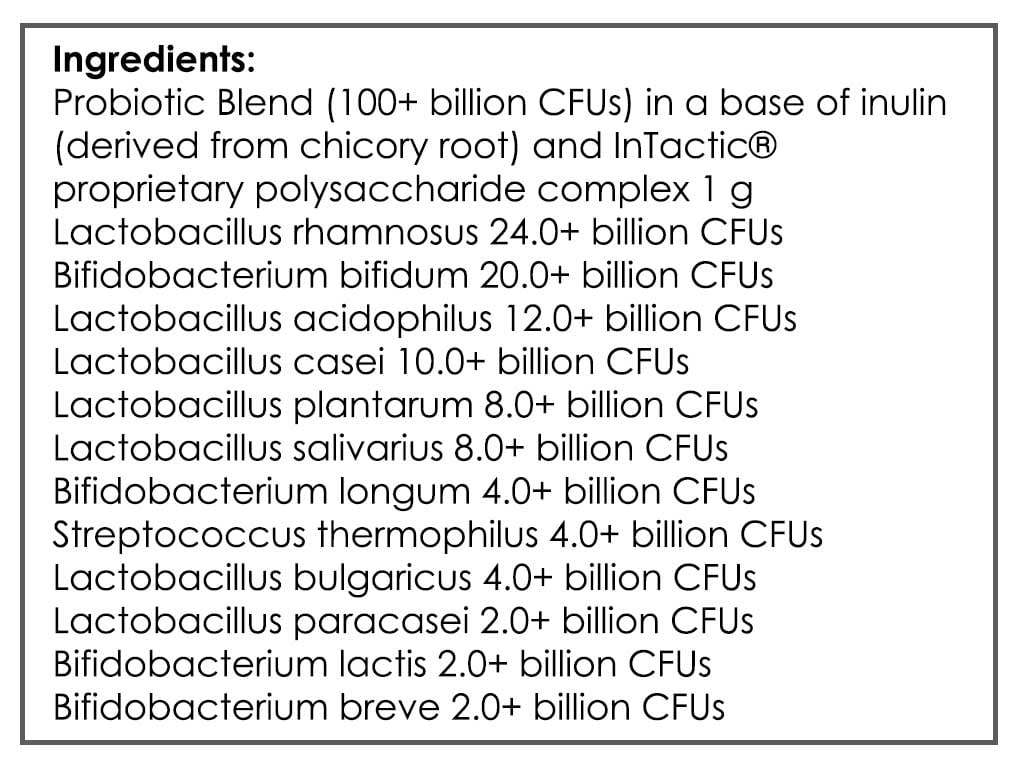
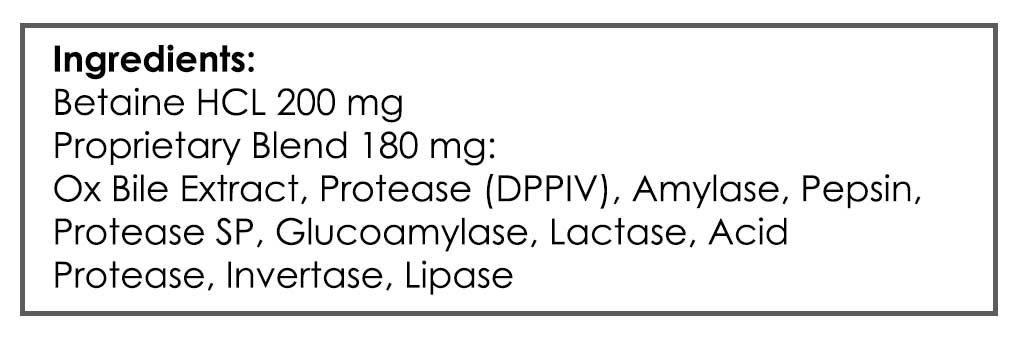
- GI: Lacto-bifido blend probiotic, S. boulardii, digestive enzyme & acid
- Rationale
- Fasting has helped previously, as has the low FODMAP w/ SCD diet (sometimes called the SIBO diet).
- Vitamin D and probiotics can improve IBS and/or SIBO.
- She may need enzymes per her Dx, but I question if she has true pancreatic insufficiency as her naturopath diagnosed. More to follow on this in my comments at the end.
Visit 3 (6/16/17) – Lab Interpretation and Treatment Evaluation
Lab Interpretation:
- Aerodiagnostics Lactulose SIBO breath test
- H2 179*, CH4 4
- LabCorp #1 blood, urine, stool & breath
- Benzoate
- Positive Stim Ctyl 1.7-L
- Parietal cell ABs (APCA)
- 28.4-H
- Benzoate
- LabCorp #2 blood & urine
- Basics, additions
- Alkaline Phos 36-L, cholesterol 207-H, LDL 136-H, UA Abnormal- Ketones 1+ abnormal
- Basics, additions
- Optional: Doctors Data Comp. Stool w/ Para 3x stool test
- N/A not performed
- Dx
- Severe H2 SIBO. LC: APCA.
- Summary
- SIBO and stomach autoimmunity
Subjective Assessment:
- MF (could not tolerate either version so did water) – digestion was a lot better, but was tired and hungry
- Low FODMAP w/ SCD – v. helpful but hard to follow; GI was great but was tired
- No caffeine – withdrawal was hard, very fatigued; now is OK; GI feels better off coffee
- Initial supplement program – no change
- Improved:
- Abd pain and bloating (way better), irregular bowels (gone)
- Same:
- Food allergies/reactivity
- Fatigue, insomnia
- Anxiety
- Female symptoms
- Worse:
- Depression
Impression:
- Today’s severe H2 SIBO perfectly fits her presentation. She has been dx and treated for SIBO in past; she had responded but then relapsed historically, so will likely need a more comprehensive plan; has responded better to Abx. Based on this, will request IBSDetex today to predict the need for Rx prokinetic. Other ddx are viable (see list), consider soon if MR, fast relapsing. Today, has responded very well to low FODMAP/SCD and coffee removal. Initial supplement program non-responsive. Will start today on 4-6 weeks Rifaximin, B12 injections, Preg/DHEA, a limited CHO reintro, and limited caffeine reintro. At follow up, determine if it’s time to transition off Abx and onto prokinetics. Also, consider retesting at that time to justify the use of tail HAbx or ED while on prokinetics.
Recommendations:
- Continue on the Low FODMAP plus SCD diet, see website for PDF. You can continue to fast during the day and consolidate your meals for lunch/dinner.
- Continue previous
- Nutritional support: vitamin D/K
- GI: Lacto-bifido blend probiotic, S. boulardii, digestive enzyme & acid
- Starting
- Please perform Quest blood test before starting treatment today.
- Add some GF bread, yogurt, other dense carbs, and potatoes to your diet and see if this helps energy. Keep this minimal for now.
- You can also use more caffeine, but be minimal.
- Adrenal: Preg, DHEA
- GI: Rifaximin 4 weeks. B12 injections (weekly)
- FU: 3 weeks
Visit 4 (7/12/17)
Lab Results:
- IBS Detex- Quest
- Negative
- Dx:
- N/A
- Summary
- Does not have autoimmunity against motility cells in gut
Subjective Assessment:
- Recently had setbacks from drinking/weddings – almost back to baseline
- Rifaximin – about the same
- Addition of GF bread, pasta, carb – very helpful
- Preg, DHEA – might help
- Improved:
- Fatigue
- Same:
- Regressed – GI, anxiety/depression, sleep
- Worse:
- N/A
Impression:
- 7/12/17 – IBSDetex negative, therefore post-antimicrobial prokinetic less important. Since motility AI was negative, will consider following Abx with HAbx or ED today. Today is about the same from Rifaximin; this is confounded by recent drinking while on vacation, which caused a flare. Adding some CHO back into diet clearly helped. Preg/DHEA – minimally responsive. Today starting elemental/semi-elemental as Rifaximin ends. Will follow up at end of 2nd week and decide on 3rd week and/or HAbx.
Recommendations:
- Continue previous
- Nutritional support: vitamin D/K
- GI: Lacto-bifido blend probiotic, S. boulardii, digestive enzyme & acid
- Adding some GF bread, yogurt, other dense carbs, and potatoes to your diet and see if this helps energy. Keep this minimal for now.
- You can also use more caffeine, but be minimal.
- Adrenal: Preg, DHEA
- B12 injections (weekly)
- Ending
- GI: Rifaximin 4 weeks
- Starting
- Perform the semi-elemental diet or elemental exclusively for 2 weeks (see website PDF for more).
- FU: at end of elemental diet
Visit 5 (8/30/17)
Subjective Assessment:
- Elemental diet (14 days) – feeling great
- Then when returning to normal diet – felt great
- Improved:
- All CCs
- Same or Worse:
- N/A
Impression:
- 8/30/17 – Kim has responded very well to 2 weeks of the exclusive elemental. Then, when returning to normal foods, she continued to feel great and this has persisted for over 2 weeks at the point of our follow up (Kim was not able to get an appointment to check in at the exact end of her elemental diet). Today we will have Kim first maintain the current plan of just diet, but will also add vitamin D back in. Then after one month, will have her experiment to see if any of the items from her previous program were helpful. And then finally, in 2 months, will have her perform a dietary reintroduction.
Recommendations:
- Starting
- Stay on diet and no supplements other than Vitamin D for 1 month.
- Then, for one month gradually introduce the other supplements; continue on anything that helps, discontinue anything that does not.
- Then, roughly 2 months from now, start into the dietary reintroduction.
- FU: 1-3 months
Dr. Ruscio’s Comments
Kim’s case was a good example of why it’s important to start with the fundamentals. A patient like Kim who did not respond to Rifaximin the second time (even though she did the first time) and who was previously non-responsive to herbal antimicrobials might make a practitioner go to extremes. “This must be biofilm, SIFO, H2S SIBO… we need to test more, let’s order and OAT test…” However, any of this would be putting the cart before the horse if you had not yet tried another fundamental treatment for SIBO, an elemental or semi-elemental diet. So, don’t make this harder or more elaborate then it needs to be. Cover your fundamentals first.
Also, and to be fully candid, I was suspicious that the ‘pancreatic insufficiency’ was a BS label from her naturopath. Likely based upon some tests that are theorized to indicate pancreatic insufficiency, but have actually not been validated. I’m still open to this actually being true, but it’s highly unlikely. Especially when considering that response to treatment is considered the most relevant test in most of the literature for PI. Since she was in my office, I am assuming she did not respond to the enzymes given to her by her other doctor. Nor did she appear to need the ones I gave her as she was feeling great after being off of them for a few weeks. Additionally, remember every diagnosis you assign to someone will carry a heavy weight. They will read up on it on the internet and internalize what they read. If someone does not have a disease, it’s best not to label them with one. A better way to phrase this would have been “your lab work shows you may benefit from supplementing with enzymes.”
Symptoms not listed as chief complaints can also be telling. Most of us are likely already making note of these, but I felt this worth mentioning just in case. Two areas I strongly look to are signs of burnout and signs of female hormone imbalance, in both symptom sections of my paperwork. This did not make a difference in Kim’s case, but I just wanted to point this out.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!