Practitioner Research Review – December 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- The risks and benefits of sun exposure 2016, review.
- What is the clinical role of oral liquid preparations in the treatment of patients with hypothyroidism?
- The effect of the apolipoprotein E genotype on response to personalized dietary advice intervention: findings from the Food4Me randomized controlled trial.
- The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS.
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
The risks and benefits of sun exposure 2016.
https://www.ncbi.nlm.nih.gov/pubmed/27942349
Study Purpose
- “review of recent studies and their analyses consider the risks and benefits of sun exposure.”
Intervention:
- Review, non-systematic
Main Results:
- “…studies that have shown a wide range health benefits from sun/UV exposure. These benefits include among others various types of cancer, cardiovascular disease, Alzheimer disease/dementia, myopia and macular degeneration, diabetes, and multiple sclerosis.”
- Ideal levels: 40–60 ng/mL
- “…it is apparent that vitamin D supplements are not an effective substitute for adequate sun exposure.”
- White people with Type II skins at 40 degrees latitude can obtain their annual requirements of vitamin D by spending about 15 minutes in the sun with face, arms and legs exposed (half that time if in a bathing suit) 2 to 3 times a week between 11 a.m. and 3 p.m. during the months of May through October.
- Type II skin: You almost always burn and rarely tan in the sun.
- “People with darker skins require more time in the sun.”
- The authors note this is likely far less than what might increase the risk of non-melanoma skin cancers (discussed below).
Additional Results:
Melanoma (the most dangerous form of skin cancer)
- Non-burning sun exposure reduces risk while burning increases risk.
- “non-burning sun exposure is associated with a reduced risk of melanoma, while sunburns are associated with a doubling of the risk of melanoma.”
- “It has long been observed that outdoor workers have a lower incidence of melanoma than indoor workers (13-19). A 1997 meta-analysis found an OR of 0.86”
- Sun exposure may protect the skin from cancer because sun exposure leads to the formation of the active form of vitamin D (1, 25-OH), which also improves DNA repair.
- The rise in melanoma incidence is likely due to a combination of 2 factors. 1) Less chronic, non-burning exposure to the sun (less time outside) -PLUS- 2) increased bouts of high exposure and burning (as occurs on vacations). So, we no longer condition our skin with chronic, non-burning exposure, but rather overexpose non-conditioned skin episodically.
- “We can find no consistent evidence that use of chemical sunscreens reduces the risk of melanoma.” Note: there is some evidence showing sunscreen reduces risk, but it is not high-quality data.
Non-Melanoma Skin Cancer
- While non-burning sun exposure is associated with decreased melanoma risk, it appears that it does increase the risk of SCC and BCC (squamous and basal cell carcinomas). However, not all the data here agree (some studies show no association) and the relationship between chronic sun exposure and non-melanoma cancer is not entirely clear.
- This was the only factor studied that showed increased risk of sun exposure:
- “The only identified risk associated with the amount of non-burning sun exposure needed to achieve serum 25(OH)D levels of 30 ng/mL is some possible increased risk of nonmelanoma skin cancer.”
All-Cause Mortality (death from any cause)
- Much association data show higher vitamin D levels equate to better health. But, the association does not mean cause.
- A 20-year follow-up study found avoiding the sun increases all-cause mortality.
- “The mortality rate amongst avoiders of sun exposure was approximately twofold higher compared with the highest sun exposure group.”
- Another study found that sun avoidance also increases all-cause mortality to a degree similar to smoking.
- “Our finding that avoidance of sun exposure was a risk factor for all-cause death of the same magnitude as smoking is novel.”
Colorectal Cancer
- No consistent effect between sun exposure nor vitamin supplementation reported.
Breast Cancer Incidence and Mortality
- One meta-analysis showed that higher blood levels of vitamin D were associated with decreased mortality.
- “Mohr et al. 2014 conducted a meta-analysis of data from 5 studies on the relationship between serum 25 (OH)D levels at time of breast cancer diagnosis and breast cancer mortality which found that patients in the highest quintile of 25(OH)D (more than 32 ng/mL) had approximately half the death rate from breast cancer as those in the lowest quintile (less than 14 ng/mL)”.
- Two studies have shown that increased sun exposure reduces breast cancer risk.
- “John et al. 1999 found that women with higher solar UVB exposure in NHANES III had only about half the incidence of breast cancer as those with lower solar exposure.
- Knight et al. 2007 found that increasing sun exposure from ages 10 to 19 reduced breast cancer risk by 35%, for the highest quartile of out-door activities vs. the lowest.”
Non-Hodgkin’s Lymphoma, Colorectal, Prostate and Breast Cancer, and Multiple Sclerosis
- A systematic review concluded the following (in short, sun exposure seems generally protective and the protective effects are sometimes independent of vitamin D levels or intake, meaning sun exposure exclusively appears to be responsible for the effect):
- “there is an inverse association between sun exposure and both colorectal cancer risk and colorectal cancer mortality;
- there is an inverse association between vitamin D status and both colorectal cancer risk and colorectal cancer mortality;
- there is a negative association between sun exposure and prostate cancer risk and prostate cancer mortality but not between vitamin D status and prostate cancer risk or mortality;
- there is an inverse correlation between sun exposure and breast cancer risk and breast cancer mortality, and possibly between 25(OH)D and breast cancer mortality, but studies on the association between 25(OH)D and breast cancer risk are inconclusive;
- there is a negative association between sun exposure and NHL risk and NHL mortality but not between vitamin D status and NHL risk or mortality;
- there is a negative association between sun exposure and lymphoma risk, but no association between lymphoma risk and vitamin D intake or 25(OH)D levels; and
- for multiple sclerosis, both experimental and epidemiological studies show that the preventative role of sun exposure is independent of vitamin D production”
Cardiovascular Disease (CVD)
- Two studies have shown sun exposure helps to lower blood pressure, independent of vitamin D.
- “Liu et al. 2014 found that hypertension is reduced by UVR-induced nitric oxide independent of vitamin D. They showed that stores of nitrogen oxides in the human skin are mobilized to the systemic circulation by exposure of the body to UVA radiation, causing arterial vasodilation and a resultant decrease in blood pressure independent of vitamin D, confirming the hypothesis of Feelisch et al. 2010”
Obesity & Type II Diabetes
- Sun exposure, not vitamin D levels or supplementation, reduced risk.
- “Geldenhuys et al. 2014, found that UVR exposure levels, not vitamin D supplements or 25(OH)D levels, reduced the risk of obesity and type 2 diabetes…”
Multiple Sclerosis
- Again, sun exposure, but not vitamin D levels or supplementation, reduced risk.
- “Baarnhielm et al. 2012 was an association study finding that persons with low UVR exposure had a significantly increased risk of MS compared with those who reported the highest exposure (OR 2.2, 95% CI 1.5–3.3), and that this association persisted after adjustment for vitamin D status.
- Wang et al. 2014 and Baarnhielm et al. 2012 confirmed the conclusions of van der Rhee et al. 2013 that sun exposure reduces the risk of MS through pathways independent of vitamin D.”
Type I Diabetes
- Sun exposure reduces risk.
- “Jacobsen et al. 2015 found that more sun exposure in the third gestational trimester was associated with lower risk of type 1 diabetes in male children.”
Liver Disease
- Again, sun exposure, but not vitamin D levels or supplementation, reduced risk.
Authors’ Conclusion:
- “Insufficient sun exposure has become a major public health problem, demanding an immediate change in the current sun-avoidance public health advice. The degree of change needed is small but critically important. The public must be advised to obtain enough sun exposure and vitamin D supplementation to maintain a serum 25(OH)D level of at least 30 ng/mL.” Note: they are not recommending supplementation here**
Interesting Notes:
- Vitamin D deficiency is rapidly increasing, with recent estimates that over 75% of the population is deficient (below 30 ng/mL).
- “Using the Endocrine Society’s definition of vitamin D sufficiency of 30 ng/mL, the level of vitamin D insufficiency increased from 55% of the US population in NHANES III to 77% in NHANES 2001–2004, which indicates that the vast majority of Americans have an insufficient vitamin D status.”
- “Public health authorities in the United States are currently advising that human sun exposure be reduced. At the same time, NHANES data show that 32% of Americans suffer from vitamin D insufficiency.”
Clinical Takeaways:
- Obtaining chronic, non-burning sun exposure is a key practice for optimum health.
- Vitamin D supplementation may not be an acceptable substitute.
- Obtain at least 15 minutes (or more for darker skin types) of direct, unprotected sun exposure 2-3 days a week, midday, during the sunny months.
Dr. Ruscio’s Comments
Not much to add here, this study pretty much speaks for itself. Obtain chronic, non-burning sun exposure and don’t rely on supplementation to increase your levels.
What Is The Clinical Role Of Oral Liquid Preparations In The Treatment Of Patients With Hypothyroidism?
https://www.ncbi.nlm.nih.gov/pubmed/28095045
Study Purpose
- To review the potential advantages of oral liquid preparations in the treatment of patients with hypothyroidism.
Intervention:
- Commentary on a recent trial by Fallah, et al., https://www.ncbi.nlm.nih.gov/pubmed/27849377
Main Results:
- Fallah’s study found improved TSH when using liquid T4 as compared to levothyroxine tablets.
- “They noted that the 21 patients with elevated serum TSH values on tablet levothyroxine had a statistically significant decrease in serum TSH values into the normal range, but no change in FT4 and FT3, when switched from oral tablet levothyroxine preparations to the liquid levothyroxine preparation.”
- This result was no coincidence, as it occurred again after subjects went back on tablet levothyroxine and then again switched to liquid form.
- “Further, 15 of the 21 patients were then switched back to their tablet levothyroxine preparation and TSH significantly rose. Patients were then given the oral liquid levothyroxine preparation and followed long term; as expected, the serum TSH values decreased again and remained constant.”
- Liquid T4 does not contain the excipients (fillers) that are contained in tablet form.
- “the liquid preparation contains alcohol, apparently without additional excipients.”
- In adults with hypothyroidism, switching from levothyroxine to liquid T4 caused a significant median decrease of TSH from 3 to 2.30.
- Those with atrophic gastritis (severely impaired stomach acid secretion) appear to see better responses in TSH with liquid form T4.
Additional Results:
- The majority (68%) of thyroid hormone Rx absorption occurs in the small intestine.
- “… approximately 15% of oral T4 was absorbed in the duodenum, 29% in the upper jejunoileum, and 24% in the lower jejunoileum.”
- Coffee can interfere with levothyroxine absorption.
- Soft gels may be preferred to true liquid forms of T4.
- Documented conditions that interfere with thyroid hormone absorption:
- “Coeliac disease, inflammatory bowel disease, lactose intolerance as well as Helicobacter pylori (H. pylori) infection and atrophic gastritis.”
- “Drugs, such as bile acid sequestrants, ferrous sulphate, sucralfate, calcium carbonate, aluminium-containing antacids, phosphate binders, raloxifene and proton-pump inhibitors.”
- Cost may be factor limiting use of liquid T4.
- “For example, the cost of a liquid levothyroxine capsule in two major pharmacy chains in the United States is approximately $150 for 100 microgram tablets for 30 days or $1800 per year, values higher than brand levothyroxine tablets without insurance.”
Authors’ Conclusion:
- N/A
Interesting Notes:
- N/A
Clinical Takeaways:
- Liquid or soft gel forms of thyroid hormone may be preferential to tablet form in those with impaired GI health.
Dr. Ruscio’s Comments
In my opinion, there is much hyperbole regarding thyroid treatment in FM. This is one area that clearly deserves some attention, however. We know that many people with impaired GI health will exhibit hypothyroid-like symptoms even when on thyroid Rx. A missing component for some of these cases may be a simple switch to a more absorbable form, thus allowing more consistent thyroid hormone levels. If you do a good job improving your patient’s GI health, the need for liquid thyroid Rx shouldn’t be common. But, for those with more severe GI involvement, this may be required.
The effect of the apolipoprotein E genotype on response to personalized dietary advice intervention: findings from the Food4Me randomized controlled trial.
https://www.ncbi.nlm.nih.gov/pubmed/27510539
Study Purpose
- To assess if gene-based dietary (personalized nutrition = PN) recommendations would be helpful for those with the APOE4 genotype.
- “The apolipoprotein E (APOE) risk allele (e4) is associated with higher total cholesterol (TC), amplified response to saturated fatty acid (SFA) reduction, and increased cardiovascular disease…it is unclear whether e4 carriers would benefit from gene-based personalized nutrition (PN).”
Intervention:
- Randomized controlled trial.
- 1,466 subjects were randomly assigned into one of four groups:
- Level 0: standard non-personalized dietary and physical activity (PA) advice
- Level 1: advice based on dietary intake and PA
- Level 2: advice based on dietary intake, PA, and phenotype (blood biomarkers)
- Level 3: advice based on dietary intake, PA, phenotype, and genotype
- Diet and total cholesterol (TC) were evaluated at baseline and at 6 months.
Main Results:
- Significantly higher TC concentrations were observed in E4+ participants than in E4-, at baseline.
- There were no significant differences in response to gene-based diet when comparing those with the APOE4 gene and those without it.
- “However, there were no significant differences in change of diet, TC, or omega-3 index between APOE risk groups (E4+ and E4-) receiving gene-based PN.”
- “there was no additional benefit of gene-based PN for E4+ participants.”
- Note: the number of subjects in this study was small and might have led to the non-significant change from gene-based dietary advice. A larger study might show otherwise.
- Being told the diet recommendation was based upon one’s genes improved compliance, even if one did not have the genes which increased risk.
Additional Results:
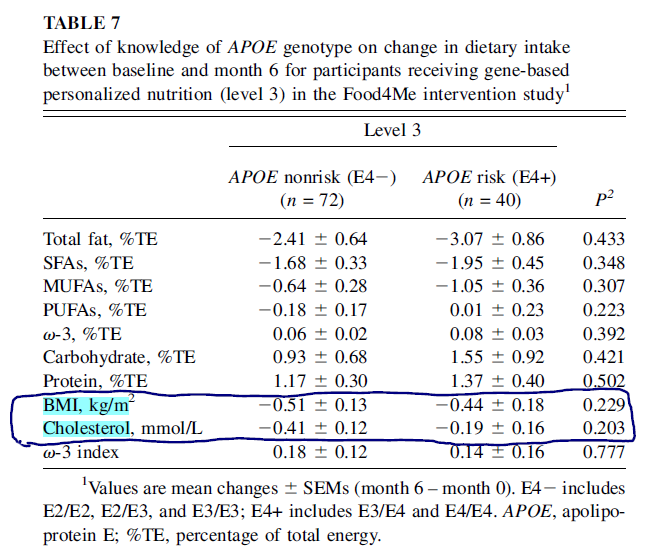
- When comparing two groups put on the same ‘gene-diet,’ one group with no gene risk (E4-) and one group with gene risk (E4+), there was no difference in changes in BMI or total cholesterol between the two groups after 6 months.
Authors’ Conclusion:
- “Although gene-based PN targeted to APOE was more effective in reducing SFA intake than standard dietary advice, there was no difference between APOE ‘risk’ and ‘nonrisk’ groups.”
Interesting Notes:
- “The APOE gene is a key regulator of cholesterol and lipid metabolism.”
- “The e4 allele is associated with increased serum total cholesterol (TC) and LDL cholesterol, as well as coronary artery disease and mortality.”
- “data from intervention studies suggest that E4+ participants may be more sensitive to dietary cholesterol, total fat, and, in particular, SFA modulation.”
- “There is a dose-dependent inverse association between omega-3 index and CHD mortality (33), with an index >8% offering the most cardioprotective effects and an index <4% being associated with the greatest risk of CHD mortality. Thus, the omega-3 index may be a risk factor for CHD.”
- As much as I dislike fear as a motivator, the authors cite a meta-analysis that shows fear is an effective motivator.
- “In a meta-analysis of fear arousal techniques, stronger fear messages promoted greater intention and behavior change in public health campaigns, provided that the threat was perceived to be severe and personally relevant, and that individuals could take specific action to mitigate their risks.”
- https://www.ncbi.nlm.nih.gov/pubmed/11009129
Clinical Takeaways:
- Gene testing to personalize dietary recommendations did not improve results.
- However, gene testing and associated fear of increased risk appear effective at improving compliance.
Dr. Ruscio’s Comments
I remain fully open to gene testing in clinical practice, should evidence be provided showing it to be helpful. However, as I have repeatedly stated, it appears gene testing promises much but delivers little. There are a few exceptions to this rule for genes that are associated with a disease state and for which a corresponding treatment has been studied and established to be effective. However, this is reserved for a handful of rare medical conditions and does not apply for most of what is being assessed in functional medicine, including APOE and the MTHFR group of markers. Understanding this can prevent clinicians and their patients from wasting much time and money in pursuit of meaningless markers. I will be more than happy to update my opinion here once we have supporting evidence.
The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS.
https://www.ncbi.nlm.nih.gov/pubmed/28592442
Study Purpose
- To review the available data on the low FODMAP diet and its mechanisms.
Intervention:
- Review, non-systematic.
Main Results:
- “There are currently at least 10 randomised controlled trials or randomised comparative trials showing the low FODMAP diet leads to a clinical response in 50%–80% of patients with IBS, in particular with improvements in bloating, flatulence, diarrhea and global symptoms.”
- Note: so it’s not surprising to see a meta-analysis finding the low FODMAP diet effective.
- The low FODMAP diet may also be effective in the long term.
- “Follow-up of patients consuming a FODMAP-modified diet suggests clinical benefit in 57%–74% of patients at 14–16 months (62), although the results are likely subject to significant recall bias.”
- https://www.ncbi.nlm.nih.gov/pubmed/17000196
- Supplementing with soluble fiber is a viable therapy for IBS according to two meta-analyses.
- “Two recent meta-analyses identified between 14 and 22 randomised controlled trials (RCTs) of dietary fibre, and reported moderate quality evidence for fibre supplementation in IBS, with greater global symptom improvement compared with placebo, in particular for soluble fibre.”
- There is weak evidence for removal of caffeine, fat, and alcohol.
- Some evidence shows soy, milk, wheat, and yeast to be problematic, but verification of randomized control studies are required.
Mechanisms of the Low FODMAP Diet
- Small intestinal water
- Studies have clearly documented that increased FODMAP intake will increase water in the small intestine. However, this increased water has not been shown to influence symptoms. So, the impact of SI water is unclear.
- Inulin does not appear to affect SI water.
- Glucose can help with fructose absorption and therefore decrease fructose’s impact on SI water.
- Colonic gas production
- A high FODMAP diet can increase breath hydrogen levels, which correlate with the exacerbation of IBS.
- “A controlled, crossover feeding study demonstrated that a high FODMAP diet (50 g/day) led to a marked increase in 14-hours breath hydrogen production after two days compared with a low FODMAP diet (<10 g/day) in 15 patients with IBS and 15 healthy individuals, which was paralleled by higher symptoms scores in those with IBS.”
- A low FODMAP diet has been shown to decrease hydrogen gas levels.
- “Furthermore, a recent crossover study in IBS showed that a 3-week low FODMAP diet (unknown total FODMAP dose) reduced 5-hour breath hydrogen following a lactulose challenge compared with a high FODMAP diet (unknown total FODMAP dose), suggesting the low FODMAP diet leads to a shift in colonic fermentation pattern independent of acute fermentable carbohydrate intake (i.e. lactulose challenge), which is likely mediated by an alteration in microbiota composition.”
- Inulin has been shown to increase intestinal gas levels.
- Those with IBS may not produce any more colonic gas than healthy controls, but rather may be hypersensitive to the gas that is produced in response to FODMAPs. Note: this was only according to one small study, however.
- “Patients with IBS who developed symptoms on FODMAP challenge did not, in fact, have greater colonic volume than those who do not report symptoms, suggesting that visceral hypersensitivity to luminal distension, rather than increased luminal distension per se, is key to symptom provocation during colonic fermentation”
- A high FODMAP diet can increase breath hydrogen levels, which correlate with the exacerbation of IBS.
- Motility
- Not enough research has been performed to form a conclusion.
- Microbiota
- Histamine has been shown to decrease from a low FODMAP diet.
- Changes in the microbiota and immune system from a low FODMAP diet might be responsible for improved clinical outcomes.
- “Several associations were also found between abundance of various taxa, the metabolome and clinical symptoms, suggesting that the observed diet-induced changes in the microbiota and metabolome may be in part responsible for clinical outcomes.”
- Short Chain Fatty Acids (SCFAs)
- A low FODMAP diet may decrease SCFAs, which are often elevated in IBS.
- “Several associations were also found between abundance of various taxa, the metabolome and clinical symptoms, suggesting that the observed diet-induced changes in the microbiota and metabolome may be in part responsible for clinical outcomes.”
- However, some low FODMAP studies show no change in SCFAs.
- “However, current evidence regarding the effect of the low FODMAP diet on SCFA is limited by conflicting findings between studies.”
- Stool may not be a good measure for SCFAs. Note: a marker I do not use.
- “Furthermore, stool SCFA concentration is not an accurate measure of in vivo SCFA production due to the effect of colonic transit time on SCFA absorption and stool volume on SCFA dilution.”
- “without assessment of SCFA concentration at the major site of production in the ascending colon, which requires technically demanding and invasive techniques (54), it will be difficult to confirm the interaction between the low FODMAP diet, SCFA production and symptom provocation in IBS.”
- A low FODMAP diet may decrease SCFAs, which are often elevated in IBS.
- Serotonin cells
- A low FODMAP diet may normalize serotonin cells.
- “One RCT of patients provided low FODMAP advice in combination with other dietary advice (n=13) reported normalization of colonic serotonin cell density after 3–9 months.”
- A low FODMAP diet may normalize serotonin cells.
- Leaky gut
- A low FODMAP diet may improve leaky gut.
- “normalization of stool lipopolysaccharide to levels comparable with healthy controls has been demonstrated in patients reporting a symptomatic response to a low FODMAP diet.”
- A low FODMAP diet may improve leaky gut.
Does a low FODMAP diet damage the microbiota?
- Summary: the thinking that the low FODMAP diet damages the microbiota is not supported.
- Two studies have shown a decrease in Bifidobacterium, but with no changes to other bacteria or total bacteria.
- “a 50% reduction in FODMAP intake led to a marked six fold reduction in relative abundance of Bifido-bacteria compared with controls who maintained their habitual diet. There were no differences in total bacteria or other bacterial groups such as Lactobacillus or Faecalibacterium prausnitzii.”
- Another study showed a decrease in absolute bacteria numbers, but at the same time displayed an increased diversity in healthy bacterial populations like Clostridium cluster XIV.
- Another study showed no change in alpha or beta diversity from the low FODMAP diet.
Does a low FODMAP diet cause nutrient deficiencies?
- There does not appear to be a significant impact on carbs or calories when compared to standard IBS dietary advice.
- Lower calcium intake has been reported, likely due to decreased dairy consumption.
Additional Results:
- Only one medical treatment for IBS is supported by high-quality evidence: linaclotide (Linzess). Note: this review scored Rifaximin as having moderate level evidence.
- “there is a lack of effective pharmacological treatments available, with a technical review reporting high quality of evidence for only one of nine pharmacological treatments.”
- https://www.ncbi.nlm.nih.gov/pubmed/25224525
Authors’ Conclusion:
- “Convincing evidence exists for the clinical efficacy of the low FODMAP diet in IBS, which represents a therapeutic milestone for a condition that has historically been difficult to treat by either medical or dietary means.”
Interesting Notes:
- The majority of IBS patients, 70-80%, report food reactivity.
- “Numerous studies show that the majority of patients with IBS (70%–89%) report that specific foods exacerbate symptoms and consequently many patients limit or exclude some food items.”
- “Recent studies have used MRI to demonstrate that short-chain fermentable carbohydrates increase small intestinal water volume and colonic gas production that, in those with visceral hypersensitivity, induces functional GI symptoms.”
- IBS does not contribute to mortality, but significantly affects quality of life.
- “Although there is no impact of IBS on mortality, it is likely that the morbidity associated with its chronic nature and the high incidence of GI and extra-intestinal comorbidities, such as anxiety and depression (5), contribute to its negative impact on health-related quality of life.”
Clinical Takeaways:
- The low FODMAP diet is an effective therapy for IBS.
- Current evidence suggests it does not appear to damage the microbiota and might even help repair the gut and dampen immune activation.
Dr. Ruscio’s Comments
In short:
- The low FODMAP diet is an effective therapy for IBS.
- It does not damage the microbiota and might even help repair the gut and immune system.
- Changes in SCFAs are likely irrelevant.
But also remember to encourage your patients to later reintroduce and work to the broadest diet possible in the long term.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!