The balance of bacteria in your gut (aka microbiota) can impact not only digestive symptoms, but a wide array of seemingly unrelated symptoms and conditions including mood, energy, skin, your joints, metabolism, sleep, immune function, hormone balance and thyroid health. Probiotics can help balance your microbiota, the world of bacteria in your gut, and thus these symptoms and conditions.[1, 2, 3, 4, 5, 6, 7, 8, 9, 10]
This is not speculation nor is this wishful thinking. Clinical trials have shown that people who are not feeling well can improve their health by modulating the microbiomes with probiotic bacteria. This is good news. However, marketers are also quick to make hyperbolic health claims that will lead you to waste your money. Fortunately, when we take a principled and science-based approach, we can simplify the probiotic landscape down to three key formulas and an easy to follow protocol. Let’s cover what probiotics can do, what they can’t do, what the best probiotics are and how to use them effectively.
Fast Facts Summary |
|
Probiotics are live microorganisms that confer health benefits when consumed. They can be obtained through foods (sauerkraut, kombucha, kimchi, etc..) or via probiotic supplements.

In an ideal world, probiotics wouldn’t be needed. Unfortunately, in today’s world imbalances in intestinal microbiota are the norm. Why?
- Overuse of antibiotics
- Lack of, or short-term duration, of breastfeeding
- Cesarean (C-section) birth
- Reduced contact with animals, dirt and environmental bacteria
- Overuse of antibacterial soaps
- Unhealthy diets low in fiber and high in processed foods and added sugar
- Sedentary lifestyle and poor sleep habits (yes, these affect your intestinal bacteria)
The above then leads to:
- Robbing your intestines of the sources of healthy bacteria
- Reducing the food needed to feed healthy bacteria
- Reducing the proper development of your intestinal immune system, which regulates bacteria
This creates a perfect storm setting the stage for poor gut health. Let’s take a closer look at the storm.
Sources of Healthy Bacteria
As a child you require colonization with healthy bacteria, you are not born with them. Yes, you pick up some bacteria while in utero but you obtain a mega dose when you pass through your mother’s vaginal canal. You get even more through your mother’s breast milk. If you were born via c-section, not breastfed (or only breastfed for a few months) these are all lost opportunities for beneficial bacterial colonization.
While the practice of indiscriminate use of antibiotics is thankfully being reformed, this is another harmful practice for your intestinal microbiota. If you grew up on a farm, you had increased exposure to dirt, animals and bacteria and this has been shown to improve bacterial colonization and immune system health. However, if you are like many of us, you did not. If you combine a clean modern environment with overuse of antibacterial soaps, reduced breastfeeding and c-section birthing, you see how quickly these factors add up.
Feeding Your Microbiota (Bacteria)
Your beneficial bacteria have a chance to thrive if you’re eating a healthy diet, high in fruits and vegetables and low in processed foods and sugar. However, many of us have gone through periods of time where we overindulged in processed foods, ate too much junk food or overused alcohol. Even a sedentary lifestyle and poor sleep habits can negatively impact your beneficial bacteria.[11, 12] More bad news for our gut bacteria…
Proper Immune System Development Which Regulates Bacteria
So, you may lack the healthy colonization you should have obtained through mom and her breast milk. You may also have washed away good bacteria with antibiotics, and been deficient in ongoing bacterial contact through hygienic modern (non-farm-like) living. Poor diet may have further compounded this by not providing all the food these bacteria require. Not good.
How does this tie to your immune system? Your gut bacteria serve a major function of training your immune system. We often think it’s the bacteria themselves that make us healthier, and to some extent this is true. For example, some intestinal bacteria aid in the creation of certain vitamins. However, it is underappreciated that these bacteria lead to the proper formation and function of your immune system. Why does this matter?
- Because your immune system is a major, if not the primary, source of inflammation in your body.
- When you lack the healthy bacteria to regulate your immune system, your immune system becomes overactive and attacks when it shouldn’t.
- Inflammation is the weapon your immune system uses to attack things it does not like.
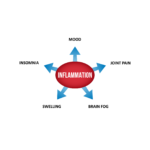
Let’s connect the dots and see how this can build into a vicious cycle:
The above scenario creates a vicious cycle. A cycle wherein you lack the healthy bacteria to regulate your immune system, thus creating an overactive immune system that attacks when it shouldn’t. Remember, that inflammation is the instrument your immune system uses to attack things it does not like.
Unhealthy Gut Bacteria = Inflammation
Inflammation = Symptoms
You may be surprised to know how many common conditions are caused by inflammation. Modern-day inflammatory conditions include (references to support these will follow later in the article):
- Fatigue:
- Inflammation can cause fatigue by creating imbalances in stress hormones; sometimes this is called adrenal fatigue (even though this term isn’t literally true, many may identify with it)
- Depression or Anxiety:
- When inflammation from the gut gets into the brain, it can alter your neurotransmitters or “happy mood” chemicals
- Brain Fog:
- When inflammation from the gut gets into the brain, it can cause brain fog (cloudy thinking)
- Insomnia:
- Inflammation in the digestive tract has been documented to cause insomnia
- Acne or Other Skin Conditions:
- It is often said that the skin is a reflection of the gut: a healthy gut equals healthy skin
- Female Hormone Imbalances:
- Inflammation can directly and indirectly alter the balance of female hormones and cause PMS (fatigue, irritability, bloating, altered cycle length or flow, low libido and hot flashes)
- Male Hormone Imbalances:
- Inflammation can cause male hormone imbalances, causing fatigue, low libido, erectile dysfunction, muscle loss, and poor memory
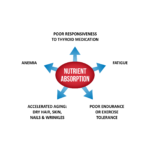
- Hypothyroid Symptoms:
- Inflammation damages your body’s ability to use thyroid hormone, so if your thyroid labs are normal or you are on a thyroid medication but still exhibiting hypothyroid symptoms, inflammation is likely the cause
- Immune System Dysregulation and Autoimmunity:
- Bacterial overgrowths or inflammation in the small intestine are connected with problems in the immune system, including conditions such as Hashimoto’s disease (autoimmune thyroid), celiac disease, irritable bowel syndrome, rheumatoid arthritis, food reactivity and inflammatory bowel disease (Crohn’s and ulcerative colitis).
The Destructive Self-Feeding Cycle People Can Get Stuck In
This poor bacterial colonization (aka an unhealthy microbiota) can lead to a poorly trained immune system and result in excessive inflammation. This inflammation can damage your good intestinal bacteria and damage your gut lining. This inflammation and damage furthers the dysfunction, and so starts a self-feeding cycle.
It’s important to point out that inflammation is poisonous to healthy bacteria.[13, 14, 15, 16]
In the most severe cases, this cycle manifests as inflammatory bowel disease which by definition can lead to an immune attack against your healthy, resident bacteria.[17]
This sounds terrible, and it can be, however there is also A LOT you can do to improve the health of your gut. So please do not worry, as is the tendency for people to do when not feeling well. You can improve, there is much you can do, and this cycle can fairly easily be unwound. Then you can become stuck in a self-perpetuating cycle of healing and improvement. Thankfully, probiotics can help break this cycle.
Probiotics are living microorganisms that provide health benefits to their host. Most people have around a thousand different bacterial species occupying their gut, this is collectively known as their microbiota. We co-evolved with bacteria in what is known as a symbiotic relationship; we help them and they help us.
How Do Probiotics Help You?
The Journal of Clinical Gastroenterology[18] and the journal Trends in Microbiology[19] offer insights regarding how probiotics make you healthier.
Probiotics can:
- Increase bacterial diversity, or health, of your bacterial community.[20]
- Fight pathogens (harmful bugs) and their toxins.
- Promote a more rapid recovery from imbalances in your gut organisms.
- Promote a healthy immune response in your gut.[21, 22]
- Reduce gut inflammation (remember excessive inflammation is part of an overzealous immune response).[20]
- Encourage the growth of healthier microbes in your gut.[21]
- Reduce leaky gut aka damage to your gut lining.[23, 24, 25]
Said simply, probiotics can help improve the balance of organisms in your gut, reduce overzealous immune system activity and reduce the inflammation which many of us suffer with.
An important point to emphasize is that probiotics are antibacterial, antifungal and antiparasitic. This is, in part, how they help promote a healthier community of organisms in your gut, they clean out the bad bugs.
Probiotics Heal The Gut – The Gut Affects Almost Everything
We can boil the impact of gut health down to these root fundamentals:
|
Immune System |
Inflammation |
Nutrient Absorption |
Immune System
Your small intestine contains the largest density of immune cells in your body.[26] This is one reason why the health of your digestive tract and the health of your immune system are so closely linked. If your gut bacteria are unbalanced, your immune system may be chronically activated into an overzealous response.[27, 28]
Inflammation
An overzealous immune system produces inflammation in the gut and elsewhere in the body. Chronic inflammation is a major factor in many health conditions, including rheumatoid arthritis[29], and cardiovascular disease.[30, 31]
Nutrient Absorption
Inflammation also damages the lining of the digestive system.[32] This can impair nutrient absorption. If you eat a healthy diet but don’t absorb nutrients well, this can be similar to eating an unhealthy diet.
Most Probiotics Do Not Colonize You
This is well known. To quote a recent article from the journal Nature:
“The gut microbiota generally shows colonization resistance, in which the native microbiota prohibits harmful [pathogenic] and potentially beneficial [probiotic] microbes from establishing.”[33]
This is a good thing. This means your gut microbiota is resistant to colonization from bad bugs, but it also means you can’t take probiotics and expect them to “stick.” Most probiotics don’t work by forming colonies in your gut. Rather, they help to improve the health of your gut microbiota as they make their way through your gut and before coming out in your stool. They are mostly transient helpers, improving gut health as they make their way through your gut.
Diet is a great source of probiotics. Below is a table of common foods that are high in probiotics compared with probiotic supplements. As you can see, a challenge with diet is that it is difficult to obtain the same dose used in the research studies. So I would consider adding probiotic supplementation to your diet for optimum results.
| Food | Species | Amount | Equivalent Dose |
| Sauerkraut | Leuconostoc mesenteroides Lactobacillus brevis Pediococcus pentosaceus Lactobacillus plantarum | 3 billion CFU per cup | ⅛ capsule Lacto-Bifido Blend Probiotic |
| Yogurt[34, 35] | Lactobacillus acidophilus Streptococcus thermophilus Lactobacillus delbrueckii subsp. bulgaricus | 2.5 billion CFU per cup | 1/10 capsule Lacto-Bifido Blend Probiotic |
| Lacto-fermented Pickles[36, 37] | Lactobacillus casei Lactobacillus rhamnosus Lactobacillus plantarum Lactobacillus brevis | 1.3 billion CFU per pickle | .05 capsule Lacto-Bifido Blend Probiotic |
| Kefir[38] | Lactobacillus brevis Lactobacillus acidophilus Lactobacillus casei Lactococcus lactis Saccharomyces cerevisiae | 2.5 billion CFU per cup | 1/10 capsule Lacto-Bifido Blend Probiotic |
| Kimchi[39, 40] | Weissella koreensis Lactobacillus sakei Lactobacillus graminis Weissella cibaria Leuconostoc mesenteroides | 11.5 billion CFU per ½ cup | ½ capsule Lacto-Bifido Blend Probiotic |
Here is something I’d like to share, that most supplement companies don’t want you to know. Probiotics can be organized into 3 categories. Meaning nearly every probiotic product can be classified into one of three categories.[41] Why this is never disclosed is because not knowing this keeps you on the probiotic merry-go-round.
Have you ever compared the ingredients in two different shampoos? If so, you have probably noticed that even though they claim different things, one might be for adding volume and the other might be for fighting gray hairs, the ingredients are almost identical. Marketers are always looking to find new ways to market the same thing. This also happens with probiotics.
This is great news. This means you don’t need to try every probiotic on the market, but rather use one quality formula from each category, together. Wait a few weeks and reevaluate. That’s it.

Why does this work so well? To support balance in your gut it is often best to use 3 supports similar to a 3 legged stool approach.
I’ll go into the scientific support for this 3 category system and provide specific product recommendations in a moment, but first, let’s define the three categories.
| CATEGORY 1 | CATEGORY 2 | CATEGORY 3 |
| Lactobacillus & bifidobacterium species predominated blends | Saccharomyces Boulardii (a healthy fungus) | Soil-Based Probiotics using various bacillus species |
Category 1 – Lactobacillus & Bifidobacterium Predominated Blends
These are the most well-researched, with over 500 trials assessing their validity.
These live microorganisms are commonly used in foods such as yogurt, kefir and lacto-fermented sauerkraut. Also known as lactic-acid producing probiotic bacteria, they consume carbohydrates and produce lactic acid. They typically do not colonize the host, but do improve the health of the host.
This category of probiotics usually contains a blend of various Lactobacillus strains and bifidobacterium strains.
- Most lactobacilli are transient but important; there are over a hundred species.
- Bifidobacteria typically reside in the large intestine; there are over thirty species.
Here are some of the documented beneficial effects from this category of probiotic bacteria:
- Clinical research shows that Category 1 strains promote optimal gastrointestinal function, a healthy inflammatory response, and the ability to support a healthy and balanced microbiota.[43]
- Preliminary research suggests that Category 1 probiotics work to reduce anxiety.[44]
A review of studies into the biological effects of probiotics on Inflammatory Bowel Disease[45] found multiple beneficial effects. These include:
- Reducing factors that cause inflammation
- Modulating the immune system
- Producing beneficial substances in the gut (proteins, short-chain fatty acids, and immunoglobulins)
- Reducing factors that cause biofilm production
Another review[46] looked at the role of probiotics in allergic and inflammatory conditions. Category 1 probiotics were widely used in the research and shown to be beneficial in treating:
- Infantile diarrhea
- Vaginal infections
- Urinary tract infections
- Tooth decay, diabetes, cancers
- and more…
- Probiotics also seem to help with lactose intolerance
An exciting body of research has found category 1 probiotics are helpful in patients with depression.[47]
Another review looked at the results of studies using probiotics for small intestinal bacterial overgrowth (SIBO). Again, Category 1 probiotics were commonly studied. Researchers found that probiotics are effective for reducing bacterial overgrowths and gas production as well as improving abdominal pain.[48]
Category 2 – Saccharomyces Boulardii
The second most researched probiotic, with over 100 studies. Saccharomyces boulardii (S. boulardii for short) is a healthy fungus. S. boulardii is not a normal part of the human microbiota, meaning it does not colonize us. S. boulardii has been used successfully for:
Saccharomyces boulardii helps fight the bad bugs
This live microorganism is antifungal and can help fight fungal (candida) overgrowths in your intestines. It does this in part by breaking down the protective layer (biofilm) that forms over fungus.[54]
S. boulardii has been shown effective in treating digestive tract parasites such as entamoebas, giardia, and Blastocystis hominis.[55] When antibiotics are co-administered with S. boulardii, it increases success compared to antibiotics alone.[56]
Even more exciting, S. boulardii has been shown to be as effective as the antibiotic metronidazole (Flagyl) in treating Blastocystis hominis (a potential gut pathogen/infection).[49]
S. boulardii has also shown the ability to increase clearance of H. pylori infection, according to systematic reviews with meta-analyses[57] and according to clinical trials.[58]
Although S. boulardii does not appear to colonize,[59] it has shown some pretty impressive results, including the ability to correct dysbiosis (imbalances in your microbiota).[60]
Category 3 – Soil-Based Probiotics (Bacillus Species)
The third most researched category of probiotics is soil-based probiotics. This group has roughly 15 clinical trials evaluating their effectiveness. These live microorganisms are also known as non-lactic acid forming bacteria and sometimes also referred to as spore-forming bacteria. Scientists like making names complicated. This category of probiotic can colonize the host.[42]
Again, these are also known as spore-forming bacteria or soil-based organisms. This is because they are found everywhere in soil and water, and they often spend part of their life cycle in the dormant “spore” state.
These may be an important type of probiotic to include in supplemental programs because they may help replace what we are missing due to our reduced contact with soil and natural environments.
A number of soil-based species[61] show health benefits, including Bacillus coagulans and Bacillus subtilis. This type of probiotic, like many others, has been shown to improve and balance the community of bacteria in your gut. Research shows that this category of probiotics can:
- Improve diarrhea, abdominal pain, bloating, and stool consistency in IBS patients[62, 63, 64, 65, 66, 67, 68, 69, 70]
- Reduce symptoms of acute diarrhea[71]
- Have a slight benefit on constipation. Not all the studies show this[62, 72, 73, 74, 75, 76]
- Decrease leaky gut[77]
- Decrease inflammation[61, 78]
- Decrease adverse events from antibiotics[79]
- Decrease respiratory tract infections
- Build a healthier microbiota
- Decrease post-exertional muscle soreness
- Secrete antimicrobial peptides, meaning probiotics are actually antimicrobial
Some bacilli bacteria are harmful, so use well-labeled and tested strains. These types of probiotics should be avoided in critically ill patients but otherwise are very safe.[80]
3-Category Summary
There are other probiotic bacteria strains that fall outside of these three categories, but the category system covers 90% of strains. After nearly ten years of treating patients with a litany of various GI disorders, I am confident that if you focus on this 3-category protocol, you can see substantial improvement in your health.
That said, probiotics are not a cure all and sometimes other, more advanced, therapies are needed. If this interests you, please see Healthy Gut, Healthy You which provides a detailed guide for what else you can do to heal your gut beyond probiotics.
Taking All 3 Probiotics At Once = Powerful Results
I’m hoping to motivate you to go beyond simply taking one probiotic (ie: one category), but rather supercharging your probiotic protocol by using all 3 categories (3 probiotics) at once. In my experience this has been the difference between people experiencing minimal or impressive results. I’ll detail this protocol in a moment.
Here is a science-based summary of the therapeutic benefit of probiotics.
High-level scientific support for:
- IBS: Gas, bloating, diarrhea, constipation, abdominal pain
- IBD: Crohn’s and ulcerative colitis
- Mood: Depression and anxiety
- Gut microbiota imbalance: SIBO, H. pylori, candida/fungus, pathogens
- Leaky gut aka gut damage and permeability
Limited, but encouraging, scientific support for:
- Cognition
- Sleep
- Thyroid health
- Female hormones
- Autoimmune conditions
- Metabolism
- Blood pressure and cholesterol
- Brain fog
- Sleep
| Probiotics Support These Conditions | ||
| High level of scientific support for: | ||
| Irritable Bowel Syndrome (IBS) Gas, bloating, diarrhea, constipation, abdominal pain |
Inflammatory Bowel Diseases (IBD) Crohn’s disease and ulcerative colitis |
Mood Depression and Anxiety |
| Gut Imbalances SIBO, H. pylori, candida/fungus, pathogens |
Leaky Gut Gut damage and permeability |
Infections Vaginal infections, urinary tract infections, tooth decay |
| Limited, but encouraging, scientific support for: | ||
| Cognition Cognitive function, brain fog |
Hormonal Health Thyroid health, PCOS, endometriosis, bone density |
Allergies Dairy intolerance, seasonal allergies |
| Autoimmune Conditions Type 1 diabetes, multiple sclerosis, rheumatoid arthritis |
Metabolic Health Blood sugar, cholesterol, blood pressure, weight loss |
Sleep Sleep quality and Disruption |
Below we will detail what the scientific research with probiotics has found. This will be a review of high quality scientific support.
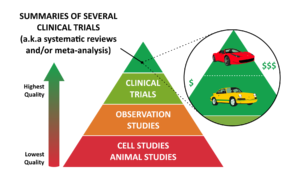
Why the emphasis on high quality?
To protect you from inaccurate advice. The balance here is usually between two extremes:
- Your doctor might make a remark such as “there is no evidence for probiotics.”
- Online marketers who proclaim probiotics as a cure all.
Of course most doctors are only trying to help, but might not have the time to stay current with the research. Sadly, instead of saying “I haven’t kept up with the probiotic research” most doctors default to an understandable stance of circumspection.
Internet marketers routinely use junk science to tell you their ‘product is scientifically proven’. What they leave out is that it’s been ‘proven’ to help a rat or a petri dish, not humans.
Here is an example I will never forget. I was attending a lecture by a health guru who razzle dazzled the audience with how promising this ‘new fiber’ was for weight loss. There were mechanistic diagrams and colorful charts showing how this fiber would lead to ‘weight loss on a cellular level‘. I sat there fuming knowing that we have already tested this in humans! Guess what the results showed? About 2-3 pounds of average weight loss in subjects who were already obese.[81]
You see, one can find a mechanism study (often done in petri dishes aka cell studies) or an animal study (often done in rats) to support almost anything. An honest, disciplined and responsible scientist will not cherry pick from low-quality science like this, but rather tell you what results we have when we test these theories in humans, in what are known as clinical trials. This is putting the truth first, not one’s agenda.
As you can see from our pyramid diagram, the pinnacle of scientific evidence is the systematic review or meta-analysis which are summaries of several clinical trials. You will see I have cited a host of this type of pinnacle evidence in this article.
Probiotics have been shown helpful for the symptoms of IBS, which include constipation, loose stools, diarrhea, abdominal pain and gas.
Proof
Two meta-analyses have shown probiotics to be an effective treatment for IBS, with no side effects. A multi-strain mixture containing a blend of predominantly lactobacillus and Bifidobacterium strains is best (category 1).[82, 83]
Reminder: A meta-analysis is a summary of clinical trials, and is the highest level of scientific evidence.
When reporting
“Two meta-analyses have shown probiotics to be an effective treatment for IBS”
What does this mean?
- It means that over 1,100 patients were tracked in order to assess how effective probiotics were for IBS. The subjects were given either probiotics or placebo, thus guarding against the placebo effect.
- After a number of weeks a follow up analysis of the subjects symptoms were conducted and there was clearly and consistently more benefit documented in those using probiotics than in those on placebo.
This is huge.
This is the type of high quality data you as the healthcare consumer needs.
- Using high quality data greatly increases the likelihood you will experience the same benefit noted in the study.
- Low quality data (animal or petri dish studies) have an extremely LOW likelihood you will experience the desired result.
In another meta-analysis[84], the results of twenty clinical trials were reviewed with a total of 1,404 subjects. In all studies, subjects were given either probiotics or placebo, thus guarding against the placebo effect. The probiotic group showed improvement in global IBS symptoms when compared to the placebo group. This includes improvements in:
- Constipation, diarrhea and or loose stools
- Abdominal pain
- Bloating
- Flatulence
- Food Intolerance
- Fatigue and Difficulty Sleeping
Further research continues to be published. A large clinical trial (330 patients) was published in 2020 and shows that probiotics significantly reduce abdominal pain and abdominal distension in IBS patients.[85] Subjects taking probiotics experienced a significant normalization in stool consistency and improvements in quality of life when compared to placebo.
The compelling data above are likely why the Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS) recommends a trial on probiotics for IBS.[86]
Certain circles on the internet claim you should not take probiotics for SIBO (small intestine bacterial overgrowth) because in SIBO you already have too much bacteria. However, looking at the research,
we CLEARLY see probiotics help with SIBO
and may even be effective as a stand-alone treatment.
We also have evidence showing that some probiotics are as effective as antifungal drugs in treating fungi and that probiotics are as effective as antiparasitic medications in treating parasites. The antibacterial effect of probiotics can help to reduce bacterial overgrowths, correct imbalances, and clear infections.
Proof
Probiotics have been shown to be effective in treating SIBO (small intestinal bacterial overgrowth), both in improving symptoms and in improving lab values.[48] The clinical trials here were even summarized in a meta-analysis, concluding that probiotics are an effective therapy for SIBO. One study found probiotics to be more effective when compared directly to the antibiotic metronidazole.[87]
Two types of probiotics have been shown effective for SIBO. One, a blend of lactobacillus & Bifidobacterium strains (category 1). Two, a probiotic containing bacillus strains, aka soil-based probiotics (category 3). More evidence supports a blend of Lactobacillus and bifidobacterium.
Data from 18 clinical trials were summarized in a meta-analysis, which concluded that probiotics are an effective treatment for SIBO.[48] Specifically:
- Probiotics reduce bacterial overgrowths in SIBO patients
- Probiotics reduce hydrogen concentrations in SIBO patients
- SIBO patients who take probiotics experience symptom improvement
- SIBO patients who take probiotics experience marked reductions in abdominal pain
A wide variety of probiotic strains were used in these clinical trials, however all of them fall into Category 1 or Category 3.[87]
Probiotics might outperform antibiotics
This exciting study[87] was conducted in 50 subjects diagnosed with SIBO and who had chronic abdominal distention.
- Treatment:
- Half of the subjects were treated with metronidazole (Flagyl);
- Half took a multi-strain probiotic (Category 1).
- Results:
- 52% of the subjects taking metronidazole showed improvement in symptoms,
- 82% of those taking the probiotic improved.
- Conclusion:
- Probiotics were more effective than standard antibiotic treatments for patients with SIBO and chronic abdominal distension.
Probiotics might work better if you have bacterial overgrowth (SIBO)
Another exciting study found that probiotics work better for digestive symptoms if you also have SIBO (small intestinal bacterial overgrowth), as compared to those who have digestive symptoms without SIBO.[88]
- Patients with both IBS and SIBO showed a 71.3% reduction in their total IBS score
- IBS patients without SIBO only showed a 10.6% reduction

In this case a combination of Category 1 and Category 2 probiotics were used.
So, probiotics can improve digestive symptoms, combat SIBO and may work better if you have symptoms (IBS) and SIBO.
Probiotics for H. pylori infection
A review published in 2020 determined that probiotics are a useful complement to traditional treatments for H. pylori. Probiotic supplementation improves the effectiveness of standard H. pylori treatment and reduces side effects of antibiotic therapy.[89]
Probiotics for leaky gut
Can probiotics help with Leaky Gut? One small clinical trial found that probiotics helped to promote intestinal repair in humans.[77] Another trial found positive effects of probiotics when used to treat intestinal impairment after a GI infection.[24]
Probiotics for fungus, candida, and parasites
We also have evidence showing that some probiotics are as effective as antifungal drugs in treating fungi.
In a study of 181 infants, S. boulardii (a Category 2 probiotic) was as effective as Nystatin (an antifungal medication) in reducing fungal infection and improved food intolerances.[90]
Probiotics have also been shown to have antiparasitic benefits.
- In a clinical trial of 65 adults infected with giardia (a protozoa),
- One group was given standard treatment with metronidazole.
- A second group was given metronidazole and S. boulardii (Category 2).
- Results showed full recovery from the infection for patients taking a combination of medication and probiotics.
- In the group taking medication only, 17.1% of subjects were still infected with giardia cysts 4 weeks after treatment.[55]
Another study[49] shows that probiotics can be more effective than standard antiparasitic drug treatment. In this study of children with Blastocystis hominis infection, a comparison was made between treatment with Saccharomyces boulardii (Category 2) and a standard drug (metronidazole).
- After one month, stool samples for both groups showed similar cure rates.
- The children who took probiotics had much better improvement in their gastrointestinal symptoms.
This included many of the symptoms of IBS which are also seen in ulcerative colitis and Crohn’s disease.
IBD is usually diagnosed as either ulcerative colitis or Crohn’s disease, although there are other less-common types of colitis. These are all conditions where there is a high level of inflammation in the gut which is often caused by autoimmunity against intestinal tissue or intestinal bacteria.
Probiotics have been shown to be very helpful for IBD.
Proof
A recent review showed that in Crohn’s disease, the probiotic VSL#3 (Category 1) worked as effectively as the medication mesalamine in maintaining remission. But the best evidence was for the probiotic Saccharomyces boulardii (Category 2) used with the anti-inflammatory drug mesalamine.[91]
Another review found the best approach for treating active ulcerative colitis was with VSL#3 (a Category 1 blend) combined with an anti-inflammatory drug.[91]
Other reviews have found probiotics (specifically a Lactobacillus and Bifidobacterium blend aka category 1 probiotics) to be equally effective for ulcerative colitis as anti-inflammatory drugs like mesalamine.[92]
One systematic review has found probiotics do not help maintain remission, but overall the data suggest probiotics are helpful.[93]
Gastroesophageal reflux disease (GERD) is a condition where stomach acid flows backwards towards the mouth.
A recent systematic review of 12 studies found that 79% of studies reported positive outcomes when GERD was treated with probiotics, including reduced regurgitation, improvements in reflux, heartburn, indigestion, nausea and gas-related symptoms like burping.[94]
Two recent and very-high quality studies recently combed through the available research into probiotics for constipation and both produced similar results:
- A systematic review of 17 randomized control trials (with 1469 patients) concluded that probiotics significantly increased stool frequency by an average of 1.29 bowel movements per week. Compared with placebo, patients using probiotics experienced a shorter gut transit time by an average of 12.36 hours.[95]
- A meta-analysis of 15 randomized control trials showed that probiotics increased the stool frequency by 0.98 bowel movements per week and significantly reduced gut transit time by 13.75 hours.[96] The research also showed that multistrain probiotics were more effective than single strain probiotics for increasing stool frequency, improving stool consistency and reducing bloating.
A study of 80 patients with mild, intermittent constipation found that 7 weeks of soil-based probiotics (bacillus coagulans) led to improved gut transit time, more complete bowel movements, and less abdominal discomfort.[97]
A Randomized Control Trial involving 100 infants and children from 3-36 months old with acute diarrhea found that the time of recovery from diarrhea was significantly shorter in the probiotic group (S. boulardii) compared with the placebo (65.8 hours vs. 95.3 hours).[98]
The prestigious Journal of the American Medical Association published a meta-analysis of 82 randomized control trials. They found all three categories of probiotics worked equally for antibiotic-associated diarrhea.[99]
Three additional meta-analysis have also concluded that probiotics work to prevent antibiotic-associated diarrhea.[99, 100, 101]
A systematic review and meta-analysis found that probiotics are effective for preventing traveler’s diarrhea.[50]
- Probiotic consumption decreases the incidence of respiratory tract infections in children.[102]
- Probiotics may be helpful in preventing recurrent urinary tract infections in women.[103]
- Probiotic supplements are safe and beneficial for the treatment of vaginal infections.[104]
- Probiotics decrease oral pathogens that cause cavities, gingivitis and periodontal disease and may be beneficial for maintenance of oral health.[105]
How can something that improves the health of your gut, like probiotics, aid with mood problems like depression and anxiety? This happens through what’s known as the gut–brain connection. We know when there is inflammation in the intestines, it can also cause inflammation in the brain.
Proof
The Journal of Affective Disorders published a meta-analysis of 10 clinical trials with a total of 1,349 subjects.[106] They compared the effect of probiotics versus placebo on mood. What did they find?
“significant improvements in the moods of individuals with mild to moderate depressive symptoms and non-significant effects in healthy individuals”
So, if you have depression, probiotics may help. If your mood is fine, then they won’t. Makes sense.
Two more systematic reviews with meta-analysis of clinical trials have found probiotics lead to a significant reduction in depression.[47, 107] One review found that probiotics were especially beneficial in patients with major depressive disorder.[107] In addition, multiple strains of probiotics were more effective in reducing depressive symptoms.[107]
There is also data showing anxiety can be improved from probiotics. The data here are not as strong, but still have documented an anti-anxiety effect, in human clinical trials.[108, 109]
In related studies, there is also data from human clinical trials that probiotics can dampen symptoms of stress in healthy adults.[110, 111, 112, 113]
What is ‘the best probiotic for depression or anxiety’?
Here is some empowering news from the Annals of General Psychiatry, the dose and type of probiotic varied among the above studies.[114] What this means is that you do not need a special ‘mood enhancing probiotic’ to improve your mood with a probiotic supplement. Why?
- Probiotics are not drugs, they do not act with a narrow and specific action.
- Rather, by improving your gut health probiotics can lead to an array of benefits, including improved mood.
- This is the gut-brain connection.
So, the goal is to find the right probiotic for the individual and not the right probiotic for the condition. This is exactly what the 3-category system does. So, if you’re suffering with depression or anxiety, we can focus on using the simple 3-category system to heal what might be the underlying cause of your symptoms, your gut! And not get distracted by the marketing claims of “this is THE probiotic for depression or anxiety.”
Data here are preliminary but encouraging. Research has found increased brain fog, aka lack of coherence, in those with IBS.[115] We have discussed the impressive evidence substantiating probiotics can improve IBS. So, we can draw a tenable inference here that if IBS occurs with brain fog, reducing IBS could reduce brain fog.
Proof
A 2020 Meta-analysis looked at 7 human and 11 animal studies. Researchers concluded that probiotics enhanced cognitive function. Effects of probiotics on cognitively impaired individuals were greater than those on healthy ones.[116]
Brain fog, or fuzzy thinking, isn’t usually studied in isolation but we can look at other disease-model studies where probiotics have improved cognition. This includes probiotics improving cognitive function in:
Here’s an interesting study of 4th year medical students. The trial was done over a 2 year period during times of exam stress. Students who took a Category 1 probiotic showed superior sleep quality. So, probiotics seem to help with sleep quality during times of stress.[121]
In a clinical trial, participants reported that their sleep quality improved after 6 weeks of taking probiotics.[122]
Another clinical trial of IBS patients showed sleep improvements for diarrhea-type IBS patients. The same results were not seen for constipation-type mixed-type IBS patients.[123]
A third study of subjects with depression showed that the group taking probiotics had less sleep disruption than the placebo group.[124]
One very small study of men with mild insomnia also found beneficial effects on sleep when taking probiotics.[125]
This is another area where data are sparse. However, there are some encouraging preliminary findings. These are highlights from a research review that focused on probiotic treatment and autoimmune disease.[126]
Proof
Type 1 Diabetes
- In a large and very interesting study of 7,473 children at risk for type 1 diabetes, early probiotic supplementation was shown to reduce the risk of autoimmunity when compared to children who had not taken probiotics or had been given probiotics more than 27 days after birth.[127]
Multiple Sclerosis (MS)
- Another study found that probiotic treatment can have positive outcomes for patients with multiple sclerosis.
- In this double-blind study of 60 subjects, half of the MS patients took a Category 1 probiotic for 12 weeks. The other half took a placebo.
- Patients treated with the probiotic showed less disability, lower insulin resistance and fewer inflammatory markers.[128]
Rheumatoid Arthritis (RA)
Three different studies found mixed results for probiotics in RA disease activity. One study did not show significant improvement while two other studies did show improvements.[129, 130, 131]
- The specific findings from study to study vary, but they all show improvements in some of the following:
- joint swelling and tenderness
- pain
- inflammatory markers
- function
- imaging findings
The authors of this research review noted that intestinal dysbiosis is seen in autoimmune disease.[132] Specifically, autoimmune patients have:
- decreased bacterial function and diversity
- impaired gut barrier function
- increased inflammation
- autoimmunity
Does this sound familiar from our earlier discussion?
This is another semi-inferential connection. This has not been studied robustly yet, but from the preliminary data we do have, it does appear the small intestinal bacterial overgrowth affects metabolism. The good news here is that probiotics can combat small intestinal bacterial overgrowth.
First of all, we have three studies showing a relationship between SIBO and body weight:
- Two studies support the connection between SIBO and metabolism. In these studies, patients who tested positive for SIBO had higher BMI scores than patients without SIBO.[133, 134] However, not all the data show SIBO correlates to weight gain.[135]
Next, we can look at studies that are trying to unravel the reasons why methane gas in SIBO is associated with obesity.
- Two studies look at the role of methane-producing bacteria M. Smithii in obesity.
- What might be happening is that this bacteria is involved in helping you to extract extra calories from your diet, leading to weight gain.[136, 137]
Can treating SIBO improve your metabolism?
Finally, there is some preliminary evidence that shows treating SIBO may help improve blood sugar, cholesterol, and even reduce weight.[138]
Histamine intolerance symptoms look a lot like seasonal or food allergies, however it’s actually caused by a buildup of histamine in the body.
Histamines can be consumed as food and histamine patients should take steps to lower their dietary intake. However, histamine usually becomes a problem as a result of gut bacteria imbalances which cause histamines to build up.
Gut dysbiosis leads to a build-up of histamine, both directly and indirectly:
- Bad bacteria in the gut produce excess histamine.
- A damaged intestinal lining (also known as leaky gut) cannot process histamine into other compounds.
- Damage to the intestinal lining also leads to immune system activation and reactivity, producing more histamine.
It’s likely that probiotics can lower histamine, however some controversy exists. We don’t have any direct research here, but we can make some educated inferences, based on three areas of research:
1. Studies make a direct connection between histamine intolerance and gut conditions:
- This study found that 30-55% of patients with digestive symptoms may also have histamine intolerance.[139]
- In this study, patients with histamine intolerance were more likely to test positive for gut bacteria imbalances and leaky gut when compared with controls.[140]
2. Research clearly shows that probiotics are effective against gut conditions, including:
- SIBO [48, 87, 88]
- H. pylori, fungus, protozoa and parasitic infections[49, 55, 89, 90]
- Leaky gut [23, 24, 25, 77]
3. Preliminary evidence suggests that probiotics can be effective against histamine-type symptoms:
- A meta-analysis and a more recent clinical trial concluded that probiotics significantly reduced symptoms and clinical markers in patients with allergic rhinitis.[141, 142]
- The use of probiotic bacteria for the prevention and/or treatment of allergic disease have shown promising results to date. However, the validity of these findings need to be confirmed by further randomized controlled trials.
All of this research indirectly suggests that there’s a role for probiotics in treating histamine intolerance. Since probiotics are very safe, a probiotic trial is a good idea for patients with histamine intolerance.
Some practitioners recommend taking a low-histamine probiotic product. However, this recommendation overlooks the net beneficial effect of probiotics on the gut ecosystem. Any quality probiotic supplement will help to reduce histamine levels.
Lactose Intolerance
A systematic review of 15 clinical trials found that
probiotics can improve dairy tolerance.[143]
Good news for dairy lovers! Some evidence suggests the reason probiotics lead to improved dairy tolerance is because they positively impact your intestinal bacteria aka microbiota.
Gluten Intolerance
- Excitingly, one preliminary study found that, for patients with non-celiac gluten sensitivity, a gluten-free diet combined with probiotics was more effective than a gluten-free diet alone.[144]
- For celiac patients already on a gluten free diet, but still experiencing digestive symptoms, probiotics have been shown to reduce symptoms.[145]
Seasonal Allergy
A meta-analysis of 22 randomized control trials concluded that
probiotics can improve seasonal allergy.[146]
Why? Remember your gut has a substantial impact on your immune system, healthier immune system = less allergy. Other high-quality studies support this same finding.[147]
There is also data, albeit mixed, suggesting that probiotics given to children may prevent or reduce formation of allergy.[148]
A study of 250 children with allergic rhinitis treated with steroids/antihistamines found that after 3 months the probiotic group had a significant reduction in symptoms and less need for conventional medication compared to the placebo group.[149]
We don’t have good data regarding female hormones and probiotics, but we can make some inferences based on other research:
- We know that the gut microbiota is involved in regulating estrogens and that gut dysbiosis can disturb estrogen levels.[150]
- A research review and one additional study indicates that women with certain health conditions have lower diversity in their intestinal bacteria.[150, 151] These conditions are all associated with unbalanced estrogen levels (for example: PCOS, obesity, endometriosis, cardiovascular disease, and breast cancer).
- One study found that probiotics plus soy isoflavones improved bone density.[152]
- There is also preliminary evidence that these types of health conditions can improve when bacterial diversity in the gut increases.[150] This is where probiotics may come in.
One very recent meta-analysis confirms that we are on the right path with these inferences.[10] The authors looked at 13 studies involving 855 women diagnosed with PCOS and found that probiotic use improved hormonal and inflammatory markers for these women.

In the clinic, I have been amazed at how easy it is to improve female hormone symptoms by focusing on gut health. Additionally, some cases may also require female hormone balancing herbs. This is the same approach I detail in Healthy Gut, Healthy You. I’m thankful for the many women who shared their stories here.
When it comes to blood pressure and cholesterol, we have five meta-analyses (the highest quality of research data available), so this is worth a look. The results are a bit mixed, however the majority of results do show benefits
Four meta-analyses found that probiotic supplements can improve overall cholesterol profiles. One of these studies also shows significant improvements to blood pressure. All together these four meta-analyses evaluated 68 clinical trials with 3885 patients.[153, 154, 155, 156]
Another meta-analysis found probiotics had a significant effect on reducing LDL Cholesterol. However, there was no effect on blood pressure or any other cholesterol readings. This meta analysis evaluated 9 clinical studies with 678 participants with pre-diabetes.[157]
Another interesting study found that probiotics can lower homocysteine,[158] which is an independent risk factor for heart disease. How did the probiotic lower homocysteine? The probiotic increased healthy bacteria levels in the gut, these bacterial changes lead to increased B vitamin production (intestinal bacteria produce certain B vitamins) and this then lead to decreased homocysteine levels.
The effect size in these studies is usually small, but favorable. So, probiotics should not be viewed as the primary therapy for high cholesterol or blood pressure.
There are some exciting data documenting the gut-thyroid connection which suggest probiotics may improve thyroid health.
Proof
A fascinating study from the World Journal of Gastroenterology[159] found that being hypothyroid or on thyroid medication were the most closely associated with SIBO (small intestinal bacterial overgrowth). This was after analyzing 1,809 for the following factors and their association to SIBO.
- Surgical removal of the stomach
- PPI drug therapy (to reduce stomach acid)
- Surgical removal of portions of the colon or stomach
- Stenosis (narrowing of the intestinal canal)
- Gastroparesis (delayed stomach emptying)
- Neuropathy (nerve damage)
- Immunosuppressive drug therapy
- Hypothyroid or levothyroxine use
- Diabetes type 2
This shocked the researchers and was an eye-opening finding regarding the gut-thyroid connection. Again, of all the above listed factors,
being hypothyroid or on thyroid medication were the most highly associated with SIBO.
Another study[160] also found that thyroid autoimmunity was higher in those with SIBO as compared to healthy controls. Remember that thyroid autoimmunity is the underlying cause of most hypothyroidism.
Can gut bugs besides SIBO impact thyroid through the gut-thyroid connection?
Yes. A recent meta-analysis (summary of clinical trials, highest level evidence) has concluded there is an association with the bacteria H. pylori to thyroid autoimmunity.[161] And while the data here don’t definitively associate H. pylori with hypothyroid, it is exciting to consider the possible benefit probiotics could have on thyroid health as probiotics have anti-H. pylori capability.
What can you do about this? Good news, a meta-analysis has found that Saccharomyces boulardii probiotic (Category 2) can aid in clearing the H. pylori bacteria.[58]
In recap, SIBO and H. pylori are both associated with hypothyroidism. Thankfully, probiotics can combat both SIBO and H. pylori. Category 1 and 3 probiotics have the best evidence for SIBO. Category 2 probiotics have the best evidence for H. pylori.
Best probiotic for the gut-thyroid connection
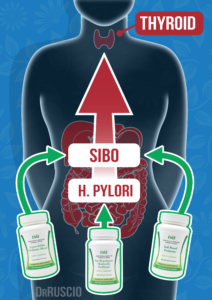
Consider this. We have discussed a SIBO-thyroid connection and H. pylori-thyroid connection. We have also discussed that two types of probiotics can combat SIBO (Category 1 and 3) and one type can combat H. pylori (Category 2). This is why I developed the 3-category system for probiotics. When you see the big picture, you realize that the probiotic research essentially boils down to only needing 3 probiotics to cover your probiotic needs. Then, you can get off the probiotic merry-go-round of marketing claims for a specific probiotic for a given condition. Let’s expand upon how you can use this information to create your own, personalized probiotic protocol.
Caution: If you have any of the above conditions (infection, IBD, depression, hypothyroidism) please see a qualified healthcare provider.
Is there a gut-skin connection?
The skin and the gut have similarities in their structure, they play similar roles in immune function and both host a diverse bacterial population.[162] Evidence suggests that intestinal health and skin health are closely linked.[163, 164]
A recent review paper summarized the research into acne and the microbiome and confirms the connection.[165] The 3 clinical trials reviewed in the paper provide the strongest evidence:
- 2 clinical trials showed that topical probiotic treatments were effective for treating acne.[166, 167]
Probiotics as effective as acne-antibiotics:
- Another study compared traditional antibiotic therapy for acne with a probiotic supplement. The young women in both groups showed significant improvement after 4 weeks, although some in the antibiotic group dropped out because they got yeast infections. A third group that was treated with both antibiotics and probiotics had the best results.[168]
Two clinical trials have found clinical improvements when probiotic supplements are used to treat dermatitis.[169, 170]
Another systematic review suggests that a combination of oral and topical probiotics may be most helpful for skin conditions such as rosacea, acne, and atopic dermatitis.[171]
Probiotics have also been found helpful for sensitive skin. In a clinical trial of women with sensitive skin, a probiotic cream was shown to reduce skin sensitivity, increase skin hydration and make the skin more resistant to damage.[172]
We will detail recommendations for infants and moms later. For now, here is the short summary.
Researchers have found benefits from probiotic use for infants, including:[173]
- Less colic and irritability
- Less diarrhea
- Fewer spitting episodes
- Fewer respiratory infections
Researchers have also found benefits for preterm infants. Probiotics were associated with lower rates of mortality and necrotizing enterocolitis (NEC) mortality. This points to the safety and efficacy of probiotics in high-risk populations.[174]
Women who took probiotics during pregnancy had fewer incidences of:[175]
- Gestational diabetes
- Pre-eclampsia (high blood pressure during pregnancy)
- Excessive weight gain
- Vaginal bacteria infections
More studies show that probiotics:
- Appear safe for infants and even preterm infants[174, 176, 177]
- Protect infants against intestinal fungus (candida) overgrowth[178]
- Reduce the risk of ear and respiratory infection in babies[179]
- Reduce colic
- Reduced symptoms of allergic rhinitis[149]
- Are beneficial as part of a treatment program for newborns with jaundice[180]
- Significantly improve abdominal pain for children with IBS[181]
Otitis Media
- No Evidence from a Systematic Review for the Use of Probiotics to Prevent Otitis Media[182]
So far, we’ve covered why imbalances in intestinal bacteria are so common and how these imbalances can lead to excessive inflammation. We discussed that probiotic supplementation can improve the health of your intestinal microbiota and by doing so can improve a litany of symptoms.
We have also clarified that almost every probiotic formula used in research studies is one of three types or categories. This greatly simplifies the process of finding the best probiotics for your gut and leads to Probiotic Triple Therapy we will now detail.
Probiotic Triple Therapy
In order to use probiotics effectively it is crucial that you understand the power of simplicity. The importance of simplicity has been emphasized throughout history.
“Truth is found in simplicity, not in the multiplicity and confusion of things.”
Isaac Newton
“The evolution of knowledge is toward simplicity, not complexity.”
L. Ron Hubbard
“Knowledge is a process of piling up facts; wisdom lies in their simplification.”
Martin H. Fischer
“Complexity is impressive, but simplicity is genius.” –
Lance Wallnau
As quoted above, when knowledge of probiotics increases to the point of “wisdom” or “genius”, a simplification in their application appears.
What you need to do – easy as 1, 2, 3
-
Probiotics Easy Protocol Try a quality formula probiotic from category 1, category 2 and category 3 – take all three together.
- Monitor your symptoms for 3-4 weeks.
If you’re improving, stay on the Probiotic Triple Therapy protocol until your improvements have plateaued. - Once you’ve seen your maximum improvement (you’ve plateaued), stay here for about a month to allow your system to calibrate to these new improvements.
Then reduce your dose and find the minimal effective dose. Stay on the minimal effective dose.
Research supports this approach to taking probiotics. When mixtures of several probiotics were compared with single strains of probiotics in the treatment of IBS, the systematic reviews and meta-analyses indicated that the multi-strain probiotics were more effective than single-strain probiotics.[183, 184]
Multistrain probiotics were also found to perform better in a meta-analysis of studies using probiotics to treat constipation.[96]
A meta-analysis found that multiple strains of probiotics were more effective than single strains in reducing depressive symptoms.[107]
Dosing Your Probiotics
Each probiotic has a dose range. Anywhere in the range is fine, more isn’t better. Some like to start at the lower dose, wait a few days and then try the higher dose. Others like to go right to the high dose. Do whatever appeals to you.
| Name | Dose | Times/Day | w/Food |
| Lacto-Bifido Probiotic Blend | 1/4 tsp. OR 4 pills | 1-2 | N |
| Saccharomyces Boulardii Probiotic | 2-4 pills | 1-2 | N |
| Soil-Based Probiotic | 1-2 pills | 1-2 | Y |
Why a dose range?
These dose ranges cover the ranges that have been used in research studies. This is good news. It means you have some leeway in your dose. When you look at the ranges listed in the studies, see table below, you see a common range emerges. Thus, our simple range which provides you a summary of what has been used in the research.
| Condition | Dosing Range | References |
| Irritable Bowel Syndrome – IBS | 10 million – 1,000 billion CFU/day | [82, 83, 84] |
| Intestinal Imbalances: | ||
| SIBO | 100 million – 10 billion CFU/day | [48, 87, 88] |
| Leaky Gut | 10 – 100 billion CFU/day | [23, 24] |
| Fungus | 5 billion CFU/day | [90] |
| H. Pylori | 20 million – 1,800 billion CF/day | [185] |
| Infection | 10 – 15 billion CFU/day | [49, 55] |
| Inflammatory Bowel Disease – IBD | 10 million – 100 billion CFU/day | [91, 92, 93] |
| Mood, Depression & Anxiety | 10 million – 100 billion CFU/day | [47, 106, 108, 114] |
| Brain Fog | 1 – 1,000 billion CFU/day | [117, 119, 120] |
| Sleep | 1 – 100 billion CFU/day | [121, 122, 123, 124] |
| Autoimmunity | 100 million – 10 billion CFU/day | [128, 129, 130, 131] |
| Metabolism | 10 million – 100 billion CFU/day | [186, 187] |
| Female Hormones | 1 – 1,000 billion CFU/day | ** |
| Thyroid Function | 1 – 100 billion CFU/day | [58] |
| Blood Pressure & Cholesterol | 1 million – 1,000 billion CFU/day | [153, 154, 155, 156, 157, 158] |
You have options. You can use any quality probiotic that fits the profile of what I’ve described above. I recommend the formulas I’ve created here. These are what I use in my clinic and myself, so I can vouch for them. I went through a period of not feeling well, I know it’s not fun. Fatigue and brain fog, as I suffered from, made life hard. This is why I’ve tried to make using Probiotic Triple Therapy as easy for you as I can.
Our store offers free shipping and stands behind our probiotics with a satisfaction guarantee. If this is helpful, great. If not, feel free to shop around and use what you feel most comfortable with. We will detail what quality assurance practices you should look for in a probiotic a little later.
It doesn’t really matter if probiotics are taken with or without food. Do whatever is easiest for you. Many people like to take them in the morning with some water. And then again in the evening.
You will hear claims that a given type should or should not be taken with food, but there is no conclusive evidence to support this, only speculation. I tell my patients to do whatever they will be most consistent with.
Troubleshooting
Some people are very sensitive to dietary supplements. If this is you, simply start the probiotics one at a time, roughly every few days. If any probiotic causes a negative reaction lasting longer than five to seven days, stop. This means whatever one you are using is not a good fit for your gut.

At the end of the day, you want results. You want a probiotic protocol to reduce or eliminate whatever symptoms you are suffering from. As a doctor, I want this for you also, but I understand that we need to fix the underlying cause of your symptoms. So, instead of using a probiotic that is marketed for your symptom, we go a level deeper and use Probiotic Triple Therapy to ensure we support a balanced healthy gut environment.
This thorough probiotic therapy fixes the underlying cause of your symptoms and thus your symptoms resolve. The symptoms that improve after balancing your gut could be anything from digestive symptoms all the way through mood or metabolism. This probiotic protocol is not a cure all, but gut health is clearly a foundational aspect of wellbeing.
Important reminder, probiotics are not a get out of jail free card for an unhealthy diet and lifestyle. These both must be in place to see optimal response to any probiotic regime.
The difference between success and failure with probiotics often comes down to either:
- Establishing balance in your gut ecosystem
- Failing to establish balance in your gut ecosystem
The key difference here is that many people don’t seem to achieve this balance with just one probiotic. Some lucky people do, but for many, one probiotic won’t suffice.
“But it’s easier if I use one probiotic.”
It might seem easier, but it is more difficult to obtain the results you are looking for. Just as it is much harder to balance on a one-legged stool, it’s hard to rebalance your gut environment with one probiotic support.
With Probiotic Triple Therapy, the three probiotics all act to support different niches of your gut environment. Together, these three supports achieve balance. Most people require all three to feel best. In fact, in my clinical practice it is somewhat common for someone to come into my office claiming “I’ve tried probiotics and they don’t work for me.” Just like Phyllis, who had been suffering with digestive symptoms for three years. She tried diets and numerous probiotics, nothing worked. Not until the simple, yet effective, Probiotic Triple Therapy.
Here is another way of thinking about this.
What is the likelihood you will randomly stumble across and try a random probiotic in a few months. And then in another few months, again try another probiotic when a marketer finds the right buzz word to pique your curiosity? Get off the probiotic merry-go-round. Do this the right way, do it once, and be done with it.
We just quickly mentioned Phyllis, who provides us a clear example of the power of Probiotic Triple Therapy.
Here is the summary of her case:
- Experienced digestive issues for 3 years
- Was previously diagnosed with SIBO
- Did the Paleo low FODMAP diet for 2 yrs
- Tried random probiotics – had a negative reaction
- Nothing was working….
After roughly 1 month she experienced:
- Increased energy
- Improved motility (or bowel regularity)
- Improved overall gut health (as she described it)
Here is a key takeaway, if you get the probiotics right you could finally achieve balance in your gut. Phyllis had tried probiotics, but like trying to balance on a one-legged stool, her gut was always tipping into imbalance. When she finally supported all three ‘legs’ of her gut ecosystems, she improved markedly. Again, Probiotic Triple Therapy is not a panacea, but it is effective for many.
1st – Take stock of your symptoms
They might be fatigue and depression, or bloating, or joint pain, or constipation, or insomnia, or unstable dose of thyroid medication. Whatever they are, take stock of how often and how severe your symptoms are.
2nd – Reevaluate these symptoms after 3-4 weeks of probiotic therapy
Are you improving? If so, keep on the protocol. You are not looking for complete resolution, per se. If so, that is great. But don’t expect everything to be fixed completely at the 3-4 week mark. You are looking for a clear trend of improvement. If so, great, we are on the right track. Keep going.
3rd – Look for when you hit your peak improvement
Once you peak or plateau, great. This is another milestone. Keep this constant for another four weeks, so your body can integrate and you can lock in this new balance.
After four weeks…
Finally – Try to gradually find the minimal effective dose
Technically, you don’t have to do this but I find less is more with supplements. I like people to cut their dose in half, then reevaluate after 3-4 weeks. If this goes well, try coming off completely.
These are just rough guidelines, this is not that precise so don’t stress yourself out. This is a simple process of gradually trying to wean off. If at some point your symptoms return, it means you should stay on the probiotics.
You can try weaning again in a few months. Simple. Don’t overcomplicate this.
Here are a few scenarios of what dose weaning might look like.
- You half your dose, then a few weeks later you say “Hmm, I’m experiencing significantly more X”.
- You weaned too early. Go back to your initial dose.
- You half your dose, your symptoms don’t change.
- Great. Wait 3-4 weeks and try coming off completely.
- You come off completely and… repeat the two bullets above.
Probiotics can safely be used in the long term, so if you consistently notice you feel better on them that is OK.
I was doing great on my maintenance dose until….
Life happens and this can derail gut balance. Things like travel, stress or a significant period of poor self-care might lead to a regression. If this happens, it’s OK. It happens. No one is bulletproof. Simply return to the full Probiotic Triple Therapy protocol, and then later you can again wean your dose.
You may have heard claims like:
Only X probiotic has been proven effective for Y symptom….
In some cases, this is a well-intentioned claim by those who are trying to stay congruent with the research. In other cases, this is just marketing i.e. cherry-picking studies to sell you something. In either case, the message is generally incorrect. Of course, there is no need to explain why cherry-picking studies is incorrect. But, why are those who are attempting to stay true to the research incorrect?
Well, these types of claims that only X probiotic has been shown effective for Y condition are reflective of a limited knowledge of probiotic research. Said simply, if you know of one study showing a probiotic can improve constipation, you would state ‘only X probiotic has been shown effective for constipation’. The whole time being unaware that other studies have found different probiotics can also improve constipation.
Here’s the Proof
- Multiple studies have found probiotics can improve mood. As we discussed earlier, these studies used different probiotics.[106, 108, 114] These probiotics were all different iterations of category 1.
- Different categories of probiotics have been shown to improve IBS, including different probiotic formulas from category 1,[84, 188] category 2,[189] and 3.[62]
- Three different probiotics have been found to improve constipation.[184, 190, 191] In fact, one study even directly compared two different formulas in a placebo-controlled fashion and found either probiotic formula worked.[192] These studies mostly used category 1 or category 2 probiotics.
- Various types of probiotics have been found helpful for inflammatory bowel disease. Mainly category 1 and 2[193] but also a growing number of studies on category 3.[70, 194]
- At least 2 different categories have been shown effective against SIBO.[87, 195, 196]
- Urinary tract infections have been reduced using category 1 probiotics. The formulas differ from study to study.[197]
So, it’s clear that probiotics are not condition-specific and that different probiotics can work for the same symptoms or condition. This is why I find it frustrating seeing marketers try to sell you the special probiotic for a given symptom. It is misleading. This is also why we can simplify the process via Probiotic Triple Therapy. Remember this quote from earlier
“The evolution of knowledge is toward simplicity, not complexity.”
A non-evolved perspective on probiotics would have you believe that you need a different probiotic for every different symptom or condition. One for SIBO, one for constipation, another for depression, and so on. However, as our knowledge evolves we see many different types of probiotics could help the same condition. Evolve further and we see that it is more important that we use the 3-category approach to help support balance in your gut ecosystem. This addressed the root cause of many symptoms and conditions.
We have to think critically
There was a point in time where I was planning to use a special probiotic for my constipated patients. This was after the first, and only study of its kind, was published showing probiotics could improve constipation. Then, something interesting happened. Six months later, a different probiotic formula was shown to improve constipation. Then, soon after, another study showing another different probiotic also improved constipation.
I watched this same thing happen with probiotics and mood, probiotics and SIBO, etc…. Eventually I came to understand it wasn’t that specific, nor that complicated. Unfortunately, not every ‘health expert’ seems to be following the literature and are still making antiquated claims like “you need a certain probiotic for constipation. The only proven probiotic…” Or, even worse, they are unaware of any of the studies showing probiotics can improve constipation so they hide behind platitudinous comments like ‘we need more research’. Agreed, we always need more research, but if you know your stuff you can at least provide a cautious recommendation.
Probiotics are not drugs
So, probiotics are not like drugs. They do not have a limited mechanism of action to suppress a certain pathway that is involved with a given symptom. Probiotics are not like, for example, acid blocking medications which treat acid reflux. But rather, probiotics help to support a healthy gut environment thus treating the underlying causes. Befittingly, probiotics may also help with reflux.[198] However, probiotics do not cause the long term side effects that acid suppressing medications do.
Yes, we want to be scientific but don’t fall into the trap that someone who cites science has a mastery of a body of science. Anyone can do a quick search and find a reference. It takes years and years of study to have a mastery of a body of research. This is the wisdom I’m trying to impart here.
“Knowledge is a process of piling up facts; wisdom lies in their simplification.”
Probiotic Criticisms
There are two viable criticisms of probiotics:
- We need more and better quality data
- The type of probiotics used in the research has varied, thus making it difficult to create any clinical recommendations
We need more and better quality data
This is true. We could have better data, but there is some nuance here we should fill in. Here is a helpful analogy. If you had a porsche you could still have a better car, say a ferrari. Porsches start at $60,000 while Ferraris start at $250,000. Either car is great, but the ferrari is better. This parallels probiotic research.
We have numerous clinical trials. We even have the gold-standard summary of several clinical trials, the coveted meta-analysis. So, probiotics are a porsche. However, we could have even better, ferrari-like, data in the sense that the clinical trials could have a larger number of participants.
You see, the more participants in a given clinical trial, the more accurate the data. Think of it this way, if surveyed 70 people ate at a restaurant this would give you an idea of how good it was. But if instead you had a survey of 700 people who ate at this restaurant, you would have an even better idea of how good it was.
Currently, the clinical trials in probiotics are smaller than typical drug studies (more like 70 people rather than 700). The drug studies often have hundreds, or even thousands, of subjects in one large clinical trial. Unfortunately, the profit to be made from probiotics is not as much as the profits to be made from drugs, so the funding for these studies is lacking. Drug studies do often have ‘better’ data, like the drug Rifaximin, which is an antibiotic which can be quite helpful for IBS.
So, while yes we could have better data, ie the ferrari equivalent of research, I would much rather someone use the probiotic porsche before using a ferrari drug/antibiotic. That said, they both have their place. To be clear, certain antibiotics can be helpful. Antibiotics are often vilified as exclusively harmful, which they are not. We should be open minded to either therapy.
The types of probiotics used in the research has varied…
This is another viable criticism, but is also a remnant of a research model that is more reductionist and drug-centered. We addressed this earlier when we discussed that probiotics do not act like drugs. Drugs having a narrow mechanism of action, but probiotics more broadly support your gut.
We also detailed the research supporting this claim in how different types of probiotics have shown benefit for the same condition. We want to be evidenced-based and use science. Yes. However, we also do not want to be evidence limited. Meaning, we have to be able to think critically and weigh the pros and cons.
In this case, the pro/con balance clearly favors, at the very least, a trial on probiotics. Then, considering other more invasive therapies.
Here is an example. There are more studies, larger studies, using antidepressant drugs for depression and anxiety. These drugs also carry side effects, as WebMD lists[199] such as:
- nausea
- increased appetite and weight gain
- loss of sexual desire and other sexual problems, such as erectile dysfunction and decreased orgasm
- fatigue and drowsiness
- insomnia
- dry mouth
- blurred vision
- constipation
Probiotics on the other hand, while improving your mood, may also have side-benefits, including reduced inflammation, bloating and improved bowel regularity.
While the evidence could be better, we certainly have enough evidence to support a reasonable trial on probiotics. We should trial probiotics while also being responsible and not ignoring standard medical care if it is indicated. Probiotics are not a panacea.
Quality assurance practices do matter, let’s start with the two most common problems with cheap probiotics.
The two most common problems with probiotics are:
- not meeting label claims
- containing potentially harmful organisms
Here are the best practices you should look for in a probiotic. If a company follows these quality assurance practices a probiotic will meet its label claims and not contain potentially harmful organisms. The Probiotic Triple Therapy approach I’ve formulated follows all of these guidelines.
Genetic identification
To ensure the strain of probiotic meets the label claim, thus protecting you from using frankenstein probiotics or harmful organisms. Harmful organisms are one of the most common problems with probiotics, as we will detail more in a moment.
Free of all major allergens
Probiotics should be grown on media which are free of the common allergens: wheat, gluten, milk, casein, eggs, fish, shellfish, tree nuts, peanuts and soybeans. Quality probiotics will also be free of artificial colors, flavors, or preservatives.
Validated potency
Probiotics should always meet the claims of their lab upon testing. Certain probiotics should be stored by the manufacturer and shipped in refrigerated conditions to retain the potency list on the label claims.
Current Good Manufacturing Practices (CGMP)
GMP is defined as:
A set of best practices for dietary supplement manufacturing in the United States.
This includes utilizing a state-of-the-art facility where temperature and air quality are tightly controlled. This produced a consistent quality and purity of product.
Independent laboratory analysis
All probiotic raw materials and final products undergo independent laboratory analysis ensuring probiotic quality and fulfillment of GMP requirements. This ensures the probiotic meets its label claims.
How Important is Quality Assurance
Some companies hide behind ‘quality assurance’ as a ploy to jack up their prices. You don’t need to purchase the most expensive probiotic. But, you should be wary of a probiotic that is substantially cheaper than the rest. This usually indicates corners have been cut in the above quality assurance measures.
This does matter and is evidenced by cautions published in the research literature.
Examples of why quality matters
The Journal Biotechnology & Biotechnological Equipment found[200]
- None of the 26 commercial probiotics assessed fully supported label claims, and some of them contained unacceptable microorganisms.
- Two common problems were a low concentration of viable cells (ie you’re getting ripped off) and the presence of undesired (potentially harmful) organisms.
The Journal of Clinical Gastroenterology and Hepatology has concluded[201]
- Regulation of probiotics is inadequate to protect consumers and doctors.
The journal PLOS One found[202]
- Only half of the probiotics they examined had the specific strain listed on the label, which varied considerably by store.
LabDoor found
- 43% of the probiotics assessed contained less than half the amount of probiotic listed on their labels
Bioinformatics and Drug Discovery concluded[203]
- Regulations of probiotics are loose, so the safety and effectiveness of most probiotics gets to be decided by the manufacturer.
The bottom line
No, not by the consumer. A storage temperature that is less than 77 °F is likely fine.
During short term storage (a few months in the hands of the consumer), refrigeration is not required. One caveat, if your residence is hot (100 degrees Fahrenheit) then you should keep your probiotics in the fridge.
During longer term storage (as in at the manufacturing facility), yes probiotics should be refrigerated.
You can store your probiotics in the fridge if you’d like, just understand it’s not required – this is welcomed news by most of my patients as it makes life easier (especially when traveling).
Ambient temp is OK (less than 77° F)
The journal Microorganisms[204] in 2019 essentially states it’s OK to store at room temperature.
“probiotics may be incorporated in dietary supplements and other “dry” food matrices which are expected to have up to 24 months of stability at ambient temperature and humidity.”
Specifically, less than 77 °F and you’re OK.
This is via the International Probiotics Association 2019 guidelines recommend storing category 1 and 2 probiotics at less than 77 °F.
Hot temps are bad (over 104 F)
The Journal of Applied Microbiology[205] found storage at a temperature of 104 Fahrenheit was damaging to probiotics.
We provide freezer bags when shipping certain probiotics, but this isn’t really necessary.
Some evidence has even found that probiotics that were killed by heat still had positive effects!
Four different studies used heat-killed probiotics and found them beneficial for improving IBS symptoms, treating skin allergy, enhancing the immune system and reducing colds.[170, 206, 207, 208] Another very surprising study found that heat-killed Lactobacillus was more effective than living Lactobacillus in treating diarrhea.[209]
The National Institute of Health[210] states that probiotics are generally safe, even for premature infants.
“Given the large quantities of probiotics consumed around the world, the numbers of opportunistic infections that result from currently marketed probiotics are negligible. For example, probiotics have been administered to thousands of newborn infants, including some who were premature, without a single case of sepsis.”
When not to use a probiotic
Those who are critically ill.
The journal Expert Opinions on Drug Safety recommends the following[211]
“Critically ill patients in intensive care units, critically sick infants, postoperative and hospitalized patients and patients with immune-compromised complexity were the most at-risk populations.”
“While the overwhelming existing evidence suggests that probiotics are safe, complete consideration of risk-benefit ratio before prescribing is recommended.”
However, when it comes to immune-compromised individuals, recent research suggests that probiotics may be safe and beneficial.[212] An analysis of 57 clinical studies indicates that probiotic administration in immunocompromised adults is safe with regard to the current evaluated probiotic strains, dosage and duration. There were no major safety concerns in the study, and overall, adverse events occurred less frequently in immunocompromised subjects receiving probiotics compared to the control group.
How good are the data showing probiotics are safe? Well an analysis of 57 clinical trials is a great start. However, there have been criticisms that the quality of these trials could be better so this should be kept in mind.
The first thing we should ask here is, are probiotics safe for infants? Answer: yes and we’ll elaborate below. Second question, do probiotics provide benefit to infants? Answer, again yes. That said, make sure to speak with your pediatrician before using a probiotic with your infant or child.
Probiotics are safe for healthy infants according to a systematic research review[173] based on studies using six different probiotics (all Category 1). None of the studies found any safety concerns or adverse effects. Researchers found some benefits from probiotic use, including:
- less colic and irritability,
- less diarrhea,
- fewer spitting episodes and
- fewer respiratory infections.
Different benefits are connected with different strains, which suggests that a multi-strain formula may be the best choice.
Another systematic review with meta-analysis looked at 44 studies involving premature babies. Probiotics helped to prevent serious GI illnesses that are sometimes fatal for very low birth weight babies.[213]
A very interesting review looked at the impact of prenatal and postnatal probiotic use.[175] Researchers found several benefits for both mom and baby. Women who took probiotics during pregnancy had fewer incidences of:
- Gestational diabetes
- Pre-eclampsia (high blood pressure during pregnancy)
- Excessive weight gain
- Vaginal bacteria infections
Another review that included data from 4368 pregnant women[214] showed that prenatal probiotic use resulted in lower death rates and lower rates of necrotizing enterocolitis (a life-threatening intestinal infection) among babies. The moms who took probiotics in this study also had longer pregnancies.
Both studies noted that the babies born to these moms had much lower rates of eczema at birth and later in childhood.
Probiotic supplementation after birth reduced symptoms of colic and decreased the risk of life-threatening GI conditions for infants.
More studies show that probiotics:
- Appear safe for infants and even preterm infants.[176, 177]
- Protect infants against intestinal fungus (candida) overgrowth.[178]
- Reduce the risk of ear and respiratory infection in babies.[179]
That being said probiotics are not always protective. If a child is very ill, probiotics may not be helpful or even detrimental. This was shown in a study where pediatric intensive care babies had slightly more infections when given a probiotic.[215]
What Type and Dose of Probiotic is Best for Infants?
Most of the infant studies used an infant formula fortified with category 1 probiotics. The exact strains varied from study to study. Dosages varied between studies as well, but 10 billion CFU per day appears a good general starting point.[216] Talk to your pediatrician before choosing a probiotic for your child.
| Probiotic Species | Dosage | Reference | Species Used In Our Blend (Lacto-Bifido Blend) |
| L. paracasei, L. plantarum, L. acidophilus, L. bulgaricus, B. longum, B. breve, B. infantis, S. thermophilus | 5 billion CFU/day | [217] | L. paracasei, L. plantarum, L. acidophilus, L. bulgaricus, B. longum, B. breve, (B. infantis not in blend), S. thermophilus |
| L. reuteri | 100 million CFU/day | [218] | (not in blend) |
| B. breve, Propionibacterium freudenreichii, and L. rhamnosus | 12 billion CFU/day | [219] | B. breve L. rhamnosus |
| L. rhamnosus | 1 billion CFU/day | [220] | L. rhamnosus |
| B. bifidum, B. lactis, and Lactococcus lactis | 3 billion CFU/day | [221] | B. bifidum, B. lactis |
| B. lactis and L. rhamnosus | 2 billion CFU/day | [222] | B. lactis and L. rhamnosus |
| L. rhamnosus | 10 billion CFU/day | [223] | L. rhamnosus |
| L. paracasei and B. lactis | 20 billion CFU/day | [224] | L. paracasei and B. lactis |
Probiotics are Not a Substitute for Medical Advice
Yes, probiotics can improve a number of symptoms and conditions. No, they are not a cure-all and are no substitute for necessary medical care. Speak with your doctor regarding how probiotics could be integrated into your current treatment.
Also, remember that not all doctors are knowledgeable about probiotics. If your doctor isn’t aware of the research presented in this article, then consider obtaining a second opinion.
Probiotics as Part of a Larger Health Plan
As helpful as probiotics can be, they may not be enough alone. You may require other, synergistic, supports to fully heal and balance your gut. This could include:
- Finding the ideal diet for your gut
- Determining if you require supplemental enzymes
- Use of herbal antimicrobials agents
- Special, gut healing, meal replacements shakes aka elemental diets
- Select nutrients to help rebuild the lining of the gut
- Prebiotic or fiber supplementation
If you feel you require more support than probiotics, please see Healthy Gut, Healthy You to determine what your personalized gut-healing plan should look like.
The health of your gut has far reaching effects. If you have gas, bloating, constipation, diarrhea, abdominal pain and/or reflux – you could improve the health of your gut. However, fatigue, depression, joint pain, skin issues or thyroid challenges could also be emanating from your gut.
Probiotics are a safe and effective way to encourage healing in your gut and balancing of your gut microbiota, thus addressing the root cause of many of these symptoms and conditions. Using a quality probiotic protocol, involving all three of our three categories, can lead to substantial improvements. Even if you have tried a probiotic in the past, it is well worth using Probiotic Triple Therapy as you may experience the improvements you’ve been hoping for.