Patient Summary:
- Overview Context:
- Mary is a 52 year old female seeking guidance for ongoing GI symptoms. She has struggled with weight and has tried “several different health programs” and diets. Her goal is to feel better overall, and she would like to find a sustainable plan to mitigate her symptoms and help optimize her weight.
Symptoms and Concerns
- Chief Complaints:
- Stomach pain
- Burping
- Acid reflux
- Throat constriction sensation
- Weight
- Other Symptoms:
- Hot flashes
- Fatigue
- Shakiness
- Snoring frequently
- Waking gasping for air
- Onset, Timeline and History:
- Constipation and mouth breathing during sleep since childhood.
- 2017-2018: Noticed increase in seasonal allergy symptoms.
- 2019: Worsening of reflux, gas, and stomach pain.
- 2020: Worsening of burping/belching; sensation of throat closure started.
- 2021: COVID followed by all worsening of all symptoms; began experiencing more persistent constipation.
Past Medical History
- Prior Diagnoses:
- Obesity (BMI 41)
- GERD
- IBS
- Medications:
- N/A
Prior Testing and Treatment History
- Prior Testing Summary:
- 2019 Endoscopy – Sliding hiatal hernia, esophagitis, and gastritis
- 2019 SIBO Breath Test – Hydrogen positive
- Previous Diets:
- Helpful
- Gluten-free
- Dairy-free
- Paleo
- Low histamine diet
- Low carbohydrate diet
- Helpful
- Previous Treatments:
- Helpful
- Immunoglobulins
- Antihistamines
- Acupuncture
- Coffee enemas
- Non Responsive
- PRObiotics (Triple Therapy Probiotics)
- Antibiotics (Xifaxan)
- Digestive Enzymes
- Hydrochloric acid (Betaine HCl)
- Magnesium
- Reactive
- Herbal Antimicrobials
- PREbiotics
- Bitters
- Colostrum
- Helpful
Initial Impression
- Clinical Commentary:
- This patient likely has dysbiosis based on her upper GI symptoms. She does have a past history of SIBO in 2019, which may still be present given her current symptoms, especially reflux and belching.
- She has tried an extensive list of nutrition plans and supplements. She even found many of them to be helpful, however she found challenges in sticking with them.
- She mentioned that she feels defeated, and that her case must be “extremely complex” due to her lack of response thus far. Patients who say “I am a complex case” should be gently called out on this. This is a negative mindset that can impact their progress and become a self-fulfilling prophecy. We like to reframe this as “we often find patients who felt their case was complex were simply not provided with the right treatments. Once the right treatments are given, our patients who have been sick for years often start feeling better in months.”
- Recommended Testing
- At-Home Sleep Study
- Standard Panel: CMP, CBC w diff, iron panel, ferritin, Vit D
- Thyroid Panel: TSH, fT4, fT3, TPO
- Metabolic: fasting insulin, HgA1c, lipid panel
- Cardiovascular: lp(a), apoB
- Initial Treatment Recommendations
- Diet:
- Paleo Low FODMAP Diet
- 80% compliance recommended
- Intermittent fasting for 14-18 hours, once or twice weekly
- Health coach check-ins recommended for implementation support.
- Paleo Low FODMAP Diet
- Lifestyle:
- Daily meditation
- Gentle walking for 30 minutes 3-4x/week, ideally in nature with a friend
- Improve sleep hygiene
- Treatment:
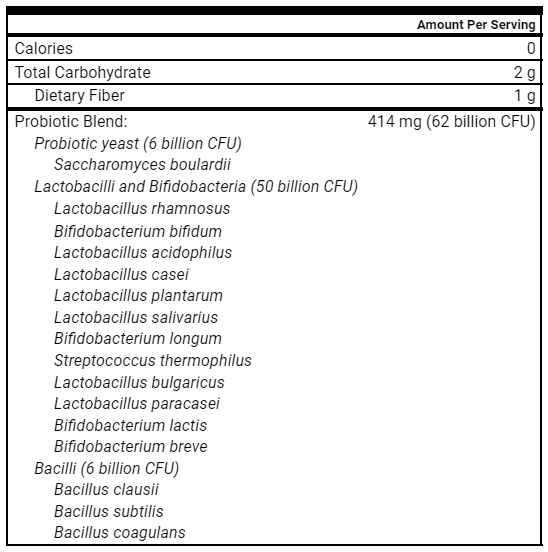
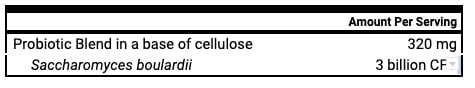
- S. boulardii, soil-based probiotics, lacto-bifido probiotic blend
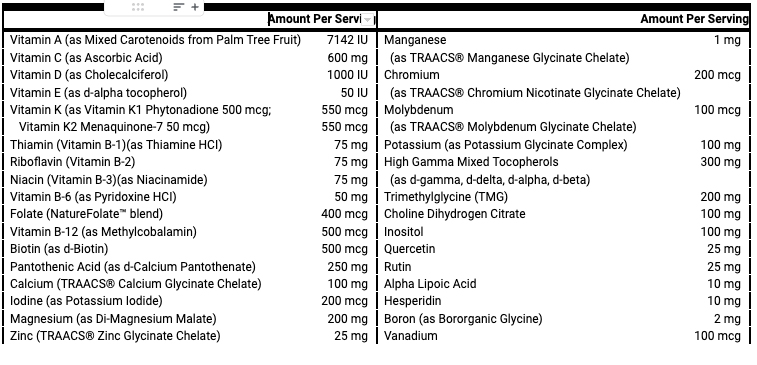
- Multivitamin/mineral
- High potency fish oil
- S. boulardii, soil-based probiotics, lacto-bifido probiotic blend
- Follow-up: 5-7 weeks
- Diet:
- Clinician Summary
- Home sleep study was recommended because of classic sleep apnea symptoms of snoring, waking gasping at night, and fatigue.
- We’re recommending the Paleo low FODMAP diet because she hasn’t tried it yet and it is very clinically useful for improving symptoms associated with dysbiosis and SIBO. We are recommending she follow it 80%, as she expressed difficulty with sticking with different diets. This allows the patient to let go of perfectionism and be more consistent.
- Despite reporting “no response” to triple probiotics, we find that patients often try the right interventions, but just do them either for not long enough or they’re missing other foundational interventions, including proper diet, mindset and stress management. We believe that adding in triple therapy probiotics alongside the other therapies will lead to better success than just triple probiotics alone.
- Subjective Assessment
- Overall 50% improvement since initial visit
- Lost 10 pounds
- Still experiencing mild reflux, throat pain, and nausea
- Current Symptoms:
- Improved:
- Stomach pain
- Burping
- Throat constriction sensation
- Acid reflux
- Fatigue
- Shakiness
- Weight
- Same
- NA
- Worse:
- NA
- Treatment Response:
- Lacto/bifido and soil based
- Tolerated well
- S. Boulardii
- Reports increased heart rate/palpitations
- Lacto/bifido and soil based
- Improved:
- Lab Results
- Sleep Study: Moderate obstructive sleep apnea
- Cholesterol, Total 204 High (100-199 mg/dL)
- LDL-C 130 High (0-99 mg/dL)
- Apolipoprotein B 109 High (<90 mg/dl)
- Vitamin D 9.2 Low (30.0-100.0 ng/mL)
- Lab Interpretation and Diagnosis
- Moderate hyperlipidemia present with elevations in ApoB. Lack of personal history of diabetes or family history of early cardiac death indicate close follow up and monitoring for improvement and further lifestyle changes.
- Most notable lab finding is moderate obstructive sleep apnea.
- Impression:
- Overall, she is moving in a great direction, feeling 50% better after her initial set of recommendations. This tells us we are on the right track with addressing dysbiosis. She is still experiencing some lingering upper GI symptoms, including reflux, throat pain, and mild nausea.
- Due to persistent GI symptoms, I will recommend a trial of an elemental diet reset and GI Support nutrients to further reduce upper GI symptoms. Recommending vitamin D due to deficiency.
- Updated Treatment Recommendations
- New Treatment:
- Continue lacto/bifido and soil based probiotics
- Elemental diet reset for 3-4 days, then resume Paleo low FODMAP
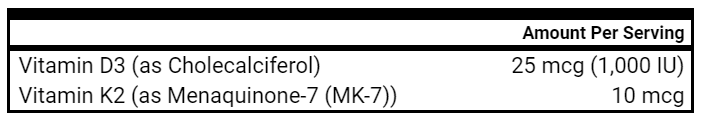
- Vitamin D
- GI Support Nutrients
- (Optional) Trial S. Boulardii again after above steps to see if tolerated better
- Referral:
- Primary care doctor for treatment of moderate obstructive sleep apnea diagnosis
- Follow-up: 5-7 weeks
- New Treatment:
- Highlighted Clinical Rules
- Diet and lifestyle based approaches should start with the least invasive or restrictive treatments first.
- Many therapies have more support to be used empirically as compared to being guided by lab results (e.g. probiotics for GI support).
- Clinician Commentary
- Over a 4 month time frame she has been able to implement exercise, follow a nutrition plan long term with 80% compliance, and she feels empowered again.
- This patient experienced significant improvements in GI symptoms with empirical treatment without the use of lab testing. We did NOT need to do any stool testing or SIBO breath testing in order to help her to improve. We used her response to treatment to guide our clinical thinking. Her positive response to GI care (probiotics, Paleo low FODMAP diet) helped inform us she is likely experiencing dysbiosis/SIBO. Once we see how she does on elemental dieting and GI support nutrients, we may pivot to herbal antimicrobials. However, this will all depend on how she is doing symptomatically and not based on lab testing. If she is doing great, then we will likely begin reintroducing FODMAP foods and start weaning her off supplements to create a more sustainable plan.
- Although we typically advocate for triple probiotic therapy when tolerated, this patient was able to see significant improvement by just taking lacto/bifido and soil-based probiotics. This highlights that a treatment or diet plan doesn’t have to be executed perfectly to see positive results.
- Overview Context:
- Sarah is a 40 year old female and mother of two. She is looking to improve her overall health and find the root cause of her GI symptoms and hypertension.
Symptoms and Concerns
- Chief Complaints:
- Gas / bloating
- Fatigue
- Frequent wakings at night
- Overweight (BMI 28)
- Other Symptoms:
- Frequent urination
- Hypertension
- Onset, Timeline and History:
- Weight increased after having her first child 10 years ago; remains unchanged with exercise.
- Wakes frequently throughout the night, does not feel rested and lacks energy even with a full night’s sleep.
- No significant diet history, yet feels carbohydrate intake is excessive and finds it difficult to avoid due to family food choices and cultural upbringing.
Past Medical History
- Prior Diagnoses:
- Gestational diabetes – 2012
- Hypertension – 2016
- Traveler’s diarrhea – 2017
- Gallstones – 2021
- Medications:
- Beta Blocker (hypertension)
- Prior Surgical History
- C-section – 2011
- Gallbladder removal – 2022
Prior Testing and Treatment History
- Prior Testing Summary:
- Sleep study (results pending)
- Previous Diets:
- Helpful
- Dairy-free
- Reduced gas/bloating
- No change
- Gluten-free
- Low carb (Atkins)
- Dairy-free
- Helpful
- Previous Treatments:
- Helpful:
- Soil-based probiotic
- Prebiotic
- Fiber
- Helpful:
Initial Impression
- Clinical Commentary:
- Are her gas and bloating a result of poor diet and dysbiosis? Or do we need to consider abdominal adhesions due to her history of C-section or recommend bile support due to her cholecystectomy?
- As gestational diabetes increases the risk of insulin resistance and hyperglycemia later in life, it seems as though routine screening based on her comorbidities of hypertension and elevated BMI would be indicated.
- The positive response to pre/probiotics and fiber gives us a glimpse of a direction that may provide more benefit for GI symptom management.
- Recommended Testing
- Standard Panel: CMP, CBC w diff, iron panel, ferritin, Vit D
- Thyroid Panel: TSH, fT4, fT3, TPO
- Metabolic: Fasting insulin, HgA1c, lipid panel
- Cardiovascular: lp(a), apoB
- Initial Treatment Recommendations
- Diet:
- Paleo diet
- Intermittent fasting for 14-18 hours, once or twice weekly
- Health coach check-ins recommended for implementation support
- Lifestyle:
- Daily meditation
- Resistance training 3-4 times weekly
- Blue light avoidance 1 hour before bed
- Treatment:
- S. boulardii, soil-based probiotics, lacto-bifido probiotic blend
- Vitamin D/K
- Multivitamin/mineral
- High potency fish oil
- Follow-up: 7-8 weeks
- Diet:
- Clinician Summary
- Rather than going right to bile supports or investigating abdominal adhesions as a cause of her bloating, we’re going to start with more foundational interventions, including diet, exercise, and probiotics.
- In this case, ruling out type 2 diabetes, hypothyroidism, anemia, vitamin D deficiency, and cholesterol elevations seemed to be an important place to start due to lack of previous metabolic testing with her known comorbidities.
- Every time testing is ordered, a reflection on how the test results will change potential treatments is crucial. If the testing results will not affect the initial treatment, then it can often be revisited as a future potential option. In this case, any of the abnormal findings listed above would initially and directly affect the treatment plan.
- Subjective Assessment
- Current Symptoms:
- Improved:
- Gas and bloating
- Frequent wakings at night
- Fatigue
- Same:
- Weight
- Hypertension
- Worse:
- None
- Improved:
- Treatment Response:
- Triple Probiotics
- Reduced gas and bloating
- Triple Probiotics
- Notes:
- The patient has been diagnosed with sleep apnea and prescribed CPAP therapy by a local physician. This has significantly improved her sleep quality and energy.
- She did not implement recommendations for diet, exercise, or health coaching.
- Current Symptoms:
- Lab Results
- Ferritin 194 High (15-150 ng/mL)
- LDL-C 107 High (0-99 mg/dL)
- ApoB 101 High (<90 mg/dL)
- Vitamin D, 25-Hydroxy 35.4 (30.0-100.0 ng/mL)
- HbA1c, Insulin, Thyroid Panel, CBC/CMP – within normal limits.
- Lab Interpretation and Diagnosis
- Elevated ferritin with normal iron and iron saturation is most likely secondary to inflammatory response due to BMI and body fat %. Other likely causes such as fatty liver (liver enzymes normal), acute infection (no symptoms), and excess alcohol intake were ruled out. Due to iron overload not being present, this marker will prompt watching and waiting. Overall, her lab work was helpful and allowed us to rule out severe or acute metabolic concerns.
- Her sleep apnea diagnosis and treatment was a wonderful step for overall health as she mentioned the extra energy and mental clarity left her feeling more empowered to make the other lifestyle changes we discussed.
- Since she saw significant improvement in bloating and gas yet still had some residual symptoms, the next step was to focus on the approach that was already helping by doubling the dose of probiotics.
- Impression:
- She had challenges implementing the nutrition and lifestyle changes given during the initial visit. More care could have been taken on the initial assessment in understanding her readiness to change.
- Despite offering to simplify recommendations to a more stepwise approach, she chose to move forward with the previous lifestyle and diet recommendations. She also elected to lean into health coaching support between appointments for implementation tips and accountability.
- Updated Treatment Recommendations
- New Treatment:
- Health coaching for support
- Double current dose of triple therapy probiotics
- Follow-up: 10 weeks
- New Treatment:
- Subjective Assessment
- 50% better overall since we first started working together.
- Clothes are fitting better even though no change on the scale.
- GI symptoms significantly improved.
- Still having difficulty implementing the nutrition plan fully.
- Current Symptoms:
- Improved:
- Gas/bloating
- Frequent wakings at night
- Fatigue
- Same:
- Hypertension
- Weight
- Improved:
-
- Treatment Response:
- Triple probiotics
- Improved digestion and less ‘stuffed’ sensation after meals. No more persistent GI symptoms.
- CPAP
- Rarely wakes at night; consistently sleeping about 7 hours per night
- Triple probiotics
- Notes:
- Increased activity by resuming pilates.
- Continues to struggle with a Paleo diet when making meals for herself and family.
- Treatment Response:
- Highlighted Clinical Rules
- Functional Medicine is foundationally a diet and lifestyle based approach and should start with the least invasive treatments first such as diet, lifestyle, and gut health.
- Consider pushing further into therapies that have a clear positive signal as compared to adding new therapies (e.g. doubling dose of probiotics before adding antimicrobials).Address underlying gut dysbiosis before digestive secretions.
- Clinician Commentary
- Habit change is challenging and takes time. The patient saw 50% improvement in overall symptoms and body composition when taking small, simple steps in the right direction. She didn’t have to implement any of the lifestyle changes with an all or nothing approach to start feeling better.
- This can be very liberating for patients to know they don’t have to follow a dietary plan 100% to see results. We recommend our patients follow a diet with around 80% compliance, and this is typically all that is required. We don’t recommend 100% strict compliance most of the time because it can be stressful and often unnecessary.
- Her gas and bloating significantly improved with very simple interventions, such as diet, improving sleep, and probiotics. Rather than starting with supplemental ox bile due to her cholecystectomy, we focused on addressing diet and dysbiosis first. If she still had GI symptoms after we went through probiotics, gut supportive nutrients and herbal antimicrobials, then we would consider secretions support.
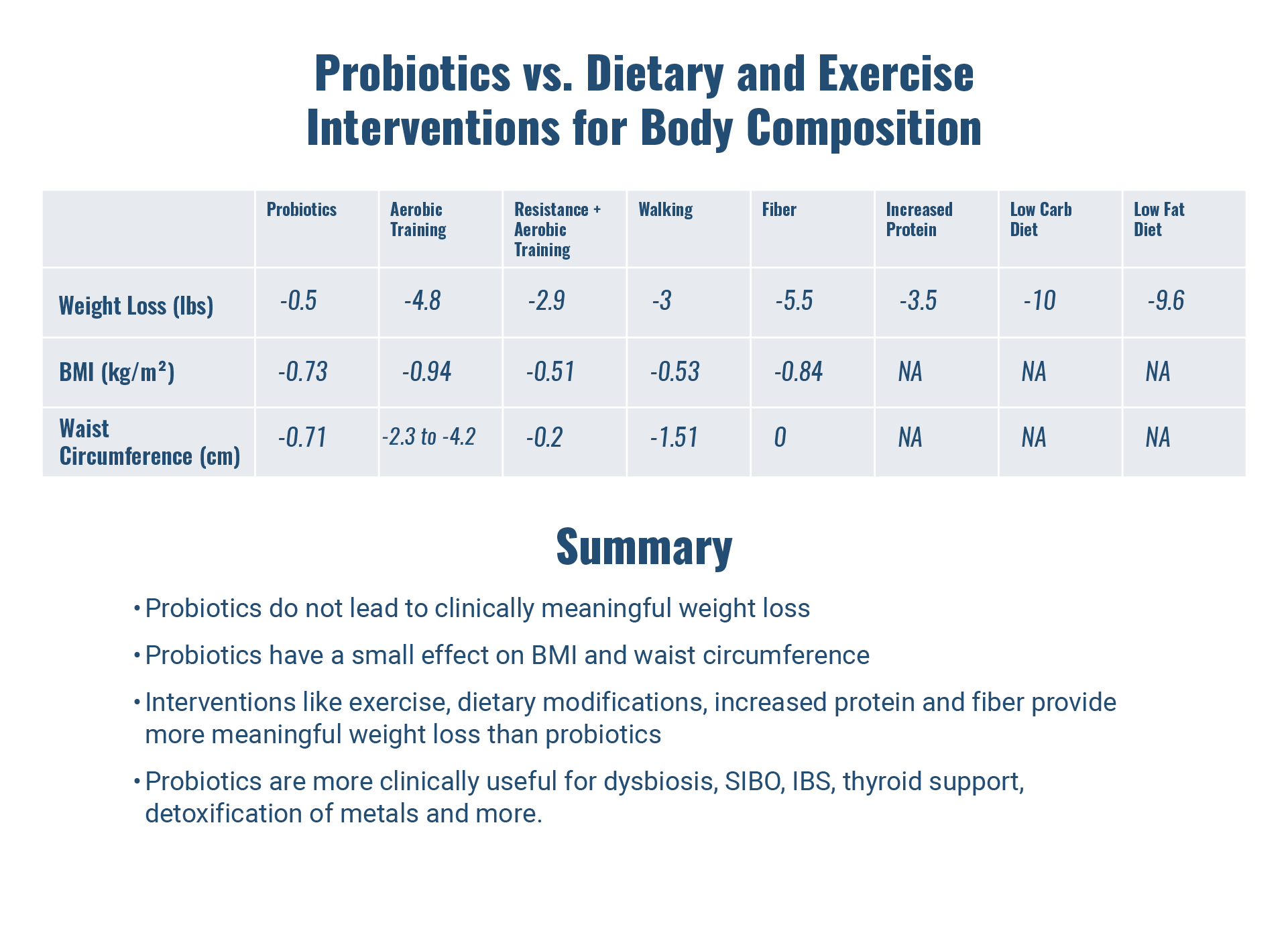
Study Purpose
- Do probiotics improve body composition in a clinically meaningful way?
Study Details
Methods
- 20 RCTs and 1,411 overweight/obese patients treated with control or probiotics (primarily lacto/bifido species)
- Length of treatment ranged from 3 weeks to 6 months (average ~3 months)
Results
- Compared to the control groups, probiotics led to:
- Non statistically significant weight loss (-0.5 lbs)
- Reduced BMI (−0.73 kg/m2)
- Reduced waist circumference (-0.71 cm)
Authors’ Conclusions
- “The results of this meta-analysis highlight a positive trend of probiotics supplementation on anthropometric measures of overweight and obese patients.”
- “Probiotics seem to be mostly effective [in improving body composition] in NASH and metabolic syndrome patients.”
Our Commentary
- Probiotics did NOT lead to significant weight loss, but did improve waist circumference and body mass index. There was a greater signal for improved body composition for those with NASH and metabolic syndrome. This may suggest the improvement in body composition is due to the effect of probiotics on fatty liver and glucose homeostasis, both of which have been demonstrated in research [1, 2].
- While these were statistically significant improvements, are they clinically meaningful?
- One great way to contextualize the significance of these results is to compare them to other interventions, such as exercise and diet.
- 32 RCTs, 4,774 obese participants
- Aerobic training led to the greatest reduction in:
- Weight (-4.8 lbs)
- BMI (-0.94 kg/m2)
- Waist circumference (-2.33 cm)
- Aerobic + resistance training led to reductions in:
- Weight (-2.9 lbs)
- BMI (-0.51 kg/m2)
- Waist circumference (-2 cm)
- Resistance training alone led to NO improvement in:
- Weight
- BMI
- Waist circumference
- 25 RCTs, 1,686 overweight/obese participants treated with various forms of aerobic exercise
- Compared to control groups, waist circumference was reduced with:
- Vigorous intensity aerobic exercise (-4.2 cm)
- Aerobic exercise in general (-3.2 cm
- 32 RCTs with participants randomized to:
- No exercise
- Walking ≥ 1 month
- The walking group experienced greater reductions in:
- Weight (-3 lbs)
- BMI (-0.53 kg/m2)
- Waist circumference (-1.51 cm)
Summary of Exercise Interventions
- Aerobic exercise, specifically intense aerobic training, may lead to the greatest reduction in weight and waist circumference compared to resistance training alone.
- While the study discussed above didn’t show any improvement in body composition with resistance training, this 2022 systematic review and meta-analysis found “compared to no exercise, resistance training reduced body fat percentage by 1.46% and body fat mass by 1.2 lbs.”
- Walking is an effective intervention for improving body composition.
- 12 RCTs, 609 overweight and obese participants, randomized to:
- Control
- Soluble fiber (flax, FOS, galactomannan, GOS, dextrin, glucomannan)
- Soluble fiber led to reductions in:
- Weight (-5.5 lbs)
- BMI (-0.84 kg/m2)
- NO change in waist circumference
- 121 RCTs, 21,942 individuals randomized to:
- Usual diet
- Moderate macronutrient diets (Mediterranean, Jenny Craig, Weight Watchers, etc)
- Low fat diets (Ornish, etc)
- Low carb diets (Atkins, South Beach, Zone)
- After 6 months, all 3 diet categories led to weight loss:
- Low carb (-10 lbs)
- Low fat (-9.6 lbs)
- Moderate macronutrient (-6.6 lbs)
- 37 RCTs involving overweight participants, randomized to:
- Control (increased carbohydrates, fat, fiber, or no treatment)
- Increased protein intake (18 to 59% of total calories)
- Compared to controls, increasing protein intake led to a 3.5 lb reduction in weight
Summary of Dietary Interventions
- Increasing fiber, increasing protein, and implementing numerous dietary interventions (low carb, low fat, moderate macronutrient) all lead to clinically meaningful weight loss.
- The authors of this study stated the “differences in weight loss between popular named diets are small and unlikely to be of importance to those seeking to lose weight.” This study suggests it’s unlikely that one dietary intervention is superior to another when it comes to weight loss.
How This Changes Clinical Practice
Clinical Takeaways
- While the study found probiotics did NOT lead to statistically significant weight loss, it did find that they improved BMI and waist circumference. These results slightly differ from a recent umbrella meta-analysis that found that aside from improving BMI and waist circumference, probiotics did lead to a small reduction in weight. While the results are somewhat mixed, the trend in the evidence suggests the clinical significance for probiotics and weight loss is likely very small.
- Compared to other interventions, probiotics appear to have a small effect on BMI and waist circumference. Waist circumference is highly associated with fatty liver disease [3]. The benefits of probiotics for waist circumference may be due to improvement in liver function, as one umbrella meta-analysis found. Interestingly, this study found probiotics were notably more effective in improving body composition for those with non-alcoholic steatohepatitis (NASH).
- Various dietary interventions, increasing protein and fiber, walking, and exercise (specifically intense aerobic training with resistance training) all have a much larger effect on body composition than probiotics, and should be first-line recommendations for patients desiring weight loss. Probiotics may be considered in those looking to lose weight who also have metabolic syndrome or fatty liver.
Final Comments
- It’s important to be able to guide patients appropriately if they ask about using probiotics for weight loss because it’s what they read on the internet or heard from a friend. While probiotics have a small effect on BMI and waist circumference, there is much more research supporting their use for a myriad of other symptoms/conditions, including IBS [4], SIBO [5] dysbiosis [6], liver disease [7], improving thyroid function [8], detoxification of metals [9], metabolic dysfunction [10], depression [11], food intolerances [12], and more.
Listener asks:
How will Elemental Heal affect insulin resistance?
While there are no studies on this question specifically, we can think through this logically. When we are using an elemental diet, we have to remember 2 important points. First, we are using an elemental diet for the specific reason of improving one’s gut health, which will likely lead to reduced systemic inflammation and thus improved insulin resistance. Second, aside from elemental dieting, there are likely other interventions being used to improve gut health, including probiotics and dietary modifications, both of which improve insulin resistance.
Our standard Elemental Heal powder contains maltodextrin, a rapidly digestible carbohydrate that is broken down into glucose quickly. After consuming the shake, we are likely to see a glucose spike. Luckily, we have a few strategies to mitigate this effect:
- Sip the shake slowly instead of drinking large quantities at one time
- Add fat to your shakes, such as MCT oil/powder
- Add additional protein powder, such as collagen, to your shakes
- Use our low-carb Elemental Heal shake that only contains 17 grams of net carbohydrates per serving
If you try the above methods and blood sugar is still elevating significantly, then using elemental dieting may not be the best approach for the individual. Luckily, we have many other interventions to improve gut health that don’t spike blood sugar, such as diet, probiotics, herbal antimicrobials, and immunoglobulins.
Overall, it is advised that people with diabetes or blood sugar imbalances continue to monitor their blood sugar while on the elemental diet, as they would while eating other foods. Patients who are on insulin should be very cautious with changes in carbohydrate ratios and insulin needs due to rapidly altering insulin sensitivity.