Practitioner Case Study – March 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association with Genotype Pattern or Insulin Secretion: The DIETFITS Randomized Clinical Trial
- Assessment of Anti-Vinculin and Anti-Cytolethal Distending Toxin B Antibodies in Subtypes of Irritable Bowel Syndrome
- Ferritin & Hypothyroid – Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease.
- Thyroid Algorithm Update
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Nicolette, 18yo, Female
- Previous Dx
- Cystic acne
- Rx
- N/A
- Chief Complaints
- Acne
Visit 1 (Day 1) – History and Exam:
Initial Impression:
- Nicolette presents very healthy overall and her parents brought her in for 1/2 wellness check 1/2 trying to determine whats causing skin reactions.
- She has tried diet with minimal response. She has little to no symptoms but does report right before menses her skin seems to be worse suggesting female hormonal issue is probable.
- Trying 30 days on paleo, GI test/treatment, and Herbal HRT should work very well. Use some detox support in conjunction for estrogen clearance.
- Dx/Rx:
- Acne
- Previous Testing:
- n/a
- Onset:
- Skin was clear until around age 13 when her period started. Now she says she notices it happens around her cycles.
- Family History:
- Graves’ Disease
- Prior Treatments:
- Topical antibiotics from a dermatologist
- Notes/DDX:
- She has little to no symptoms but does report right before menses her skin seems to be worse, suggesting female hormonal issue is probable.
- Prognosis:
- GI test/treatment and HHRT should work very well. Use some detox support in conjunction for estrogen clearance.
Previous Diets:
- Has tried diet interventions with minimal response
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing:
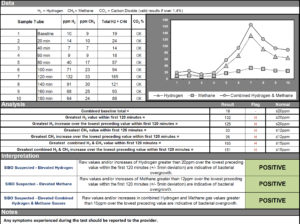
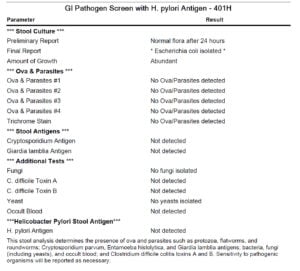
Tests ordered
- NCNM SIBO breath test
- BioHealth 401H stool test
- Blood, Urine, Stool, Breath (LabCorp)
- WBC
- Insulin
- Total Testosterone + Free Testosterone
- DHEA Sulfate
- Complete stool culture
- C. difficile
- H. pylori
- Yersinia enterocolitica
- Giardia + Crypto
- Candida
- Toxoplasma gondii
- E. histolytica
- Trichinella
- Ascaris
- solium
- D-lactate
- Indicans
- Benzoate
- CRP, ESR, Lactoferrin, Calprotectin
Rationale
- We will perform an evaluation for both large intestinal and small intestinal dysbiosis via breath and stool/blood testing.
- We will also perform a standard blood panel, plus thyroid and androgens.
Recommendations:
- Diet: Try 30 days on the paleo diet and then we will reassess.
- NRT: Multi, B complex, Liver/Gall Bladder support supplement (consider amino acids next).
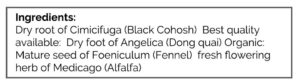
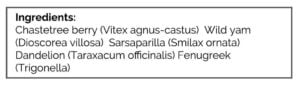
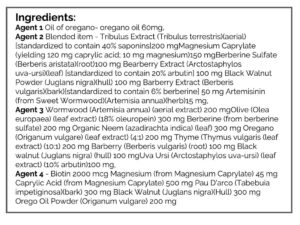
- Hormones: Herbal HRT
- GI: Lacto/Bifido blend probiotic
Rationale
- An elimination diet, dysbiosis, detox, and female hormone support are all warranted
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Doing diet with only a few cheat days
- Skin – 30% better
Lab Interpretation:
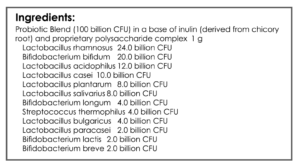
- SIBO Breath test:
- H2: 127, CH4: 11, Combined: 137
- Biohealth:
- Normal
- LabCorp
Diagnosis:
- Severe SIBO, potential candida, and Yersinia. No PCOS/elevated androgens. GI may be contributing to acne.
Impression:
- Diet/hormone supports impact – Minimal, about 30%, but it’s also early so time may increase benefit.
Recommendations:
Starting
- Habx for SIBO, base protocol.
- Temporarily discontinue NRT, so she doesn’t have to be on too many pills at once.
- F/U: 4 weeks, mid-habx treatment.
Visit 4
Subjective Assessment:
- 1st few days of treatment, had stomach
- Skin is 40% improved, still noticing breakouts before her period.
Impression:
- In the last visit, diet and hormone support yielded a 30% improvement. Expecting further after Habx. Today is doing better, but only slightly. FU upon retesting and decide on the next
Recommendations:
- Continue on Paleo diet
- B complex, fish oil, herbal HRT
- Continue Habx, base protocol-2nd month
- Re-test for SIBO and follow up when the results are available
Visit 5
Subjective Assessment:
- Skin is 30-40% better
SIBO Re-Test Result:
- H2: 15, CH4: 18, Combination: 33
Impression:
- Initial diet/program yielded about 30% improvement and GI Habx helped slightly more (10%), but still not fully responsive. SIBO essentially cleared today, could still have potential candida and Yersinia.
- Note: The fact that this marked reduction in SIBO lead to a negligible improvement in skin health makes me question how impactful any gut-skin connection is.
- Today will retest remained of prior GI findings if GI clear and she has still not responded, consider referral to a female/female hormone specialist.
Recommendations:
- Re-test candida/Yersinia.
- Starting on Multivitamin and Omega
- F/U 2-3 weeks after tests are taken
Visit 6
Subjective Assessment:
- Feeling about the same
LabCorp retesting
- Normal: entire panel, including stool culture and candida antibodies.
- Note: Yersinia antibodies were not run
Impression:
- 2/3/16 – Nicolette is still about the same although she feels she was the best when she was on Sept. program indicating NRT, herbal HRT and * Habx were helpful. But, b/c response has been minimal I would like to get female specialists’ opinion.
Recommendations:
- Referring out to female hormone specialist ND
- F/U as needed or if a specialist would like me to follow through on more GI care
Visit 7
Subjective Assessment:
- Was working with a female specialist who suspected prolactinoma. Performed the below treatment with the specialist
- GF Diet – helps stomach ache
- Iron supplement – may have helped
- SIBO – did protocol with a female specialist, helped GI but only helped skin slightly
- Liver support, methylations support, charcoal – not helpful
Outside Labs:
- H: CRP – 4.82, Candida IgM
- L: Ferritin – 14
- WNL: DHEA
SIBO:
- H2: 40/71, CH4: 17/23, Combination: 57/94
Impression:
- Nicolette did hormone support, detox/liver support, and SIBO protocol with specialists office after a referral. The results produced were about the same as from our previous and much simpler protocol from before. She would like to continue care with me in light of this.
- Note:
- The other doctor made a key mistake here, they didn’t listen to the patient and overwhelmed Nicolette with supplements. So, Nicolette returned to my office.
- Also, for low-level prolactinomas treatment is often not recommended. So, in this case, the diagnosis does not change treatment.
- Will start SIBO protocol today with fish oil and recommend considering birth control to help with skin since other therapies have only been slightly helpful. Will also have her use vitex for 6 weeks and then retest prolactin.
Recommendations:
Starting
- NRT: Multi, OmegAvail Synergy
- GI: Primal Defense = probiotic and prebiotic blend
- GI: Habx base protocol
- Female: PhytoProgest
Testing
- perform prolactin testing after 6 weeks
- fu: either in 4 weeks or in 7 weeks
Visit 8
Subjective Assessment:
- Feels about the same midway through the 1st month on Habx.
- Skin is about the same
Impression:
- 6/28/17 – My program has produced minimal change at best. We will continue to 2nd-month Habx and with vitex and then retest prolactin. Will not retest SIBO. At fu consider continuing vitex for prolactin if responding. If not, no further treatment needed. Also, recommending see Ob/Gyn for birth control for the skin.
Recommendations:
- Continue with paleo diet as able
- Stop NRT (multi, fish oil)
- Continue probiotic, Habx, female hormone support
- Retest prolactin and then follow up before returning to school
Visit 9
Subjective Assessment:
- Feels about the same
- Dairy-free diet – helping
- New face wash from the dermatologist – helping
- Was on Phytoprogest for a few months before testing
Outside Labs:
- H: Prolactin – 77
Impression:
- Prolactin has increased markedly from 1 year ago. CRP not assessed. GI may or may not be contributing to acne – appears only minimally.
- Note: today it does not appear that any further dietary or GI treatment is helping. Since Habx only led to a 10% treatment, I do not feel it prudent to continue any further dysbiosis treatment. I’d like to see what her OB can offer for prolactin and/or how birth control may aid in balancing out hormones (although I understand this is a controversial statement).
Recommendations:
- See GP and/or ask for a referral to check in on chronically elevated prolactin. Note it was confirmed 2x by repeat testing.
- Repeat testing of basic blood work, plus potassium and prolactin.
- Perform 1 week trial of the low histamine diet. See website handout.
- Discontinue all items of the program when supply is exhausted.
- F/U as needed
Visit 10
Subjective Assessment:
- Followed up with GP regarding high prolactin. Did MRI – normal results.
- Still notices she is sensitive to gluten.
Lab Results:
- H: Prolactin – 66, Iron – 178
- Normal, but functionally low, Ferritin – 28
- WNL: Vitamin D – 31.8
- UA: Abnormal appearance cloudy, Epithelial cells >10 Abnormal
Impression:
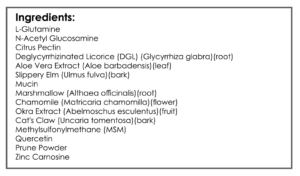
- Prolactin remains elevated. Ferritin is functionally low, despite high iron. Today will start on vitamin D, iron for fatigue and low ferritin, Chaste tree for prolactin and probiotic plus gut support nutrient protocol for potentially improving gluten tolerance. I’m advising to consider red-light therapy for skin also. Also, will refer to a specialist in skin health. Next, consider female hormone detox support, or Walsh detox program for the skin.
Recommendations:
- Start vitamin D/K, Chaste tree
- Begin supplementation with ferrous bisglycinate for 4-5 weeks, then re-test. Ideally would like to see ferritin of at least 100.
- GI: lacto-biff, s. boulardii, soil-based, gut repair nutrient cocktail. Trial for 4 weeks, then trial gluten. Later, experiment with digestive enzymes.
- Platinum LED for skin anti-aging. See podcast.
- F/U as needed or once yearly
Dr. Ruscio’s Comments
You might be asking; doesn’t the low ferritin indicate that she is suffering from a problem in the gut? Yes. However, with a college student you must pick your battles and help cultivate their awareness around diet, or you risk scaring them off. She is learning (experientially) that gluten and dairy bother her, and with my guidance and encouragement (not fear mongering) she is becoming intrinsically motivated to avoid gluten.
At current, I am curious to see if the longer term and a higher dose of vitex will improve prolactin. Also, she may improve after detox support. These are both options we will soon consider.
Also, I hope it is obvious from a practice management/practice building perspective that overzealous treatments, as the female specialist ND offered, will severely limit your practice to only the small subset of people who are OK with taking 18 supplements at a time. This approach is advisable for some patients, but it’s crucially important to meet your patients where they are at. There was a mismatch here, which cost the ND the patient.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!