Practitioner Research Review – June 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- H. pylori & Thyroid Function – Dr. Ruscio’s Mini Review
- This was a bear!
Research
*Please note: The case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however, the research studies are a collection of the most clinically meaningful research that has been published recently.
H. pylori & Thyroid Function – Dr. Ruscio’s Mini Review
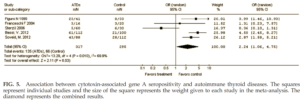
Associations of Helicobacter pylori infection and cytotoxin-associated gene A status with autoimmune thyroid diseases: A meta-analysis
Thyroid. 2013 Oct;23(10):1294-300. doi: 10.1089/thy.2012.0630. Epub 2013 Sep 11.
- Overall, H. pylori infection was associated with autoimmune thyroid disease (abbreviated ATD)
- The association was significant for Graves’ disease but not for Hashimoto’s thyroiditis
- Five of the seven articles reported the association of CagA seroprevalence and autoimmune thyroid disease
- CagA seropositivity significantly increased the risk for ATDs by 2.24-fold
- Here is a breakdown of each study:
- Figura N 1999 had no subgroup analysis of HT patients, mostly Graves’. [1]
- Franceschi F 2004 was not significant for HT. [2]
- Sterzl I 2006 had no subgroup analysis of HT patients. [3]
- Bassi V 2012 was statistically significant for H. pylori-positive HT patients positive for Cag-A antigens. [4]
- Soveid M 2012 was statistically significant for HT patients positive for Cag-A antigens. [5]
- What to tell your patients:
- H. pylori has been associated with thyroid autoimmunity.
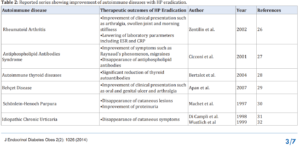
Type B Insulin Resistance Syndrome as an H. pylori-Associated Autoimmune Disease
Imai J, Yamada T, Satoh J, Katagiri H (2014) Type B Insulin Resistance Syndrome as an H. pylori-Associated Autoimmune Disease. J Endocrinol Diabetes Obes 2(2): 1026
Preliminary data support that treatment of H. pylori can improve autoimmune conditions and/or the symptoms associated with a given condition. However, this likely will not apply for all cases.
- Preliminary data shows treatment of H. pylori has improved:
- Symptoms and inflammatory markers in rheumatoid arthritis
- Circulation (Raynaud’s), migraines and antiphospholipid antibodies
- Thyroid antibodies
- Skin conditions: Hives and lesions (Urticaria and Bechet’s disease)
- What to tell your patients:
- H. pylori has been associated with autoimmunity.
- Preliminary data have found the treatment of H. pylori may improve thyroid autoimmunity, but it is not a guarantee and it is not the only factor.
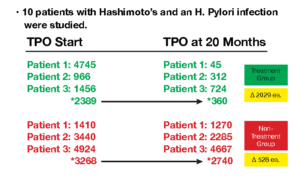
Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection.
Clin Endocrinol (Oxf). 2004 Nov;61(5):650-2.
- This is a summary of the Bertalot et al paper from the table above.
- Summary: Treatment of H. pylori reduced thyroid antibodies
Immunity markers in patients with Helicobacter pylori infection: Effect of eradication
Helicobacter. 2005 Oct;10(5):391-7.
- 86 individuals were entered (43 H. pylori-infected).
- H. pylori infected patients had higher levels of various autoantibodies, including thyroid antibodies.
- Autoantibodies improved after H. pylori eradication, however, thyroid antibodies were not assessed in follow up.
- After 1 year of follow-up, the markers of autoimmunity dramatically improved in patients eradicated for H. pylori infection compared to those where therapy failed. No patient developed a clinical autoimmune disorder.
The role of Helicobacter pylori in patients with hypothyroidism where normal thyrotropin levels could not be achieved despite treatment with high doses of thyroxine.
Helicobacter. 2011 Apr;16(2):124-30. doi: 10.1111/j.1523-5378.2011.00830.x.
- Summary: H. pylori eradication significantly improves thyroid medication absorption and leads to decreased TSH and improved free T3.
- 32 hypothyroid patients completed the study
- A total of 44 patients were assessed in the study. … total of 32 patients completed the study. … Eighteen (56.2%) of the cases were patients with hypothyroidism due to total thyroidectomy (16 cases due to nontoxic multinodular goiter and two cases due to Graves’ disease), 13 cases (40.6%) due to Hashimoto thyroiditis, and one case due to radioactive iodine ablation therapy administered for Graves’ disease (no antibody detection or results reported). …
- TSH, free T3, and free T4 values before H. pylori eradication were as listed below. Note: Antibodies were not assessed.
- 5 IU/mL, 2.64 pg/mL, and 0.92 ng/mL
- and after eradication were found to be
- 2 IU/mL, 3.02 pg/mL, and 1.3 ng/mL
- After H. pylori eradication treatment, TSH decreased in all of the cases. Free T3 also improved.
- Some cases became hyperthyroid due to improved absorption of the medication.
- Factitious thyrotoxicosis developed in 21% of these cases. In hypothyroid cases, H. pylori gastritis may be responsible for an inadequate response to the treatment. H. pylori eradication in the cases receiving high doses of thyroxine showed a risk for thyrotoxicosis.
- Authors’ Conclusion:
- “In hypothyroid cases, H. pylori gastritis may be responsible for an inadequate response to the treatment.”
- What to tell your patients:
- If you are struggling to find the right medication or dose, the problem might be your gut and not the form or dose of medication.
Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis.
N Engl J Med. 2006 Apr 27;354(17):1787-95.
- 11 patients who were treated for H. pylori experienced decreased/improved TSH. Note: Antibodies not assessed.
- “In prospective studies, the occurrence of H. pylori infection in the 11 patients treated with thyroxine led to an increase in the level of serum thyrotropin (P=0.002), an effect that was nearly reversed on eradication of H. pylori infection.”
Tablet and oral liquid L-thyroxine formulation in the treatment of naïve hypothyroid patients with Helicobacter pylori infection.
Endocrine. 2017 Sep;57(3):394-401. doi: 10.1007/s12020-016-1167-3. Epub 2016 Nov 15.
- Summary: H. pylori treatment lead to a reduction of TSH via better absorption of the medication. Antibodies not assessed.
- 28 patients with Helicobacter pylori infection (group A);
- 15 patients without gastric alterations (Group B);
- Subjects were randomly treated with a same dose of LT4 tablet (TAB) or oral liquid formulation (SOL), for 9 months on group A and 6 months on group B. Helicobacter pylori infection was eradicated after 3 months of LT4 treatment.
- When H. pylori patients (with an active infection) were treated with either levothyroxine tablets (aka TAB) or liquid gels (aka SOL), the gel patients had significantly lower (3.6 units) TSH.
- Paraphrase: On group A (SOL), after 3 months (before Helicobacter pylori eradication), subjects showed a greater thyroid-stimulating hormone reduction (3.6 units difference in TSH mU/L) and a greater homogeneity in the thyroid-stimulating hormone values compared to LT4 tablet.
- After H. pylori eradication patients were better able to absorb normal tablet levothyroxine and had better TSH than even the gel group (1.2 units lower).
- Paraphrase: At 9 months (after 6 months of Helicobacter pylori eradication) mean thyroid-stimulating hormone values were lower in subjects treated with LT4 tablet (1.2 units TSH difference, mU/L) compared to liquid gels.
- When compared to a control group, which never had H. pylori, it did not matter if they used gels or tablets.
- Note: This suggests fixing the gut is more important than using a highly absorbable form of thyroid hormone!
- On group B no differences were observed, at each time point, in the mean thyroid-stimulating hormone values and thyroid-stimulating hormone variations between two LT4 formulations.
- What to tell your patients
- Improving your gut health may be more important than using a highly absorbable form of thyroid medication. This has been shown according to studies in those with H. pylori but it may apply to other gut imbalances also.
Here is another study supporting that GI health and malabsorption are an important consideration in patients not fully responding to thyroid medication.
Atypical celiac disease as a cause of an increased need for thyroxine: A systematic study
J Clin Endocrinol Metab. 2012 Mar;97(3):E419-22. doi: 10.1210/jc.2011-1851. Epub 2012 Jan 11.
- Atypical celiac disease = absence of “typical” GI manifestations. Patients present with signs previously considered secondary or unusual accompaniments of celiac disease, such as iron deficiency or elevated liver enzyme levels
- Nothing new here but worth noting, gluten intolerance could be causing non-responsiveness to medication.
- Atypical CD increases the need for T4. The effect was reversed by GFD or by increasing T4 dose. Malabsorption of T4 may provide the opportunity to detect CD that was overlooked until the patients were put under T4 therapy.
And a study showing that those with Hashimoto’s have up to a 40% chance of autoimmune gastritis which causes chronic anemia (malabsorption of iron and/or B vitamins). Hence the tracking of ferritin in my thyroid algorithm.
Hashimoto’s Thyroiditis and Autoimmune Gastritis
Front Endocrinol (Lausanne). 2017 Apr 26;8:92. doi: 10.3389/fendo.2017.00092. eCollection 2017.
- Hashimoto’s thyroiditis (HT) is the most frequent autoimmune disease, and it has been reported to be associated with gastric disorders in 10-40% of patients while about 40% of patients with autoimmune gastritis also present HT.
- The clinical outcome of this gastric damage is the occurrence of hypochlorhydria-dependent iron-deficient anemia, followed by pernicious anemia concomitant with the progression to severe gastric atrophy. Malabsorption of levothyroxine may occur as well.
Association between hypothyroidism and small intestinal bacterial overgrowth (SIBO)
J Clin Endocrinol Metab. 2007 Nov;92(11):4180-4. Epub 2007 Aug 14.
- SIBO was found in 54% of hypothyroid patients, as compared to only 5% in controls.
- However, SIBO treatment had no effect on thyroid hormone levels, in a group of 27 hypothyroid patients.
- Note: I’m currently emailing the authors to determine if they noted any change in antibodies, I’m assuming not since it was not reported. I will update this bullet once I hear back.
- SIBO treatment did improve GI symptoms: Abdominal discomfort, flatulence, and bloating
- Only SIBO treatment study to date (as of May 2019).
- N=90, 50 hypothyroid patients versus 40 healthy controls.
- “A total of 27 patients with a history of hypothyroidism demonstrated a positive result to the breath test (27 of 50, 54%), compared with two in the control group (two of 40, 5%). The difference was statistically significant (P < 0.001).
- Abdominal discomfort, flatulence, and bloating were significantly more prevalent in the bacterial overgrowth positive group. These symptoms significantly improved after antibiotic decontamination.
- Thyroid hormone plasma levels were not significantly affected by successful bacterial overgrowth decontamination.”
- What to tell your patients
- SIBO might be the cause of your thyroid-like symptoms, thus treating SIBO may address the cause. Inferential data exists to support this. It has not yet been published that treating SIBO can lead to reduced medication need, but clinicians do see this.
- Dr. R’s Commentary
- Clinically it does appear treatment of SIBO can reduce the need for thyroid medication, but clinical hunches can be wrong and should be confirmed with a controlled study.
- At first, I wondered if perhaps levothyroxine (as a proxy for most thyroid hormone) was absorbed in the upper SI (duodenum). If so, it would follow that H. pylori could be more impactful on absorption. However, it appears that Levothyroxine is absorbed in the jejunum and ileum.
A number of studies are now finding dysbiosis in those with thyroid disease. Note, this is not causal data.
- “the current study is in agreement with the hypothesis that HT patients have intestinal microbial dysbiosis.”
- Biomed Pharmacother.2017 Nov;95:865-874. doi: 10.1016/j.biopha.2017.08.101. Epub 2017 Sep 10.
- “A significant difference between hyperthyroid and healthy groups … And real-time PCR showed an obvious decrease of Bifidobacterium and Lactobacillus.”
- Curr Microbiol.2014 Nov;69(5):675-80. doi: 10.1007/s00284-014-0640-6. Epub 2014 Jun 27.
- “Characterization of the gut microbiota in HT patients confirmed that HT patients have altered gut microbiota and that gut microbiota are correlated with clinical parameters, suggesting that microbiome composition data could be used for disease diagnosis.”
- Thyroid. 2018 Feb;28(2):175-186. doi: 10.1089/thy.2017.0395. Epub 2018 Feb 1.
Clinical Takeaways:
- The gut-thyroid connection is profound
- Addressing problems in the GI may lead to a reduction of thyroid medication but also an improvement in many non-specific symptoms
- Improving GI health may reduce thyroid, and other, auto-antibodies
- Improving GI health may stabilize medication dose
- Improving GI health may be more important than using a highly-absorbable form of thyroid medication
- Malabsorption, and thus anemias, are increased in hypothyroid patients and should be evaluated
- What to tell your patients:
- The cause of your symptoms might be your gut, let’s start there before considering fine-tuning your thyroid medication.
Dr. Ruscio Comments
This is why the thyroid algorithm is so important. It can be unclear why patient’s symptoms do not fully respond to thyroid hormone, so the clinician must decide to either attempt to fine-tune the thyroid dose or to attend to the GI. Since we know that improving GI health can a) improve symptoms, b) improve thyroid autoimmunity and c) reduce the need for medication, it seems clear that starting with the gut will treat the cause in most (but not all) cases. Also, bear in mind that IBS is more prevalent than hypothyroid, so the odds favor a gut-first approach.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!