Practitioner Case Study – December 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis
- Is SIBO A Real Condition?
- Production and Use of Hymenolepis diminuta Cysticercoids as Anti-Inflammatory Therapeutics.
- Rapid-Fire Research – Ultra-concise summaries of noteworthy studies
- Treatment of irritable bowel syndrome with probiotics. An etiopathogenic approach at last?
Practitioner Question of the Month
Case Study
SIBO Labs & Symptoms Improved, But GI-Map Become Worse… Atrantil vs Antimicrobials For SIBO And Dysbiosis; Habx More Effective.
Patient info:
- Ilana, 36y/o, Female
- Previous Dx
- n/a
- Rx
- n/a
- Chief complaints
- Bloating & Gas – 10 – constant
- Hair loss – 6 – constant
- Weight gain – 8 – constant
- Joint pain – 7 – intermittent
- Reflux – 7 – intermittent
- Low energy/mood – 7 – intermittent
- Other symptoms
- Constipation
- Acne
- Female – mild
- Thyroid – moderate
- Allostatic load – mild
Visit 1 (day 1) – History and Exam:
Initial impression
- Ilana presents as a generally healthy 36yo female with a good lifestyle, demeanor, and outlook on her health.
- Dx/Rx:
- n/a
- Previous testing:
- Low/normal ferritin
- Onset:
- Longstanding problems with weight, bowels, and sleep. Much antibiotic use for the throat. History of mast cell activation disorder.
- Family history
- Heart disease, Type 2 Diabetes
- Prior Treatments:
- Acupuncture has helped her previous female hormone imbalances.
- Enzymes/HCl helped GI, PPIs did not.
- Notes/DDx
- She is likely suffering from typical GI imbalance; SIBO, dysbiosis, etc. and will do well with standard therapies.
- Other DDX are possible including; histamine overload/MAC and pelvic adhesions.
- Prognosis
- Should do well with the standard approach. Prognosis is good to excellent.
Previous diets
- She has done better on a higher carb/lower fat, nightshade-free diet, with grains but no gluten.
- Ayurvedic diet (no wheat, cut certain veggies, less protein, thoroughly cooked veggies, more legumes) – very helpful.
- Paleo made her gain weight.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Tests ordered
- Aerodiagnostics Lactulose SIBO breath test
- GI-MAP stool test
- LabCorp 1
- CMP, CBC w/ differential, lipid panel, iron panel
- Fasting insulin, Hemoglobin A1c
- TSH, Free T4, vitamin D
- Erythrocyte Sedimentation Rate, C-Reactive Protein
- LabCorp 2
- pylori: Blood, breath, and stool
- Rationale
- Standard GI workup.
- Plus extra close attention for pylori since history suggests (reflux)
Recommendations
- Diet:
- Perform modified fast for 2-4 days
- Follow the Low FODMAP diet but also work to incorporate helpful aspects of previous Ayurvedic diet; high carb/lower fat, avoiding nightshades.
- Do your best to avoid gluten and wheat more strictly for the next 30 days.
- Finally, take steps to follow a rotation-like diet; meaning don’t eat the same thing every day but rather work to plan variety.
- Exercise:
- Exercise: incorporate resistance training into your program, shoot for resistance training 2x more than cardio. Circuit training is a good way to get intensity with resistance training.
- NRT: Vitamin D/K, Omega-3 supplement, Multivitamin
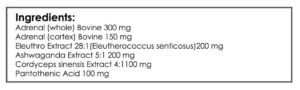
- Adrenal: Adrenal support
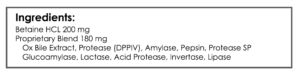
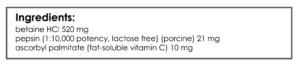
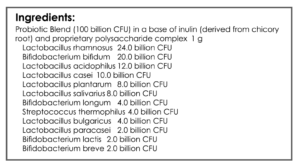
- GI: Digestive enzymes, Betaine HCl, lacto-bifido probiotic, S. boulardii
- Note: Start supplements after 2 weeks on a diet
- Follow Up: 6-7 weeks
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Modified fast (4 days, broth) – slight improvement; reflux, bloating. Slight fatigue.
- Low FODMAP w/ Ayurvedic combo diet – helpful.
- Has not yet started on supplements.
- Improved:
- Bloating, weight gain, joint pain, energy
- Same:
- Hair loss, reflux, acne
- Worse:
- Constipation
Lab interpretation:
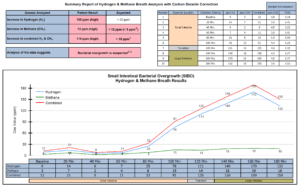
- SIBO breath test: H2: 76/111, CH4: 15, combo: 91/125
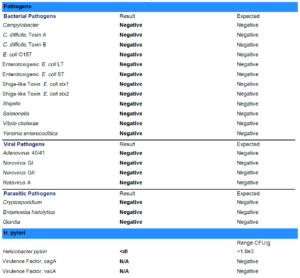
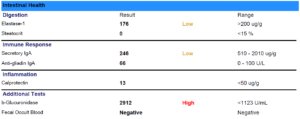
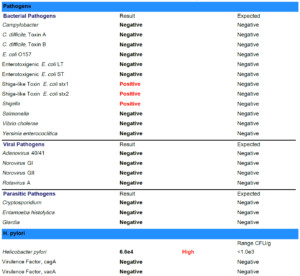
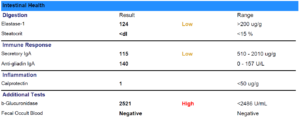
- GI-Map: Blasto H. Yeast – Geotrichum spp., Citrobacter freundii.
- Additional testing: unremarked
Impression:
- Ilana has SIBO which likely underlies most of her secondary symptoms. Has previously responded well to the previous diet of higher carb Ayurveda. Modified fast was helpful. FODMAP combo w/ Ayurveda – helpful. Today will continue on with the plan, starting the initial supplement program soon (had not yet started at today’s visit). Then will follow up and asses if herbal antimicrobials are needed; Atrantil only. If minimally responsive, consider other ddx.
Recommendations
- New:
- Start on supplement program recommended at last visit
- Follow up: 2-3 weeks
Visit 4
Subjective Assessment:
- Been on initial program 2 weeks now – improving.
- Improved:
- Energy/mood (much better), bloating/gas (much better but not gone), constipation
- Same:
- Reflux, weight, hair loss
- Worse:
- n/a
Impression:
- Improving nicely from the addition of initial program (NRT, Adrenal, and GI support) but secondary symptoms are still present, so will start on Herbal antimicrobials (Atrantil) only today then follow up in four weeks.
Recommendations:
- New:
- GI: Atrantil only (4 pills, 2-3x per day). Atrantil only study group (for a while I was comparing Atrantil to traditional herbal antimicrobials).
- Follow Up: 4 weeks
Visit 5
Subjective Assessment:
- Atrantil (4 weeks) – No response. Feels about the same as her last visit.
- But did eat off plan a little bit and had some stress. Has had a bit of nausea as well.
- Improved:
- n/a
- Same:
- Reflux, weight, hair loss, energy/mood, bloating/gas, constipation
- Worse:
- n/a
Impression:
- Ilana’s improvements have plateaued and even regressed slightly from Atrantil. Nausea and skin reactions reported today. She elected to continue with another 4 weeks. Then we will be collecting symptom survey again, retesting for SIBO, and starting a prokinetic. Will retest other findings after SIBO.
Testing:
- Tests ordered
- Aerodiagnostics Lactulose SIBO breath test
Recommendations:
- New:
- Continue to 2nd month with Atrantil, but take with food.
- Once you have finished the Atrantil complete your symptoms survey.
- Perform retesting within 1 week of ending the Atrantil.
- Once off Atrantil, start on MotilPro or Iberogast – whatever is easier to obtain.
- Follow Up: 2 weeks after re-test has been sent in.
Visit 6
Subjective Assessment:
- Reaction to Atrantil abated when taking with food. Generally, is feeling better than at last visit.
- Tried MotilPro and experienced nausea and heartburn.
- 6 weeks of pelvic adhesion therapy – think it’s helping even though it doesn’t seem to have changed.
- Improved:
- Bloating/gas (still present), acne (much better), joint pain, weight, reflux
- Same:
- Hair loss, fatigue
- Worse:
- Constipation
Lab interpretation:
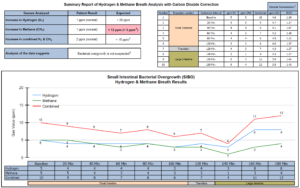
- SIBO breath test: Normalized
Impression:
- GI support program and later Atrantil produced marked reduction in H2 and also reduced CH4. Atrantil reactions completely abated when taking with food. Subjectively is improved but still has residual chief complaints. Today we’ll retest previous findings along with GI-Map. Also, starting on full program (ran out of items), along with magnesium, intermittent fasting, and pelvic adhesion therapy. Discontinue MotilPro due to reaction.
Testing:
- Tests ordered
- Diagnostic Solutions GI-Map
Recommendations:
- New:
- Discontinue Atrantil.
- Continue to experiment with intermittent fasting
- GI: magnesium citrate
- When going back on to, or returning to the full dose, start one at a time and see if you can notice what is helping and what is not.
- Discontinue MotilPro, we will consider Iberogast in the future if needed.
- Continue work with local physiotherapist for pelvic adhesions.
- Follow Up: 2 weeks after re-test has been sent in.
Visit 7
Subjective Assessment:
- Has been traveling which has made following a diet more difficult.
- Magnesium citrate – either no response or too much.
- Intermittent fasting was very helpful.
- Adrenal support – larger dose, helpful.
- Acne has regressed.
- GI is better than she thought it would be considering travel/food. Still having some reactions.
- Improved:
- Same:
- Subjectives not assessed – appears to be improving overall.
- Worse:
- Acne
Impression:
- GI-Map retesting results are pending.
- Today is overall better, especially despite traveling to US and eating way off plan. Overall has plateaued at a good level.
- I’m hopeful we have achieved balance in GI and with time will continue slow, steady improvements. Decided to maintain current program for now.
Recommendations:
- New:
- Continue with intermittent fasting and Natural Calm
- Continue with the rest of your program
- GI: Consider a trial of Iberogast
- Follow Up: 6-8 weeks
Visit 8
Subjective Assessment:
- When she returned from vacation, she felt like she regressed to her baseline. Could have been from diet and from coffee. She then tightened up her diet and stopped coffee and has been getting better again – is almost back to her previous peak improvement now.
- Good lesson here, don’t freak out if your patients hit a speed bump.
- Improved:
- Bloating/gas (though still present), acne (much better), joint pain, weight, reflux, constipation, fatigue
- Same:
- Hair loss
- Worse:
- Insomnia
Lab Interpretation:
- GI-Map: pylori, Blastocystis hominis, Geotrichum spp., Shigella, Cyclospora
Impression:
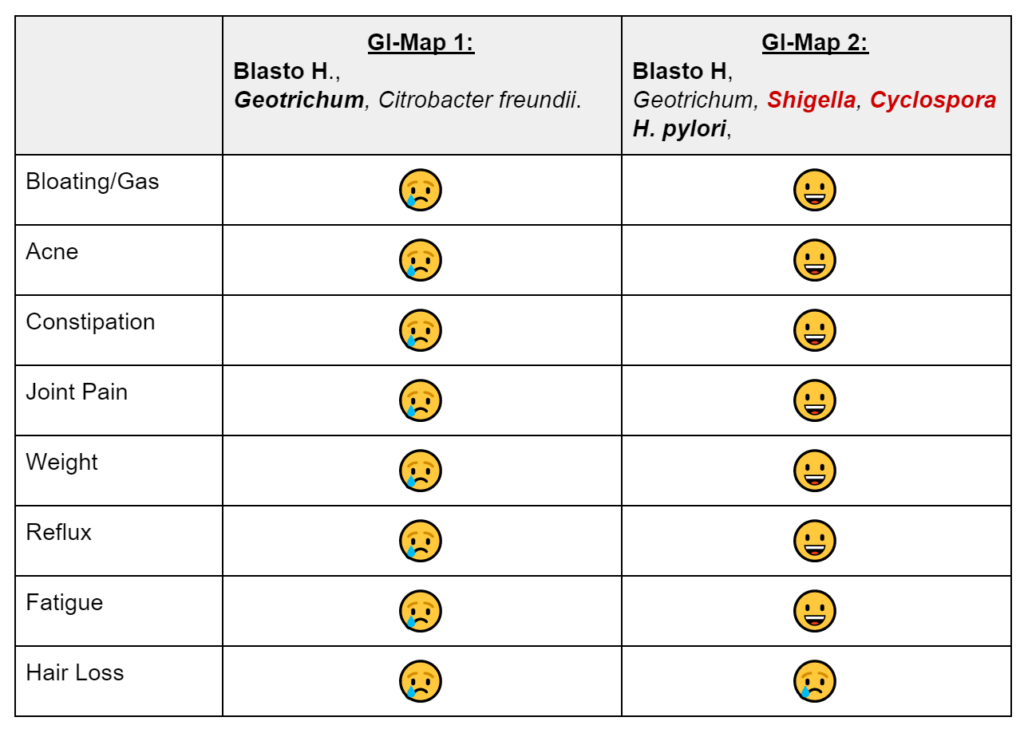
- GI-Map retesting paradoxically shows previous Blasto and Geotrichum still present, plus now positive for pylori, Shigella, and Cyclospora. Likely false positives, because SIBO and chief complaints have dramatically improved. And because we ruled out HP via blood and breath prior. Today, we decided on another round of herbal antimicrobials, this time non-Atrantil only.
- See table below which makes it easier to see that despite the fact that there are more positives on 2nd GI-Map, her symptoms are vastly improved. This test must be interpreted with caution and in the context of the patient.
- Bold = potential pathogen, Red = pathogen.
Recommendations:
- New:
- Have a snack before bed and see if this helps you sleep
- Experiment with melatonin as a sleep aid
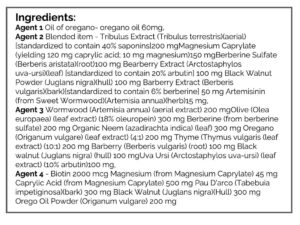
- GI: Herbal antimicrobials, base protocol
- Do not take the Iberogast while on the antimicrobial program
- Follow Up: 4 weeks into antimicrobial program
Visit 9
Subjective Assessment:
- Herbal antimicrobials were very helpful. Left her stressful job around the same time. **part of the reason I favor standard antimicrobials over Atrantil**
- Improved:
- Food tolerance, bloating/gas, acne (much better), joint pain, weight, reflux, constipation, fatigue, insomnia.
- Same:
- Hair loss
- Worse:
- n/a
Impression:
- Antimicrobials (she took both months in 1 month) were very effective, more so than Atrantil. All chief complaints have markedly responded (other than hair loss). Today will discontinue all supplements other than probiotics, and then fu in 8-12 weeks. If improvements maintained, we’re done. If regressed, consider low-dose cyclical antimicrobials.
Recommendations:
- New:
- Discontinue herbal antimicrobials, digestive enzymes, and betaine HCl
- Wean off of everything in program other than the two probiotics.
- Continue to use magnesium as needed for bowels.
- Follow Up: 8-12 weeks
Dr. Ruscio’s Comments
I had 2 more follow ups with Ilana. She was able to come off HCl, enzymes and probios with no regression. She was also able to broaden her diet in time.
This case study exemplifies a few important points
- A new/novel treatment (Atrantil) doesn’t mean it is any better than the current treatment. This distraction is a major reason why some providers see subpar results, don’t let this be you.
- DNA-based lab tests suffer from false positives and therefore must be interpreted in the context of the patient.
- Small regression often occur, don’t let this cloud your judgment and make sure to reassure your patient.
How are you feeling about the GI-Map test? We’ve covered a few case studies illustrating the nuance of using this test. I hope you are starting to develop a healthy respect for this test as being good, but not infallible. Please let me know what you think in the comments below.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!