Practitioner Case Study – February 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- DIAGNOSIS OF ENDOCRINE DISEASE: How Reliable Are Free Thyroid and Total T3 Hormone Assays?
- The Omega-3 Index: A New Risk Factor for Death From Coronary Heart Disease.
- An Italian Prospective Multicenter Survey on Patients Suspected of Having Non-Celiac Gluten Sensitivity.
- Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement.
Practitioner Question of the Month
Practice Tip
![]()
Case Study
Patient Info:
- Caitlyn, 32yo female
- Dx: Hashimoto’s
- Rx: N/A
- Chief complaints
- Bloating, 8
- Abdominal distension, 8
- Weight gain, 5
- Mental fog, 7
- Female: cycle length, flow, pain, PMS
Visit 1 (day 1) – History and Exam:
Initial Impression
- Caitlyn presents as a 32yo female who is generally in good health with a healthy lifestyle and a good outlook on her health. She could improve her diet, however.
- A few years ago some of her CCs started first with bouts of vomiting that had no known cause, and then she gradually experienced development of her other CCs with time.
- She has been dx and treated for SIBO and blasto with only minimal change; 1x Rifax/Neo, 1x Flagyl/Bactrim. She also had IgM+ for Candida. She does also have low but positive TPO abs; euthyroid. Prior endoscopy wnl.
- She will likely need standard SIBO care and will respond well since she hasn’t done much outside of Abx and has not tried diets or Habx. She has responded slightly to enzymes, B12, and iron.
- Caitlyn also exhibits symptoms consistent with female hormone imbalances which seem to provocate GI, so support here should yield good results.
- Potential for SIFO due to candida IgM. Possible APCA due to symptoms and AIT.
- Has done no prior FM care. Prognosis good to excellent.
Previous Diets
- N/A
Previous Treatments
- Neo/Rifax – helped
- B12/Iron – helped energy slightly
- Flagyl and Bactrim – no change
- Probio – no change
- Enzymes – helps slightly
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Diagnostic Solutions GI-MAP stool test
- LabCorp #2 blood & urine
- LabCorp #1 blood, urine , stool & breath
- Rationale
- We will perform our standard GI workup with tests for SIBO, dysbiosis, and GI pathogens. Will also order our standard blood/urine panel to assess CBC, CMP, Diff, TSH, fT4, vitamin D, etc.
- We will also check thyroid antibodies and thyroid metabolites
Recommendations
- Dietary:
- Please start on the Paleo Low FODMAP diet
- Work to wean yourself off coffee and use a non-coffee alternative; tea, natural energy drinks, etc.
- Supplemental:
- NRT: Omega 3,6,9 blend; Vitamin D/K
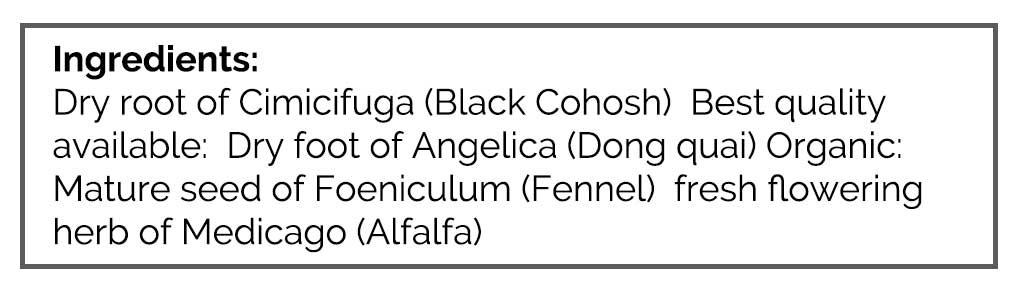
- Female: Herbal blend for estrogen, herbal blend for progesterone
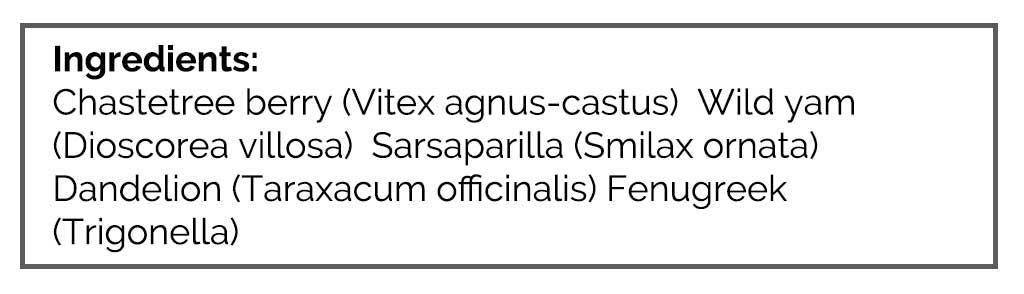
- GI: Lacto-Bifido probiotic, s. boulardii probiotic, digestive enzyme with HCl, betaine HCl
- Be on a diet for 1.5 weeks before starting a supplement program
- Be on supplement program for 1.5 weeks before starting on the Digestive Support supplements in the program
- Rationale
- Diet is a great place to start given her GI symptoms; however, we could have started even more simply with orthodox paleo. She stated an aggressive preference in her paperwork, hence my recommendation here (yes, there is a method to the madness).
- Her initial program will help replete deficiencies, balance female hormones, and start the process of addressing GI dysbiosis.
Visit 3 – Lab Interpretation and Treatment Evaluation
Lab Interpretation:
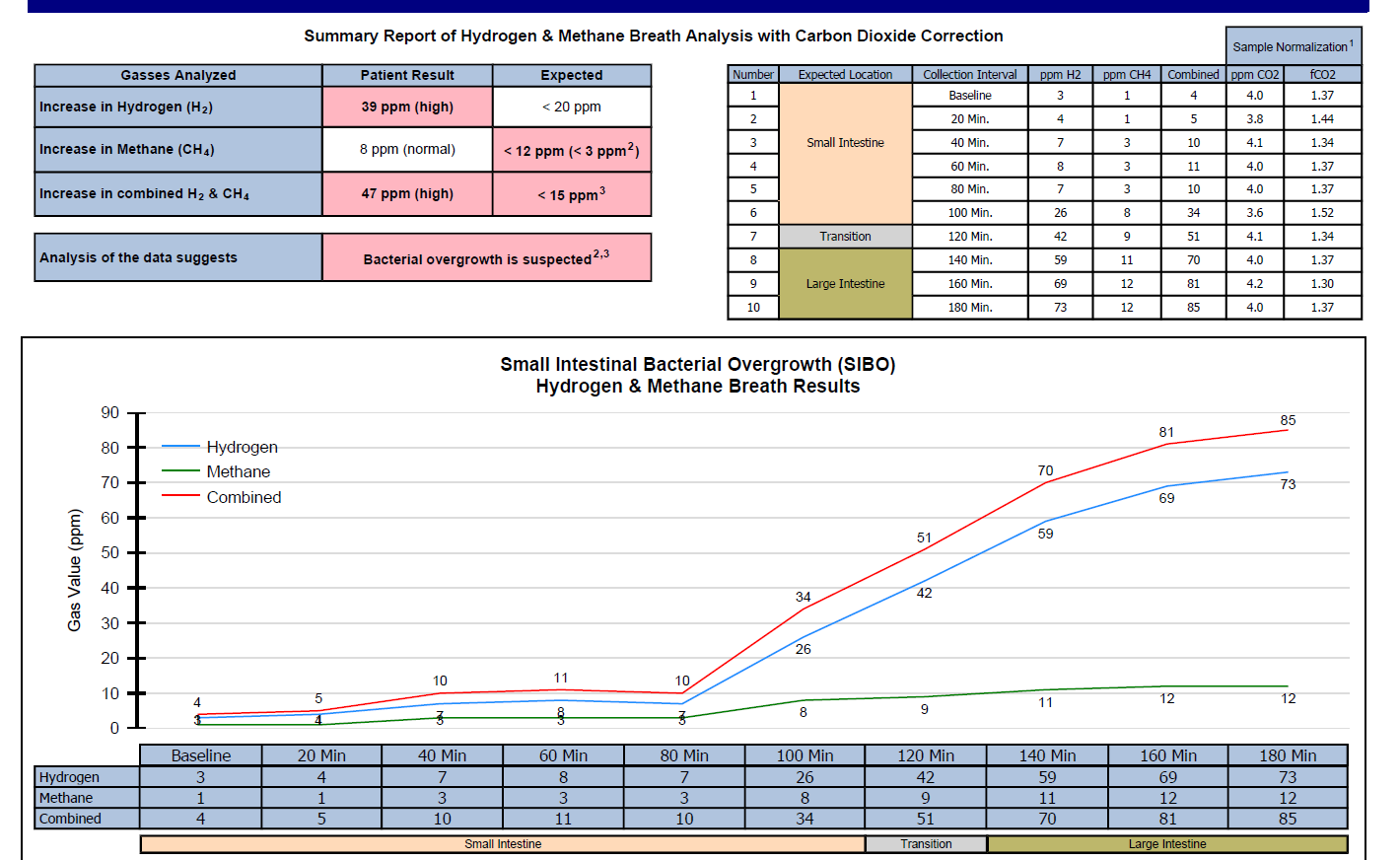
- Aerodiagnostics Lactulose SIBO breath test
- H2 26/42, CH4 8/9, combo 34/51 100/120
- Diagnostic Solutions GI-MAP stool test
- Blasto, Geotrichum spp., Calp 106, B-glucuronidase
- LabCorp #2 blood & urine
- Cholesterol 252-H, LDL 148-H, EOS 0.7-H, UA – abnormal cloudy
- t4 4.3-L, fT4 0.73-L, TPO Ab 45-H, TGA 1.9-H
- LabCorp #1 blood, urine , stool & breath
- H. pylori IgA, IgG, IgM IgM 11.8-H
- Yeast Only, Culture w Reflex to ID (stool) Geotrichum Candidum 1-2 colonies
- Indicans, urine qualitative + Abnormal
- Dx
- Mild mixed H2 predominant SIBO. LC: Yeast, low T4, managed AIT. DS: Blasto, Yeast, CalP.
Subjective Assessment:
- 3/14/17 pt was diagnosed by her ob-gyn w/ PCOS & was instructed to start Medroxyprogesterone. Dx via the US.
- Paleo low FODMAP – v. helpful; bloating, distension, mental fog
- Initial program: Betaine – v. helpful for bloating
- Coffee wean – no change
- Improved:
- Bloating, distension, mental fog
- Same:
- Constipation, cycle length, flow, pain, PMS
- Worse:
- N/A
Impression:
- Today’s labs show SIBO, Yeast (LC and DS) and potential blasto, also managed AIT. She has been treated for SIBO, Blasto, and yeast 1x and was minimally responsive. Will start today with Habx protocol, plus Artemisinin, plus anti-biofilm agents, and up the dose to full dose probiotics (had previously been using a lower dose).
- Has responded very well to paleo low FODMAP and mildly to initial program. Has recently been dx with PCOS via the US, but hormones are wnl. OB just started on progest, so monitor female symptoms and eval if herbal hormone support is helping.
Recommendations:
- Maintain previous program.
- Plus start on:
- You can bring coffee back in 🙂
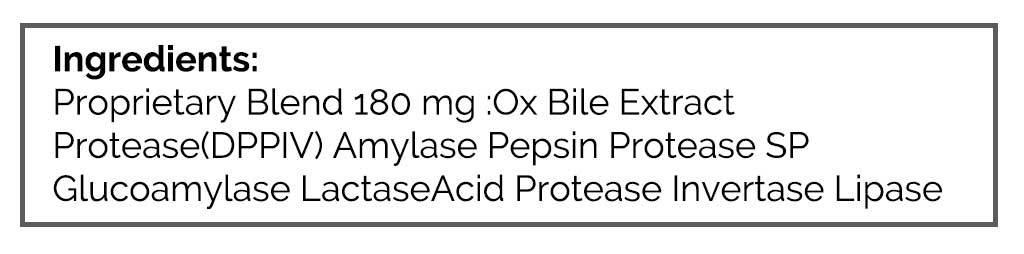
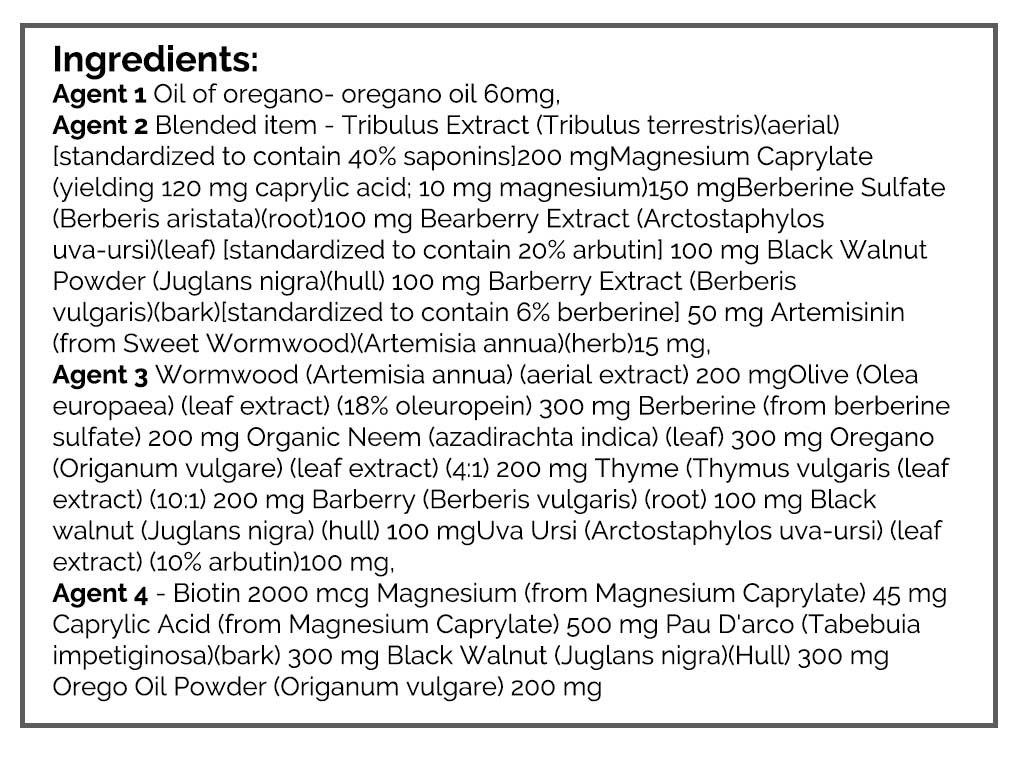
- GI: Habx; base protocol (2 formulas for one more, 2 different for the second month), Artemisinin, biofilm agent
- Start with full dose probiotics
- Follow-up: 5 weeks
- Rx: Medroxyprogesterone
- LabCorp #2 blood & urine
- Basics, additions | Cholesterol 252-H, LDL 148-H, EOS 0.7-H, UA – abnormal cloudy
- Thyroid full | t4 4.3-L, fT4 0.73-L, TPO Ab 45-H, TGA 1.9-H
- Testo f/t, DHEA | wnl – see outside labs. T4 normal also.
- LabCorp #1 blood, urine , stool & breath
- Fecal Fat | WNL
- APCA, IF Abs | WNL
- Stool Culture, complete | WNL
- Clostridium difficile Toxins A and B, EIA | WNL
- H. Pylori stool antigen | WNL
- H. Pylori IgA, IgG, IgM | IgM 11.8-H
- H. Pylori Breath Test | WNL
- Yersinia Enterocolitis IgM, IgG, IgA | WNL
- Yersinia Stool Culture | WNL
- Ova and Parasites 3x Examination w/o Giardia | WNL
- GIARDIA AND CRYPTOSPORIDUM Ag | WNL
- Yeast Only, Culture w Reflex to ID (stool) | Geotrichum Candidum 1-2 colonies
- Candida Antibodies, IgA, IgG, IgM, ELISA | WNL
- Toxoplasma gondii Antibodies, IgG | WNL
- Toxoplasma gondii Antibodies, Quantitation, IgM | WNL
- Toxoplasma gondii, PCR (whole blood) | WNL
- E histolytica, Amebic Antibodies | WNL
- Trichinella (Tissue Worm) Ab, SIgA
- Ascaris (Roundworm) Ab, IgE | WNL
- T. solium (Tapeworm) Ab, serum (aka Cysticercus Ab, serum) | WNL
- Indicans, urine qualitative | Positive Abnormal
- Benzoate | n/a
- Eosinophil Cationic Protein ( Eos. protein X) | WNL
- White Blood Cells (WBC), Stool | unable to run w/ specimen
- CRP (c-reactive protein) (non-HS) | WNL
- Calprotectin, Fecal | WNL
- ESR (Sedimentation Rate, Modified Westergren) | WNL
- Lactoferrin, Quantitative, Stool | WNL
- Occult Blood, Fecal, Immunoassay | WNL
- parietal cell ABs (APCA) | WNL
- Inflammatory Bowel Disease (IBD) Expanded Profile; ACCA, ALCA, AMCA, gASCA, pANCA. | WNL
Visit 4
Subjective Assessment:
- Habx + biofilm agent + Artemisinin – very helpful, finished 2 months, 1 month ago
- Progesterone – helpful; started cycling
- Mag Citrate – helps bowels
- Is now more alcohol tolerant
- Improved:
- Bloating, distension, body weight, mental fog, constipation
- Female: skin, PMS, no periods
- Same:
- N/A
- Worse:
- N/A
Impression:
- Caitlyn has responded very well to 2 months Habx + artemisinin + biofilm agent, Mag Citrate for bowels, and to progesterone Rx. No further improvement is needed, so we will maintain the current plan and then follow up in 2 months and move to first perform dietary reintro and then also reduce program.
- Today we will also take off herbal est/progest support since she came off 1 month ago with no change (she was confused regarding the program and came off herbal support when starting on Rx). Consider retesting previous findings at follow up, especially low T4, TPO.
Recommendations:
- Maintain previous plan
- Stop now: PhytoEst, PhytoProgest
- Follow up: 2 months
Visit 5
Subjective Assessment:
- Has been doing well and improved even more since our last visit. Has had some gas returning when eating off plan foods (processed, beer, etc.…)
- Improved:
- Body weight, mental fog, constipation
- Female: skin, PMS, no periods
- Same:
- Bloating, distension
- Worse:
- N/A
Impression:
- Today Caitlyn has continued to improve; she does notice some bloating when eating off plan foods occasionally. No further improvement needed. Today we will have her perform dietary reintro, followed by program curtail. We will not retest. Follow up as needed or once yearly.
Recommendations:
- First perform dietary reintro and then also reduce program. Try to find minimal dose needed.
- Follow up: as needed or for once yearly check in
Dr. Ruscio’s Comments
Caitlyn has responded very well to dietary change, treatment of gut dysbiosis, and some Rx hormonal support. She is happy with her current level of improvement. Yes, she does experience some symptoms if she eats unhealthy food, but that is not abnormal. With time she will likely see gradual improvement in her food tolerability, but will likely always feel some regression when eating too much unhealthy food. Again, this is normal.
There is a temptation to do more, mainly testing in her case. However, I don’t think this is needed today. We can give her some time, and if she starts to regress in the future, we can retest to identify what is driving the regression. Then, we could treat that specifically. Testing often guides treatment. Since we do not need to treat her anymore today (her clinical goal has been reached) the need for testing is minimal. Had we been tracking a frank disease, like hypothyroid or diabetes, that requires ongoing monitoring and adjustment of treatment, then testing would make more sense. Dysbiosis, in my opinion, does not play by these same rules. As her gut and gut immune system continues to heal/balance, her dysbiosis may continue to improve. So, a minor imbalance found today may right itself on its own with time.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!