Practitioner Research Review – February 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- DIAGNOSIS OF ENDOCRINE DISEASE: How Reliable Are Free Thyroid and Total T3 Hormone Assays?
- The Omega-3 Index: A New Risk Factor for Death From Coronary Heart Disease.
- An Italian Prospective Multicenter Survey on Patients Suspected of Having Non-Celiac Gluten Sensitivity.
- Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement.
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
DIAGNOSIS OF ENDOCRINE DISEASE: How Reliable Are Free Thyroid and Total T3 Hormone Assays?
https://www.ncbi.nlm.nih.gov/pubmed/27737898
Study Purpose
- To review the difference between T4 and T3 testing methodologies; comparing the more commonly used immunoassay to the dialysis methodology.
- Abbreviations:
- Immunoassays = IA
- Liquid chromatography-tandem mass spectrometry = LC-MS/MS
Intervention:
- Review, non-systematic
Main Results:
- Immunoassays may be less accurate because their results can be confounded by binding proteins.
- “Immunoassays for free thyroid hormone are affected by alterations in serum binding proteins that occur in many physiological and disease states.”
- This may result in patients who test “normal” for both free and total T4/T3, but who actually test “low” when tested via the dialysis method.
- “Multiple studies show falsely normal values for T3, FT3, and FT4 by immunoassay that are below the reference interval when measured by (ultrafiltration) LC-MS/MS, a reference method. We suggest evaluation of thyroid hormone levels by ultrafiltration LC-MS/MS for patients who continue to experience hypothyroid symptoms on LT-4.”
- Therefore, using the dialysis method appears a reliable measure for identifying those who would benefit from the addition of T3 to their medication.
- “This may help identify the approximately 20% subset of patients who would benefit from the addition of T3 to their treatment regimen (combination therapy).”
- The dialysis method may also help identify formerly subclinical hypothyroid cases as frank hypothyroid, thus assisting in the decision to initiate thyroid medication.
- “Jonklaas et al. reported lower TT3 values by ultrafiltration LC-MS/ MS compared with a chemiluminescent immunoassay platform in patients with TSH over 4.5 mIU/L.”
- “…patients with high concentrations for TSH often had thyroid hormones below the reference interval for LC-MS/MS that were misclassified as normal by immunoassay.”
- “A study of 40 patients classified as subclinical hypothyroidism by elevated TSH with normal FT4 levels by conventional immunoassay found that 65% of such patients actually had FT3 or FT4 levels below the reference range by ultrafiltration LC-MS/MS.” (1)
- “Jonklaas et al. reported lower TT3 values by ultrafiltration LC-MS/ MS compared with a chemiluminescent immunoassay platform in patients with TSH over 4.5 mIU/L.”
- TSH and symptoms may more closely track with dialysis T4s than immunoassay T4s.
- “…these papers have shown a poor correlation of immunoassay values for FT4, FT3, and TT3 with log TSH or TSH as well as with the patient’s clinical condition.”
Additional Results:
- Certain medications may also skew the results of immunoassay testing by affecting binding proteins, such as furosemide, salicylate, anti-epileptics, and heparin.
- The majority of patients with functionally low FT4/T3 may actually be diagnosable as frankly low when testing via the dialysis method.
- “Measurement of those samples for FT4 and free 3,5,3′-triiodothyronine (FT3) by ultrafiltration LC-MS/MS demonstrates that 2 out of 3 individuals classified as subclinical by immunoassay have FT4 or FT3s below the 2.5th percentiles and are therefore now classified as clinically hypothyroid.”
- Free T3 and T4 is a more clinically relevant measure than total.
- “The measurement of FT3 and FT4 is the most clinically relevant for the evaluation of thyroid disorders, with total thyroid hormones being affected by variations in binding protein concentrations.”
- The dialysis method essentially filters binding proteins that can skew the results of T4 and T3 testing.
- “An important distinction between the immunoassay and LC-MS/MS methods is that the latter removes the thyroid-binding proteins before measurement of FT4 and FT3 levels.”
- The paper cites a case study showing comparison of immunoassay to dialysis findings.
- The drawback to this method is that it is more expensive and takes longer to process.
Author’s Conclusion:
- “Measurement of TT3, FT3, and FT4 by the immunoassay methods commonly used by the majority of laboratories is problematic, especially for low levels of thyroid hormones. A significant number of patients are misclassified as having normal levels of thyroid hormones when they actually have levels below the reference range by LC-MS/MS.”
Interesting Notes:
- Hypothyroidism affects roughly 5% of populations in developed countries, while subclinical affects roughly 10%. Compare this to IBS, which affects roughly 20%, another reason why mastering the gut is so important – IBS affects more than twice as many people. Shh, but don’t tell the thyroid-fear-mongering circles on the internet.
Clinical Takeaways:
- The dialysis method of testing T4s and T3s appears more accurate than the immunoassay method.
- The dialysis method may identify:
- Those who require the addition of T3 to their T4 medication (poor converters)
- Those previously thought to be SCH as frank hypothyroid
- May not suffer from inaccuracy due to medication use or variations in binding protein levels.
Dr. Ruscio’s Comments
This method may identify those who are true hypothyroid who were previously thought to be SCH. That being said, it is unclear whether all these cases may require or benefit from thyroid hormone treatment. Remember that the most compelling data for improved patient outcomes is treating those with SCH with a TSH above 8-10. So, if you find a formerly SCH case as true hypothyroid when using the dialysis testing, mind the level of TSH to help guide decision making.
When using the dialysis method, it may no longer be required to use functional ranges. In fact, one could make an argument that using the dialysis method + normal ranges is more accurate than the immunoassay + functional ranges. The functional ranges were a good start, but my thinking is this is the evolution of functional markers, because we now take the guesswork out of the equation. Specifically, we literally can filter out particles in the blood that may confound our results when using the dialysis method.
The Omega-3 Index: A New Risk Factor for Death From Coronary Heart Disease?
https://www.ncbi.nlm.nih.gov/pubmed/15208005
Study Purpose
- Assess the validity of omega-3 intake and the “Omega-3 Index” to predict coronary heart disease risk.
Intervention:
- Clinical and laboratory experiments, combined with a non-systematic review of the literature.
Main Results:
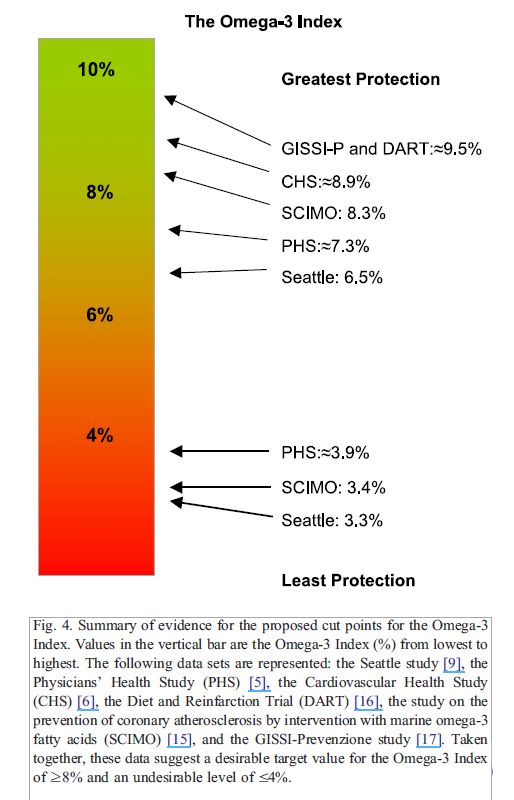
- “The Omega-3 Index was inversely associated with risk for CHD mortality.”
- “An Omega-3 Index of ≥ 8% was associated with the greatest cardio-protection, whereas an index of ≤ 4% was associated with the least.” Note: here they are citing the various trials supporting the Index.
- The Omega-3 Index had a high correlation with the more traditional measure of whole blood omega-3s.
- “Correlation coefficients between the Omega-3 Index and whole blood omega-3 FA (Fig. 2) and plasma phospholipid EPA + DHA (Fig. 3) were both >0.9 .”
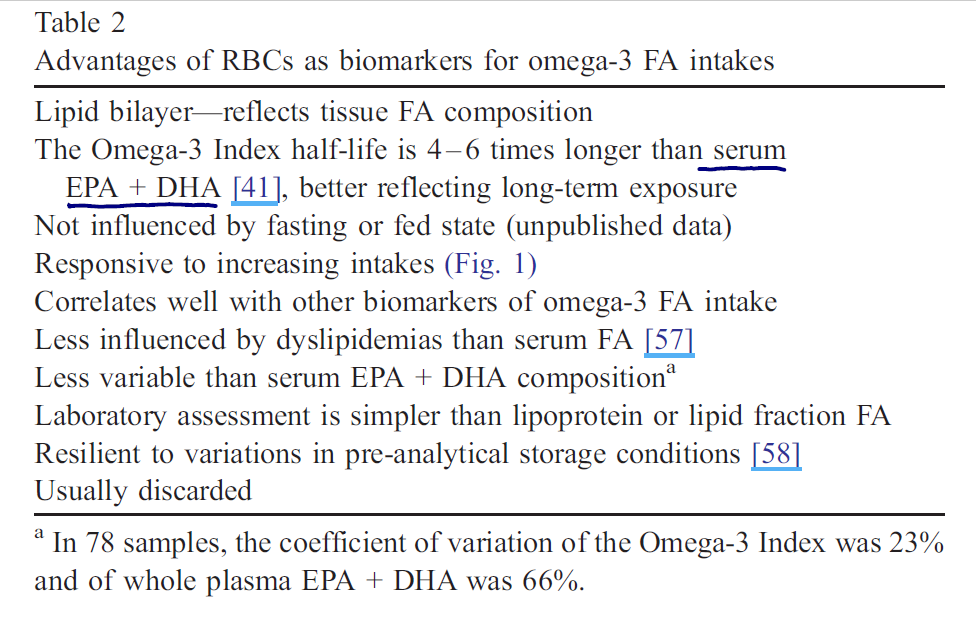
- The Omega-3 Index may be better than the traditional whole blood omega-3 testing for several reasons.
Additional Results:
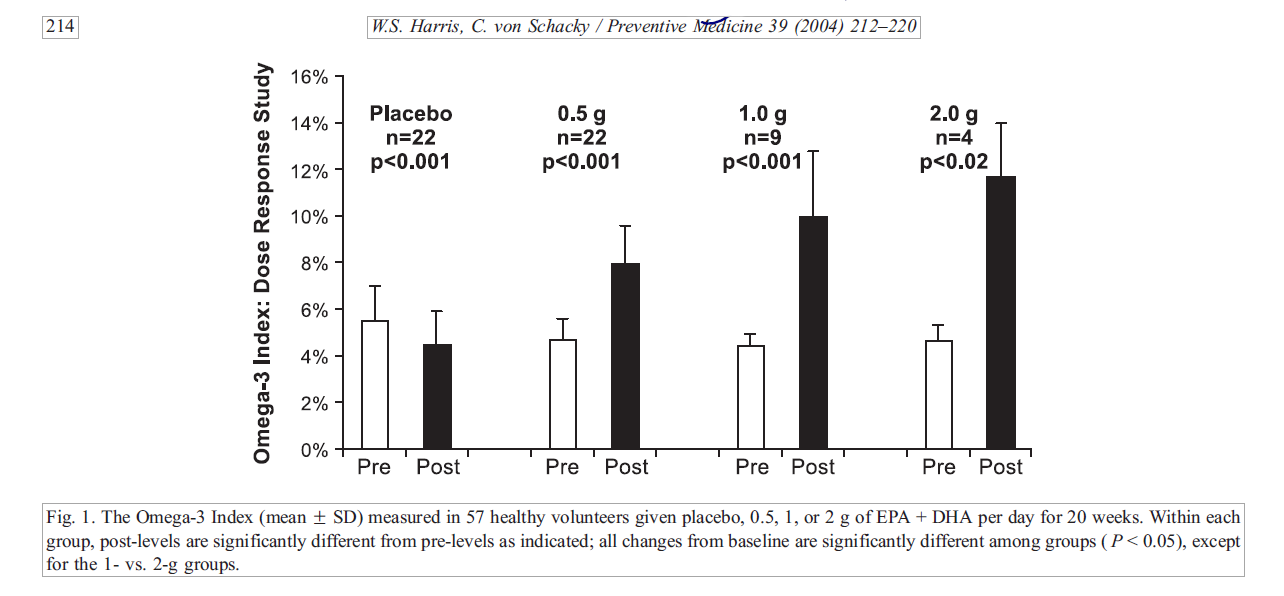
- One study found 1 gram per day of fish oil as adequate; more benefit occurred at 2 grams per day, but the additional benefit was not significant.
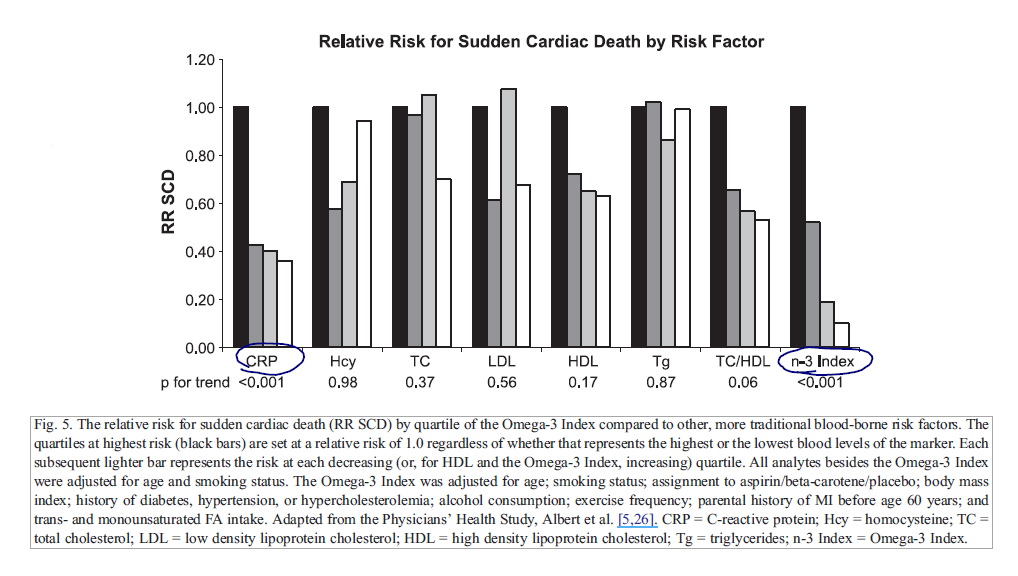
- The authors speculate that the Omega-3 Index may be a more accurate predictor than C-reactive protein.
- “Omega-3 Index were adjusted for several potential confounders, those for C-reactive protein were only adjusted for age and smoking status. Thus, the Omega-3 Index may be a more informative risk factor than C-reactive protein.”
- They continue that it might be more predictive than a number of other markers, including cholesterol and homocysteine for predicting sudden cardiac death.
- They also cite there is no risk for blood thinning when using fish oil.
- “There is, however, no evidence that EPA and DHA increase risk for clinically significant bleeding [35], nor that they interact adversely with other drugs used to treat CHD, including antiplatelet agents [36,37].”
Authors’ Conclusion:
- “The Omega-3 Index may represent a novel, physiologically relevant, easily modified, independent, and graded risk factor for death from CHD that could have significant clinical utility.”
Interesting Notes:
- “The American Heart Association (AHA) now recommends about 1.0 g/day of EPA + DHA to reduce the risk for death from CHD in the secondary prevention setting.”
- “…for individuals without known disease (primary prevention), the AHA recommends the consumption of at least two, preferably oily, fish meals per week. This amount of fatty fish would provide about 500 mg of EPA + DHA per day.”
Clinical Takeaways:
- The Omega-3 Index may predict coronary heart disease risk and guide the dietary intake of fish and supplementation of fish oil to reduce risk.
- This test is available through Quest and Genova
Dr. Ruscio’s Comments
The data here are not perfect and are preliminary, so caution is warranted. For example, some of the studies assessed fish consumption and drew an inference that a corresponding level of supplementation would achieve the same benefit.
I think a reasonable recommendation would be to strive to obtain an Omega-3 Index score equal/greater than 8 via fish consumption and to use fish oil supplementation if one falls short. Roughly 2-3 servings of oily fish per week should achieve this.
This marker requires further validation and study, but could prove a useful tool, especially to increase compliance with fish consumption and/or fish oil supplementation.
Where to get this test? Currently looking into this, more to follow here.
An Italian Prospective Multicenter Survey on Patients Suspected of Having Non-Celiac Gluten Sensitivity.
https://www.ncbi.nlm.nih.gov/pubmed/24885375
Study Purpose
- To assess the prevalence, co-morbidities, and other factors associated with non-celiac gluten sensitivity.
Intervention:
- Prospective, multi-center survey study. Pooling data from 38 Italian centers and 12,225 patients.
- Physicians tracked data in a comprehensive 60-point questionnaire which included data regarding history, family history, symptoms, lab testing, intestinal biopsy, and associated disorders.
Main Results:
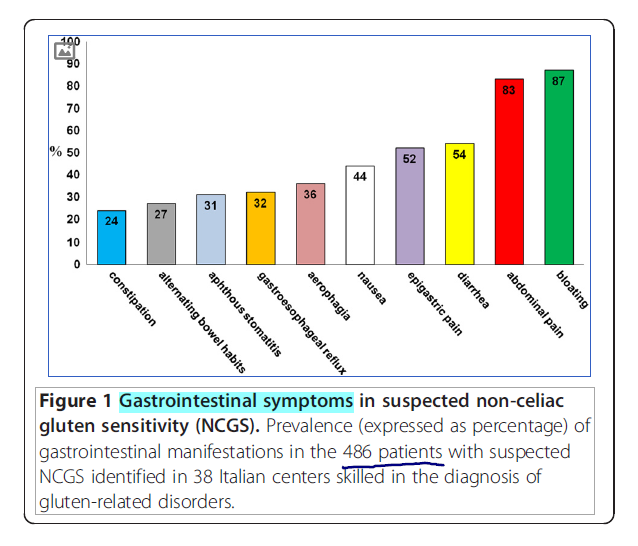
Symptoms of NCGS
- Included a mixture of gastrointestinal and extra-intestinal symptoms.
- Most common digestive symptoms were bloating, abdominal pain, and diarrhea.
- The clinical picture was characterized by combined gastrointestinal symptoms (abdominal pain, bloating, diarrhea and/or constipation, nausea, epigastric pain, gastroesophageal reflux, aphthous stomatitis)
- The clinical picture was characterized by combined gastrointestinal symptoms (abdominal pain, bloating, diarrhea and/or constipation, nausea, epigastric pain, gastroesophageal reflux, aphthous stomatitis)
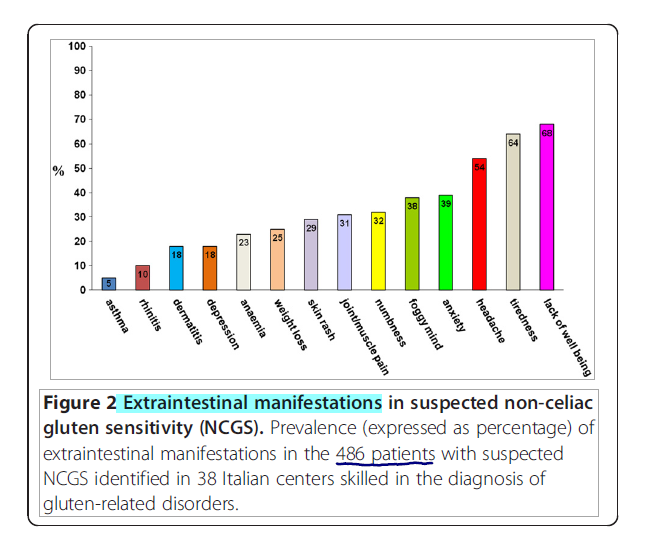
- Most common extraintestinal symptoms were lack of well-being, fatigue, and headache.
- And systemic manifestations (tiredness, headache, fibromyalgia-like joint/muscle pain, leg or arm numbness, ‘foggy mind’, dermatitis or skin rash, depression, anxiety, and anemia)
Time to reaction after gluten ingestion
- Over 90% of cases experience reactions within 24 hours…
- “In the large majority of patients, the time lapse between gluten ingestion and the appearance of symptoms varied from a few hours to 1 day”
- …whereas celiac patients may not experience symptoms for weeks.
- “In the large majority of our patients with suspected NCGS, the time lapse between gluten ingestion and the occurrence of symptoms varied from a few hours to 1 day, whereas in CD this interval is much longer (up to weeks or years)”
- This is why and where obtaining a celiac diagnosis can be helpful. Here is what I would recommend for these cases:
- 1st Test HLA-DQ2 and DQ8
- If negative = no celiac
- If positive = need to rule out celiac
- 2nd Perform celiac screening
- A 6-week reintroduction of gluten is required first for those who have been gluten-free historically
- 1st Test HLA-DQ2 and DQ8
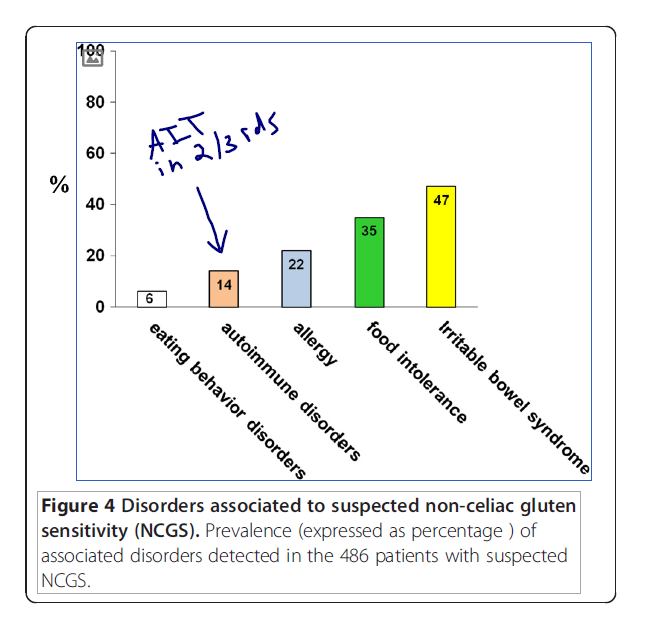
Associated disorders, including autoimmunity
- IBS and food intolerances were the most common.
- “The most frequent associated disorders were irritable bowel syndrome (47%), food intolerance (35%) and IgE-mediated allergy (22%).”
- Autoimmune disease was detected in 14% of cases. Two-thirds of these cases were autoimmune thyroid.
- “An associated autoimmune disease was detected in 14% of cases.”
- “Mainly represented by autoimmune thyroiditis, detected in two-thirds of the NCGS autoimmune sub-group.”
- “An associated autoimmune disease was detected in 14% of cases.”
- This connection to autoimmunity refutes two other papers finding low association.
- 18% of cases had a relative with celiac.
- “Regarding family history, 18% of our patients had a relative with celiac disease.”
Testing
- HLA-DQ2/8 genotyping does not appear helpful.
- “No correlation was found between NCGS and positivity for HLA-DQ2/-DQ8.”
- Anti-gliadin IgG might be the best test
- “IgG anti-gliadin antibodies were detected in 25% of the patients tested.”
- However, keep in mind that anti-gliadin IgG is not diagnostic by itself.
- “These antibodies are not specific for NCGS, being also found in CD, auto-immune liver disorders, connective tissue disease and IBS, as well as in healthy controls [26], but their finding in patients with a clinical picture consistent with NCGS has been regarded as an element supporting this diagnosis [27].”
- Intestinal biopsy showed Marsh 1 in roughly 30% of cases
- “normal intestinal mucosa (69%) or mild increase in intraepithelial lymphocytes (31%).”
- “Duodenal biopsy was performed in 302 (62%) of the 486 patients, with the finding of Marsh 0 in 209 cases (69%) and Marsh 1 in 93 cases (31%) according to the modified Marsh-Oberhüber classification [13].”
- Signs of malabsorption are also reported, including low ferritin, folic acid, and vitamin D.
- “Laboratory tests displayed low levels of ferritin, folic acid, and vitamin D in 23%, 5%, and 11%, respectively, of patients with suspected NCGS.”
Prevalence
- Slightly more common than celiac, just over 1% of general population and just over 3% of at-risk/suspected populations. Note: this is far less than some internet sources or gurus would lead you to believe.
Additional Results:
- Double-blinded studies have shown varying findings regarding the prevalence of NCGS. As much as 10-fold in some cases. This is why it’s important not to indoctrinate your patients into thinking they have NCGS.
- “Indeed, in a number of patients classified as being gluten-sensitive and put on a gluten-free diet (GFD), the double-blind reintroduction of gluten did not result in recurrence of the symptoms, which were instead evoked by the ingestion of placebo.”
- “studies in the USA have reported a large variability in NCGS prevalence with figures ranging from 0.6% in primary care to 6% in tertiary care”
- “Indeed, in a number of patients classified as being gluten-sensitive and put on a gluten-free diet (GFD), the double-blind reintroduction of gluten did not result in recurrence of the symptoms, which were instead evoked by the ingestion of placebo.”
- 30% of cases of NCGS might resolve by treating an underlying GI issue, including SIBO or other food intolerances.
- “In one recent study, a reassessment of patients who had decided by themselves to avoid gluten allowed an alternative diagnosis to be made in about 30% of cases; these diagnoses included small intestinal bacterial overgrowth, fructose or lactose intolerance, microscopic colitis, gastroparesis, and pelvic floor dysfunction.”
Authors’ Conclusion:
- “This prospective survey shows that NCGS has a strong correlation with female gender and adult age. Based on our results, the prevalence of NCGS seems to be only slightly higher than that of celiac disease.”
Interesting Notes:
- The Dx of NCGS was not performed via the gold-standard elimination followed by double-blinded reintroduction. They instead used the self-reported reaction to gluten. This may lead to a significant overreporting of the rate of reaction to gluten, as some studies have shown people will react to placebo upon reintroduction.
Clinical Takeaways:
- Non-celiac gluten sensitivity may impact roughly 3% of at-risk populations.
- A reaction upon reintroduction will occur within 24 hours in over 90% of NCGS cases.
- NCGS can manifest as both gastrointestinal and extra-intestinal symptoms.
- HLA-DQ2/8 testing does not appear accurate for NGCS; anti-gliadin IgG might be, however.
- If HLA-DQ2/8 testing is positive, the patient may have celiac.
- 30% of NCGS may have another underlying GI issue driving their symptoms, including SIBO.
- Placebo may be responsible for some cases of NGCS.
- NCGS may be related to autoimmune conditions, mainly autoimmune thyroid.
Dr. Ruscio’s Comments
Whew, there is a lot here. The clinical takeaways pretty much sum this up, but remember that while NCGS is an issue, it might not be as prevalent as purported in some circles. So, be objective to help prevent your patients/clients from falling into unnecessary food avoidance and fear.
Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement.
https://www.ncbi.nlm.nih.gov/pubmed/28492905
Study Purpose
- Update recommendations for thyroid cancer screening.
Intervention:
- Review, non-systematic
Main Results:
- There is a lack of evidence to support screening (in non-symptomatic adults) mainly because:
- It is rare,
- Outcomes for those treated versus monitored appear similar,
- Mass screening programs lead to no change in mortality, and
- “The USPSTF found inadequate direct evidence on the benefits of screening but determined that the magnitude of the overall benefits of screening and treatment can be bounded as no greater than small, given the relative rarity of thyroid cancer, the apparent lack of difference in outcomes between patients who are treated vs monitored (for the most common tumor types), and observational evidence showing no change in mortality over time after introduction of a mass screening program.”
- Screening may be net harmful.
- “The USPSTF found inadequate direct evidence on the harms of screening but determined that the overall magnitude of the harms of screening and treatment can be bounded as at least moderate, given adequate evidence of harms of treatment and indirect evidence that overdiagnosis and overtreatment are likely to be substantial with population-based screening. The USPSTF, therefore, determined that the net benefit of screening for thyroid cancer is negative.”
- Those who may benefit from screening:
- “persons who experience hoarseness, pain, difficulty swallowing, or other throat symptoms or persons who have lumps, swelling, asymmetry of the neck, or other reasons for a neck examination.”
- “persons at increased risk of thyroid cancer because of a history of exposure to ionizing radiation (eg, medical treatment or radiation fallout), particularly persons with a diet low in iodine, an inherited genetic syndrome associated with thyroid cancer (eg, familial adenomatous polyposis), or a first-degree relative with a history of thyroid cancer.”
Additional Results:
- Again, screening in asymptomatic adults may be harmful.
- “The USPSTF concludes with moderate certainty that screening for thyroid cancer in asymptomatic persons results in harms that outweigh the benefits.”
Authors Conclusion:
- The USPSTF recommends against screening for thyroid cancer in asymptomatic adults.
Interesting Notes:
- N/A
Clinical Takeaways:
- Screening for thyroid cancer should be reserved only for those with the above symptoms.
Dr. Ruscio’s Comments
We recently discussed the finding that those with Hashimoto’s are at increased risk for thyroid cancer. My position has therefore been to follow whatever recommendations were suggested by the patient’s endocrinologist or GP. This paper fills in any gaps in our understanding that an up-to-date endo/GP will only recommend screening if the patient presents with certain symptoms or history. This is reasonable and makes sense.
The fact that after initiating an early detection campaign the mortality rate stayed the same suggests no benefit from early detection. When this is combined with evidence that shows potential harm from screening, it becomes apparent why a conservative recommendation is given here.
I hope that the knowledge of the association between Hashimoto’s and thyroid cancer does not fall into the wrong hands where I could see it being used as another point of fear mongering used to scare thyroid patients into compliance.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next Practitioner Question of the Month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine.

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!