Practitioner Case Study – August 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- A concise, practical guide to diagnostic assessment for mast cell activation disease
- A Paleolithic-type diet results in iodine deficiency: a 2-year randomized trial in postmenopausal obese women
- Exercise Modifies the Gut Microbiota with Positive Health Effects
- Rapid-fire Research – ultra concise summaries of noteworthy studies
- Functional 13C-urea and glucose hydrogen/methane breath tests reveal significant association of small intestinal bacterial overgrowth in individuals with active Helicobacter pylori infection.
- Differences of microbiota in small bowel and faeces between irritable bowel syndrome patients and healthy subjects.
- Unfavorable Course of Subclinical Hypothyroidism in Children with Hashimoto’s Thyroiditis Compared to Those with Isolated Non-Autoimmune Hyperthyrotropinemia.
- Tablet and oral liquid L-thyroxine formulation in the treatment of naïve hypothyroid patients with Helicobacter pylori infection.
- In patients with subclinical hypothyroidism while in therapy with tablet l-t4, the liquid l-t4 formulation is more effective in restoring euthyroidism.
- Retrospective Study of Patients Switched from Tablet Formulations to a Gel Cap Formulation of Levothyroxine: Results of the CONTROL Switch Study.
Practitioner Question of the Month
Practice Tip
Case Study
Fatigue, Rashes, Brain Fog & Bloating Resolved In 2 Months By Ignoring and NOT Treating Contradictory Stool Test Results Nor Treating Positive SIBO Breath Test Results.
Patient Info:
- Colin, 27yo, male
- Previous Dx
- na
- Rx
- na
- Chief complaints
- Fatigue, 6-INT
- Skin Rash, 6-CO
- Brain Fog, 5-INT
- Bloating, 6-CO
- Muscle Weakness, 5-INT
- Weight Gain, 5-CO
- Other Symptoms
- loose stools
Visit 1 (day 1) – History and Exam:
Initial impression
- Colin presents as a 27yo male on a vegetarian diet, with a good lifestyle and outlook on his health.
- Previous testing:
- Showed potential EBV reactivation
- His CCs started after use of abx and since his CCs included GI its very likely that all CCs are emanating from dysbiosis post-Abx.
- Has responded well to monolaurin and to probiotics. Has done little/no FM or GI work.
- No unusual ddx to consider. Should respond very well to standard GI care.
- Prognosis excellent.
- Notes/DDX
- SIBO
- SIFO, H2S SIBO
- Dysbiosis
- GI infection
- —
- coffee intolerant
- histamine overload, MCAD
- —
- HPA dysfunction, mod
- Hypothyroid
- low androgens
- —
- Hg tissue burden
- EBV reactivation
Previous Diets
- GF and low sugar – helpful. DF helpful.
Previous Treatments
- Monolaurin (for EBV) – helpful. Probiotics – helpful.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Diagnostic Solutions GI-MAP stool test
- Diagnostechs GI-15
- Quest blood & urine
- Rationale
- The gastrointestinal symptoms could indicate dysbiosis
- The dermatological and neurological symptoms could indicate dysbiosis also
- A routine blood/urine assessment should be performed to screen for high blood, sugar, anemia, hypothyroid, etc.
Recommendations
- Dietary
- please perform the Modified Fast for 2-4 days (see website for PDF), then
- please start on the Paleo Low FODMAP diet
- please discontinue coffee, for now, you can use other sources of caffeine though
- Supplemental
- after 2 weeks on diet/lifestyle plan, start on supplements. Be on the supplements for at least 3 weeks before our follow up.
- NRT: vitamin D/K, omega 3-6-9 blend
- Adrenal: Preg, DHEA
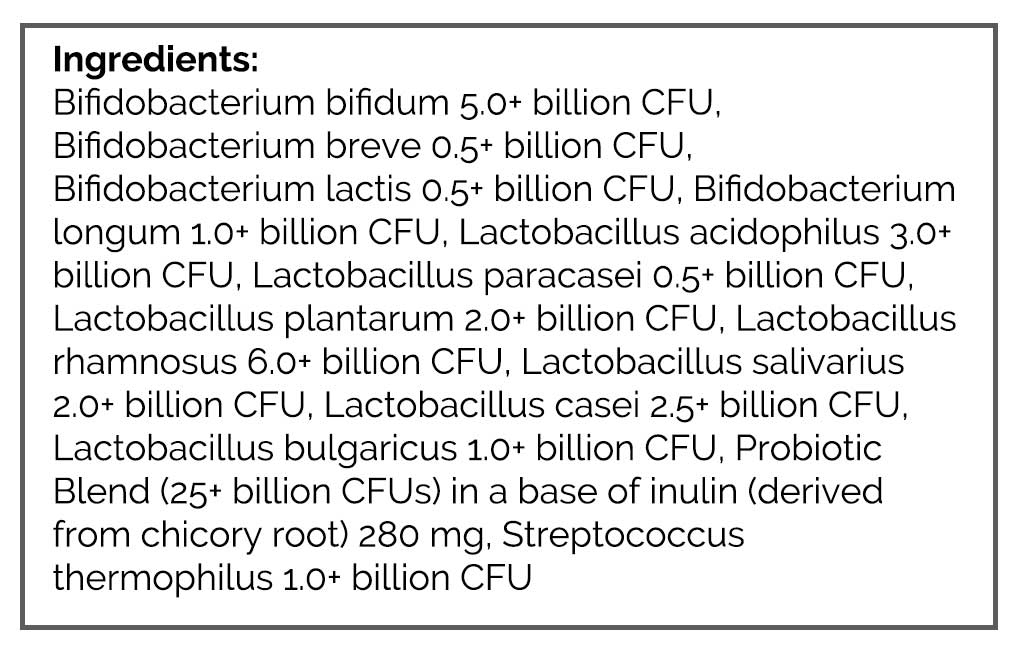
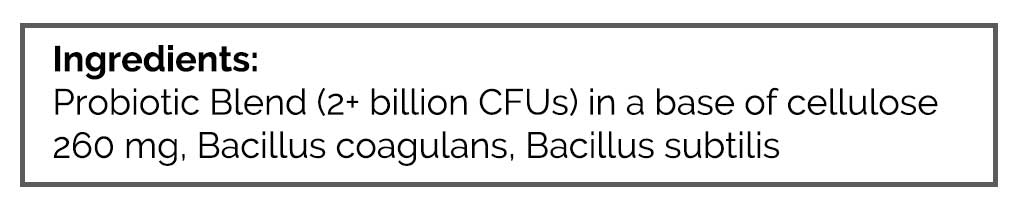
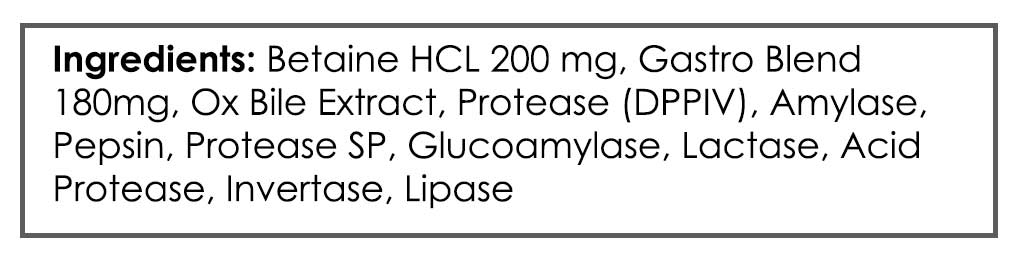
- GI: Lacto-Biff probiotic, S. boulardii, Soil-based probiotic, a digestive enzyme with HCl
- Rationale
- A modified fast may help acutely reduce inflammation and GI reactivity
- FODMAPs and coffee could be a dietary GI irritant
- Adrenal support may help with the fatigue and brain fog
- Probiotics and enzymes might be all that is needed to resolve any GI symptomatology and remedy any dysbiosis
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- MF (4day, MC) – symptoms all improved, and maintained some improvement weeks since. Flared skin slightly.
- Paleo Low FODMAP – helpful
- d/c coffee – helped.
- Initial supplement program – helped skin, bloating.
- Improved:
- weight gain (lost 20lbs, at 172). Skin, brain fog, bloating, mm weakness, loose stools.
- Same:
- fatigue
- Worse:
- na
Lab interpretation:
- Aerodiagnostics Lactulose SIBO breath test
- H2 3, CH4 56
- Diagnostic Solutions GI-MAP stool test
- H: Klebsiella pneumoniae. Morgonella, Pseudomonas.
- B. hominis and D. fragilis
- Diagnostechs GI-15, Added in place of Quest#1 per Dr.R
- blasto H – few.
- Quest #2 blood & urine
- basics, additions WBC 2.7-L, UA PH -abnormal
- Vit D, 25-OH 34-WNL
- Dx:
- moderate CH4 (56) SIBO. DS: bacterial dysbiosis, Blasto. DT: Blasto.
- Summary
Impression:
- 7/12/17 – Colin’s SS started post Abx making dysbiosis highly suspected which was confirmed today; bacterial dysbiosis, SIBO, blasto. He has responded well to monolaurin and probios previously so should do well with Habx if needed. No other ddx to mind, but consider histamine intolerance. Today has responded very well to MF, Paleo LF, initial program; all SS improved except energy. Will continue with the current plan and then fu in 1-3 months to determine if Habx is needed and/or consider retesting previously found EBV reactivation.
Recommendations:
- Continue with the current plan
- Continue to intermittent fast periodically using the modified fast
- Follow up in 1-3 months
Visit 4
Subjective Assessment:
- has been regressing slightly, then dc all probios and went back to normal.
- Improved:
- All CCs
Impression:
- 8/23/17 – Colin has maintained improvements and all CCs have responded. Probiotics caused a reaction, he then stopped and reaction abated. Today have him start dietary reintro, then perform program wean. Will fu if/when needed for regression or yearly checkup. Retesting not required at this point.
Recommendations:
- start the reintroduction of non-low FODMAP foods
- once you feel stable with this wean off the items in your program
- Follow up: as needed or for yearly check in
Dr. Ruscio’s Comments
I have been openly critical regarding the utility of testing, seeing the value but arguing the perceived value is in far excess to the actual value. This case perfectly illustrates this. A major takeaway from this case is, consider reserving testing for those cases that have not responded to preliminary therapies. How we define preliminary therapies is open for interpretation, but I feel 2-3 diet trials and probiotics to be highly tenable.
Here is another thought that some might consider heretical, but I am growing progressively more confident in
When running 2 high-quality stool tests at the same time, the results disagree the majority of the time. If the best testing we have is inconsistent, perhaps stool test results should NOT be looked at 100% literally, but rather used to establish the theme of gastrointestinal dysbiosis. Once this is established, the clinician can experiment with the available array of dysbiosis treatments empirically until the clinical endpoint is reached. This makes the utility of serial retesting to guide treatment unnecessary, which is usually welcomed by both patients and clinicians as it allows them to focus time and money on treatment. Retesting can be used, judiciously, to confirm an objective endpoint has been reached, or to guide treatment in recalcitrant cases.
In this case, as in many, the overlap between tests is minimal and was only seen in the Blasto. Additionally, there was no need to directly treat lab results but rather we were able to resolve Colin’s symptoms by using one of the most preliminary treatments for dysbiosis, probiotics. Another key takeaway is that probiotics are not a good long-term therapy for some patients. For some, probiotics work well for a few months, then start to cause reactions. My thinking here is in the short-term probiotics help to combat dysbiosis (amongst other things) then once the benefit has been achieved, continued use of probiotics leads to an oversaturated of the gut lumen with these transient organisms and thus leads to a regression. Another reason to always be working to the minimal effective dose.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!