Practitioner Case Study – April 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
- Menopause, Libido, Depression, Constipation and Reflux Improved with Dietary Changes and HRT– Guest Case Study by Dr. Anna Cabeca
Research
- Methodology and Indications of H2-Breath Testing in Gastrointestinal Diseases: the Rome Consensus Conference
- A Systematic Review and Meta-Analysis of Interval Training Versus Moderate-Intensity Continuous Training on Body Adiposity.
- Measurement of Hydrogen Sulfide During Breath Testing Correlates to Patient Symptoms
Practitioner Question of the Month
Practice Tip
![]()
Case Study
Patient Info
- Carlene, 48yo, female, G2, Po
- Previous dx: history of Hodgkin’s disease, breast cancer with left mastectomy, surgical menopause, and hypothyroidism
- Chief Complaints:
- menopausal symptoms
- decreased libido
- inability to have an orgasm
- vaginal pain and dryness
- mood changes
- hormone imbalance
- depression
- constipation
- reflux
- to quote “She can’t remember ever feeling great.”
Visit Number One
Carlene presents as a generally healthy, quite educated female who has a good diet and lifestyle which includes running and managing her own business. She has experienced gradual progression of her complaints over the past several years, again not remembering the last time she felt well. At age 26 she was diagnosed with Hodgkin’s lymphoma and underwent radiation therapy. In 1998, at age 34, she was diagnosed with breast cancer stage III.
Past medical history is further significant for recurrent yeast infections and urinary tract infections, thyroid disease, depression, uterine fibroids, ovarian fibroids, DVT, and factor V Leiden. She also reports being sick a lot as a child as well as binge eating.
Her medications include Prilosec 10 mg, Wellbutrin 150 mg, and levothyroxine 0.15 mg.
Her past surgical history is significant for a TAH/BSO at age 37. Her appendix, tonsils, and a dermoid have been removed. She had a left mastectomy at age 34 and breast reconstruction following. Her family history is significant for substance abuse, depression, and diabetes.
Social history: She is married. She has a dog and a horse she loves. She is a licensed professional counselor and has a history of sexual abuse as a child. No T/E/D.
On physical examination, she is 5 foot 4 inches tall, 160 pounds, with a BMI of 27, blood pressure of 100/64, and pulse of 82. Of significance on breast examination: right breast with fibrocystic breast disease, left mastectomy scar, and pale nipples. Abdominal exam: slightly distended gaseous abdomen. Pelvic exam reveals pale vulvar and vaginal tissue, atrophic vaginitis, diminished clitoris, and decreased sensitivity.
Initial impression
Carlene is a 48-year-old woman with a high risk for recurrent malignancy, struggling with GERD, depression, and hypothyroidism, and is essentially living as if “waiting for the next shoe to drop”. Wondering “when will the next diagnosis happen?’
My Seven Key Areas of Assessment
- Mental-Emotional: Dealing with depression, fear, and probable PTSD from the cancer diagnosis, history of sexual abuse. Plan: Reframe goals, positive verbiage, gratitude journaling.
- Nutrition: Issues include chronic constipation and multiple medications. Again, a modified elimination diet includes a 72-hour protein fast, probiotic, added fiber, and a multivitamin-mineral combination along with Mighty Maca for adrenal support and detoxification support.
- Digestion: Long-term Prilosec usage. Will need to wean off that during the detoxification program and add digestive enzymes to tolerance.
- Detoxification: Considering her cancer history and multiple medical problems as well as fatigue, this is an area that needs additional phase 1 and phase 2 support. Add detoxification support supplementation, again, the modified elimination diet, and assess results in three to four weeks.
- Hormones and Hormonal Balance: She is surgically menopausal since age 34, not on hormone replacement therapy with the exception of levothyroxine for hypothyroidism. Literature on the benefits/risks of progesterone and/or DHEA therapy and testosterone therapy in women with a history of breast cancer provided. Run full blood panels, assessing hormones.
- Sexual Health: Consider significant loss of libido and, per client, “can’t recall her last orgasm”. Will address this with regaining health and again, discuss the consideration of androgen therapy such as testosterone and/or DHEA as well as my program Sexual CPR, starting with the webinar Help Doctor, My Sex Drive Has No Pulse. This is an issue in her marriage and she would like some solutions.
- Inflammation in the Environment: Discussed with Carlene potential toxic agents that are in her environment including makeup, cosmetics, cleaning products, the environment in which she works, emotional or chemical toxins, as well as assessing her environment which she has control of and being able to remove any inflammatory substances and any endocrine disruptors. She was instructed to begin to modify the elimination diet and return back in three to four weeks.
Visit Number Two: Three Weeks Later
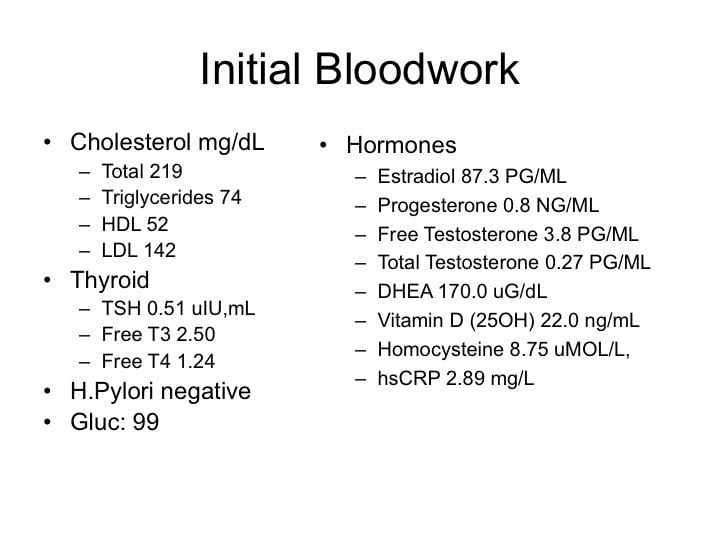
Testing results revealed a cholesterol total of 219, triglycerides 74, HDL 52, LDL 142, thyroid showed TSH of 0.51, free T3 of 2.5, free T4 of 1.24. Her H. pylori was negative. Glucose was 99. Hormones showed estradiol 87.3 pg/mL, progesterone 3.8, total testosterone 0.27 pg/mL, DHEA 170.0, vitamin D 25-hydroxy 22.0, homocysteine 8.75, and hs-CRP 2.89.
Recommendations
Continue with the modified elimination, proceed with a 72-hour protein fast using only our detoxifying cleanse shake and alkaline broth as needed for 72 hours. Nutritional support: include Mighty Maca Greens, and progesterone pregnenolone cream at 20 mg progesterone, 10 mg pregnenolone, apply at bedtime nightly to start days 1 through 26 each month.
Visit Number Three: One Month Later
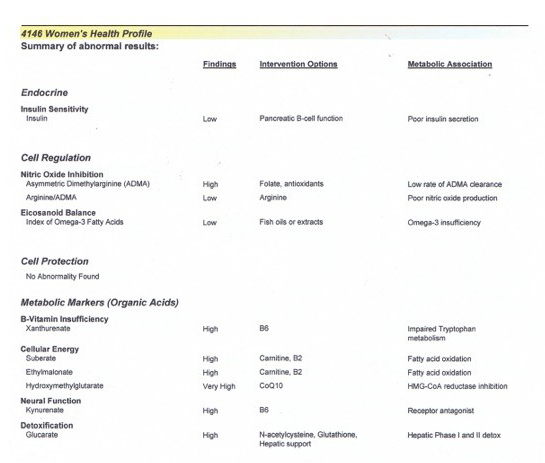
She had lost 6 pounds, now 154 pounds. Happy with that, however, during her detox, she had significant gastrointestinal upset, so we added digestive enzymes, fiber, and phase 1 and 2 detoxification nutrient support. Ordered the follow-up testing including nutritional assessment with the Women’s Health Profile by Metametrix which included fatty acid assessment as well as organic acids and estrogen detoxification assessment, which was low. Based on this, we added CoQ10, arginine, probiotic, carnitine, and glutathione. Her reflux and gastrointestinal symptoms had improved on the modified elimination diet. She no longer needed Prilosec.
Impression
Her hormonal symptoms had significantly improved. She was now getting a good night’s sleep and waking up rested. Having more energy. Constipation had also improved as well as her overall mood. Overall, Carlene is moving in the right direction.
Visit Number Four: Three Months Later
Subjective assessment improved. Carlene had significantly improved overall and continued to lose weight. She was now 141 pounds, a total of 19-pound weight loss. Her BMI was 24.2 and her blood pressure 120/60. Her vaginal health was significantly improved. Her relationship was improved and she had her first orgasm in years. Additionally, she finished her PhD thesis and began an equestrian therapy center, something she had always wanted to do. Of note, at her prior visit we did begin oxytocin 10 IU sublingual daily as needed not to exceed 50 IU, can use up to 50 IU prior to intercourse.
Visit Number Five: Six Months Later
Carlene had lost over 30 lbs and had weaned herself off of Wellbutrin.
Dr. Anna Cabeca’s Comments
When Carlene first came into my office I knew she was spiraling downward fast. I often can tell by the look on a patient’s face. She had been waiting for the next shoe to drop, would I be giving her another diagnosis? But I worked with her to get her back in control of her health and her life with the detox, M.E.D. and education programs that help (womensrestorativehealth.com) and key data points that show her that it’s not in her head. This is where functional testing really has so much utility because standard serum testing can fall short of detecting these underlying nutritional insufficiencies that can really compromise life. As well doing hormone testing and being able to see and coach appropriately and balance hormones, which can make a huge difference, especially in someone who has had a history of cancer as well as surgical menopause. The consequences are physically, mentally, and emotionally damaging.
With careful intervention in a compliant patient who’s willing to take a head-to-toe approach as Carlene was, we were able to get excellent results very quickly and maintain these results throughout the years. When using hormone therapy in a client with a history of breast cancer, consent is really important, even when we are using such low dosages of topical progesterone and pregnenolone and testosterone and / or DHEA. However, there is growing good research performed by Dr. Rebecca Glaser looking at testosterone therapy in clients with breast cancer having decreased recurrence as well as improved quality of life as well as using vaginal DHEA as with Dr. Labrie’s research. This was critically important for Carlene, who was just slowly dying, and in this short time period was able to take control of her life and fulfill a dream including her PhD in psychotherapy as well as beginning an equestrian therapy center.
I do want to note that I used oxytocin therapy based on my questionnaire and clinical impression as well as for a short-term boost for her during this initial transition period. Between the oxytocin, the testosterone, the progesterone, and clarity from a modified elimination diet, she was able to reconnect in her most intimate relationship, with her husband, in a way that she hadn’t in years. This forged a good foundation to continue to grow in health physically, mentally, emotionally, and relationally.
It’s emphasized to her that she must maintain a very strict gluten-free dietary program, to continue quarterly 72-hour protein fasts or water fasts or a quarterly detox regimen so that she stays on track. Genetic testing in this client could be quite useful, but definitely, a complicated next step considering she had excellent results and went from a 50 to a 5 on my hormone symptom review of systems checklist. She was doing quite excellent.
Currently, six years later, she has a daily protein shake (currently my keto-alkaline 0-gram sugar protein shake), one to two scoops of Mighty Maca five days a week, Julva® vulvar cream, PuraBalance PPr cream at night, multivitamin and minerals including additional magnesium, vitamin D 5000 IUs to maintain her vitamin D 25-hydroxy in the high 60s to 80 range with vitamin K2. She continues to be gluten free and dairy free, as that also revealed to be a sensitivity. She maintains her Nature-Throid and no longer is on Prilosec or Wellbutrin.
She no longer lives as if waiting for the next shoe to drop or the next diagnosis to be made. Her equestrian therapy center has grown in fame in our region and is called LightHorse Therapy Center.
Dr. Ruscio’s Comments
As you may or may not know, many women struggle with menopausal hormonal changes and its consequences.
Emory University trained Gynecologist and Obstetrician and colleague of mine, Dr. Anna Cabeca, has created an effective and natural product to help balance menopausal changes. Julva is a feminine cream with DHEA for the vulva.
Julva addresses vaginal and vulvar dryness, and discomfort during sexual intercourse. Many clients also report improved incontinence symptoms.
Many medical providers are now carrying Julva in their offices and their patients are benefiting from it. It is a great option for many women.
Please enjoy a free 7 day trial of Julva. Get it here.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!