Practitioner Research Review – April 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- Methodology and Indications of H2-Breath Testing in Gastrointestinal Diseases: The Rome Consensus Conference
- A Systematic Review and Meta-Analysis of Interval Training Versus Moderate-Intensity Continuous Training on Body Adiposity
- Measurement of Hydrogen Sulfide During Breath Testing Correlates to Patient Symptoms
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Methodology and Indications of H2-Breath Testing in Gastrointestinal Diseases: The Rome Consensus Conference
https://www.ncbi.nlm.nih.gov/pubmed/19344474
Study Purpose
- Generate a consensus position regarding breath testing in gastrointestinal disease.
Intervention:
- The Rome Foundation is one of the leading bodies in gastroenterology in the world. They convened a panel of experts to generate a consensus regarding breath testing. Specifically, a panel of 25 experts worked to generate a consensus, that was then voted on and modified by a panel of 26 different expert ‘jury’ members.
- Note: there is a lot here. If you are new to this I would read the “author’s conclusion”, “clinical take away” and “Dr. Ruscio’s comments” sections first.
Main Results:
GENERAL REMARKS
- H2 production is normal in the colon but, when certain conditions are present, can lead to SIBO and thus H2 production in the small intestine.
- In normal conditions, H2 production occurs in the colon by resident microflora, but in patients with predisposing conditions leading to small bowel bacterial overgrowth, H2 production may also occur in other gut segments.
- “the measurement of H2-breath concentration may be considered an expression of intestinal H2 production.”
- A high baseline gas reading may indicate oral dysbiosis.
- Oral cavity cleansing aimed at the inactivation of bacterial flora thus prevents the increase in an early peak of breath hydrogen excretion, which may cause false positive results.
- Some people will produce no hydrogen. Methane testing could be used to identify overgrowth in these subjects, however, the Rome Foundation does not feel we have adequate data to support CH4 testing yet.
- The reported prevalence of such H2 nonproducing subjects harboring colonic flora unable to produce hydrogen during fermentation varies widely from 2% to 43%.
- On the contrary, in subjects who are definitely hydrogen nonproducers, breath methane could represent an alternative marker. Unfortunately, up to now we have no conclusive data as few pediatric papers are available and studies in adults show contradictory results.
- CO2 levels are important to ensure SIBO breath testing collection was performed correctly.
CARBOHYDRATE MALABSORPTION
Summary:
- “lactose breath tests may be suggested in clinical practice following a standardized technique, while fructose and sorbitol tests should be proposed only for research studies”
SMALL INTESTINAL BACTERIAL OVERGROWTH
Summary:
- “Small intestinal bacterial overgrowth (SIBO) is an intestinal microflora unbalance, which can show a wide clinical spectrum ranging from a mild and unspecific intestinal symptoms to a severe malabsorption syndrome.”
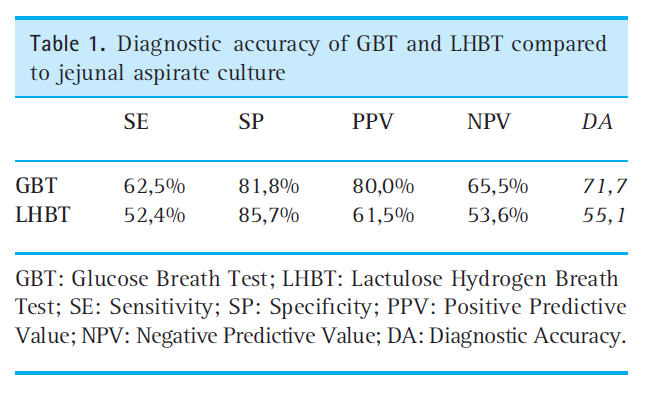
- “The culture of jejunal aspirate is considered the gold standard diagnostic test for SIBO, however, glucose and lactulose breath tests (GBT and LBT) are currently used in clinical practice. Among them, GBT seems to have a higher diagnostic accuracy in studies comparing breath tests versus culture.”
- “Some conditions, such as hypoaclorhydria, anatomical abnormalities or gastrointestinal motility failure, may cause SIBO and related malabsorption. In these cases, GBT may be useful in order to establish whether malabsorption is due to SIBO or to the underlying disease.”
- “Data about the role played by SIBO in irritable bowel syndrome are still inconclusive, and its search by breath test is not recommended in these patients.”
- “Measurement of breath methane excretion is not currently recommended to improve the diagnostic accuracy of the hydrogen breath test.”
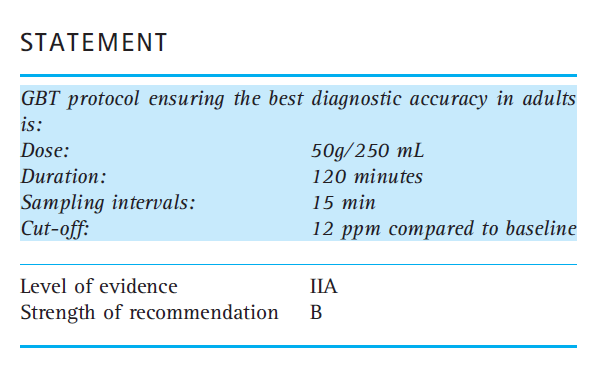
- Rome offers the following guidelines for glucose breath testing:
Additional Notes – SIBO
- Rome criticizes Pimentel’s finding regarding the 78-84% connection between SIBO and IBS. Rome concludes that a 30-46% occurrence of SIBO in those with IBS compared to only 4% in healthy controls is more accurate.
- Subsequent studies, based on GBT for SIBO diagnosis, confirmed a correlation between SIBO and IBS. In fact, the prevalence of SIBO in patients with IBS fluctuated between 30% and 46%, as compared to 4% in healthy controls.
- They continue that when other testing methods are used to assess SIBO, the incidence of SIBO in those with IBS is essentially the same as it is in healthy controls.
- In recent studies, the prevalence of SIBO in patients with IBS, tested with different diagnostic techniques, was shown to be rather low and not significantly different from that of healthy controls.
- SIBO diagnosis based on the culture of duodenal juice was performed in only 4% of IBS patients and BT positivity was similar in IBS patients and in healthy controls.
- They conclude that even though it’s likely that bacteria play a role in IBS, due to these inconsistencies in the data, SIBO breath testing cannot currently be recommended.
- In summary, although it is likely that the intestinal bacterial flora plays a role in the pathogenesis of IBS, the lack of data uniformity currently present in the literature makes it impossible to clearly identify a correlation between IBS and SIBO. Therefore, BTs for SIBO in patients with IBS are not recommended.
- And Rome then summarizes:
- In clinical practice, some conditions, such as hypoaclorhydria, anatomical abnormalities or gastrointestinal motility failure, may cause SIBO and related malabsorption. In these cases, it could be difficult to establish whether malabsorption is due to SIBO or the underlying disease. GBT is a useful, non-invasive and inexpensive test to evaluate the role played by SIBO in these clinical conditions. The diagnostic accuracy of BTs is quite good, even if the results of these tests should be interpreted with caution, always taking into account the patient clinical history.
- Even the gold standard for SIBO testing (duodenal aspirates) is not perfect and suffers from lack of standardizations and questions regarding accuracy. How to identify distal SIBO is one shortcoming of this methodology.
- The amount of liquid, the site of collection (traditionally beyond the ligament of Treitz) and the technical details of the microbiological tests (for both aerobic and anaerobic bacteria), as well as the cut-off value for definition of SIBO are not yet standardized, although many studies use a value of >105 CFU ⁄ mL.
- Besides these methodological problems of standardization, a still unsolved issue concerns the diagnostic accuracy of the culture in case of ‘distal’ SIBO, that is bacterial overgrowth affecting mainly the ileum, which is not assessable by means of traditional enteroscopy.
- 2 types of SIBO may exist from 1) upper respiratory tract bacteria due to deficient stomach acid/barrier, 2) colonic bacteria due to altered clearance and/or motility.
- In fact, two types of SIBO are identified on the basis of pathophysiological mechanisms.
- The first type is predominantly supported by Gram-positive bacteria from the upper respiratory tract, and is secondary to a deficiency in gastric acid barrier.
- The second type is characterized by an increase in colonic bacteria, and may occur in individuals with altered intestinal clearance or with abnormal communication between the large and the small bowel.
- SIBO breath testing is not perfect because of the potential for false positive and false negative results.
- Moreover, in case of LHBT, the early ‘small bowel’ H2 peak can merge with the late ‘colonic’ peak, while a quick glucose absorption into the proximal bowel may result in a false negative GBT. On the other hand, false positive H2-BTs have also been reported in individuals with an accelerated intestinal transit time.
- The following table provides a summary of study findings comparing glucose or lactulose testing to aspirates
- The glucose breath test has been found more accurate than the lactulose breath test. Note: I have reviewed this previously came to the same conclusion (1)
- Overall, regardless of the substrate dose and the test duration, GBT has shown a greater diagnostic accuracy than LHBT. Besides being accurate and non-invasive, H2-BTs have other advantages such as lack of toxicity, low cost of substrates and easy accessibility to clinical practice (for the wide diffusion of gas-chromato-graphic devices).
- Rome’s glucose testing recommendations:
- Glucose 50 g ⁄ 250 mL; 120 min. Or,
- Glucose 75–100 g (in different concentrations); 180 min.
- The diagnostic accuracy is around 70% for both tests. Theoretically, the use of a glucose dose greater than 50 g and a longer test length can also explore the distal segments of the small intestine, thus increasing the diagnostic accuracy of ‘distal’ SIBO. However, 75–100 g GBT did not show a significant improvement in sensitivity as compared to 50 g GBT.
- The most frequently used cut-off value for test positivity is 10–12 ppm.
- The higher dose of glucose may be able to make it all the way through the small intestine and reach the large intestine. This combined with a longer test may assess distal SIBO. This theory does not appear to be proven yet.
- Theoretically, the use of a glucose dose greater than 50 g and a longer test length can also explore the distal segments of the small intestine, thus increasing the diagnostic accuracy of ‘distal’ SIBO. However, 75–100 g GBT did not show a significant improvement in sensitivity as compared to 50 g GBT.
ASSESSING ORO-CAECAL TRANSIT TIME (OCTT)
Summary
- “The appearance in the expiratory breath of gases produced by colonic fermentation of an ingested organic compound may be used to measure oro-caecal transit. Both a liquid meal containing lactulose or a solid meal containing baked beans can be used in the assessment of oro-caecal transit. Ingestion of a meal is followed by a biphasic breath hydrogen profile in most subjects. The initial peak of hydrogen closely follows the meal whereas the second peak, associated with the head of the meal entering the caecum often occurs hours later. “
- “The H2 breath test is safe and usually well tolerated. However, the wide variation in the measurement of oro-caecal transit in normal subjects and the poor reproducibility of the test, in particular with the liquid meal, have limited its applications to the clinical realm. The test performance is better when applied to clinical pharmacology studies and it has been used to demonstrate the drug effects on oro-caecal transit.”
Additional Notes – oro-caecal transit time (OCTT)
- Elevated baseline values on breath tests may indicate oral dysbiosis, which can be remedied by mouthwash (chlorhexidine). Higher levels of elevated baseline may be from food residue at the IC junction.
- Carbohydrate fermentation by bacteria in the mouth may account for the initial peak and may be prevented by mouthwash.
- Larger initial peaks are probably caused by residues entering the colon from a previous meal stored in the ileum and propelled by test meal ingestion, a manifestation of the gastro-ileal reflex.
- The oro-caecal transit time ranges from 40-170 minutes. Note: this is part of what makes interpreting SIBO breath testing a challenge and thus why it is important to never make decisions based on test results only.
- The oro-caecal transit time in healthy subjects ranges between 40 and 170 min for lactulose meal.
- Roughly 5-25% of normal subjects will NOT see an increase in hydrogen in the colon. Note: this is important because sometimes labs will say the test needs to be repeated if an increase in gas is not observed in the colon, however, this does not appear to be the case.
- About 5–27% of normal subjects fail to produce an increment of hydrogen breath concentration after the meal due to the absence of hydrogen-producing flora in the colon.
- An increased OCTT has been observed in a number of conditions.
- A delayed oro-caecal transit assessed by hydrogen-breath test has been reported in various sub-groups of patients, including those with depression, chronic alcoholism, constipation, acromegalics, diabetics, irritable bowel syndrome, beta thalassemia major, pregnancy, cholecystectomy, obesity, cirrhotics, scleroderma, dyspeptic patients, in the chronic phase of corrosive injury after acid or alkali ingestion, and in constipated children.
- A shorter OCTT has been observed in other conditions.
- By contrast, fast oro-caecal transit has been reported in patients with irritable bowel syndrome, chronic alcoholics, partial gastrectomy, post-vagotomy diarrhea and hyperthyroidism.
- After taking lactulose, the OCTT is 80 minutes on average. Note: this is likely why the North American Consensus Statement advised using a cut off time of 90 minutes for SIBO breath testing. This would attempt to consolidate the testing window to the average time interval of the small intestine (80 min) plus a 10-minute buffer.
- A liquid meal containing 10 g of lactulose in 100 mL of water is expected to give a mean oro-caecal transit time of about 80 min.
BREATH TESTING FOR GAS-RELATED SYNDROMES
Summary
- “Available data do not clearly prove that gas production and intestinal gas content in patients with ‘gas-related symptoms’ differ from controls.”
- “The prevalence of sugar malabsorption (lactose, fructose…) in IBS patients and gas-related symptoms is not higher than in the general population.”
- “Hydrogen breath tests do not provide clear evidence that increased gas production ⁄ excretion is present in patients with gas-related symptoms.”
Additional Notes – breath testing for gas-related syndromes
- “Salvioli et al. showed that the small bowel is the main intestinal segment responsible for gas retention.” “However, the correlation between the volume of retained gas and the severity of abdominal bloating was poor, suggesting other factors, such as visceral hypersensitivity.”
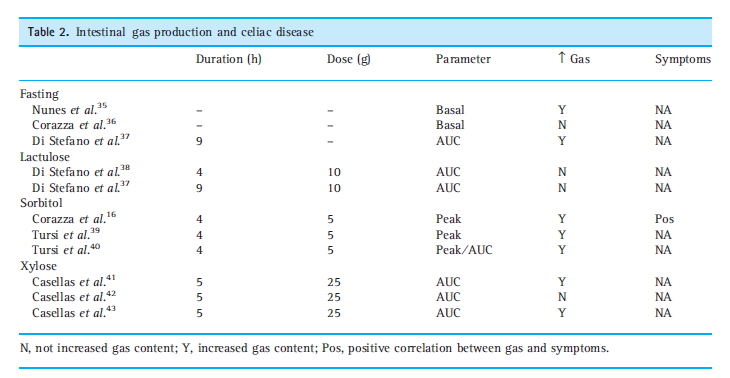
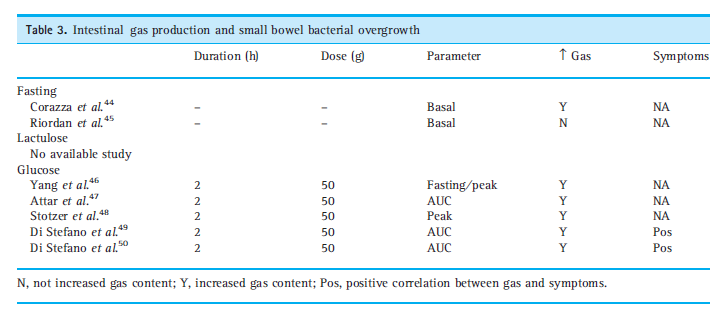
- Various disease conditions do show a higher level of gas production than compared to healthy controls.
- In Table 2 and 3, data on AUC in different diseases are reported, showing that in the majority of the available papers, AUC calculated in patients was significantly higher than in healthy volunteers.
- The Rome Consensus cautions that the above data regarding gas levels are not high quality and therefore the connection between gas levels and symptoms is debatable.
- Thus, any attempt to derive reliable information on the accuracy of breath test in gas-related symptoms in GI tract diseases is at best debatable.
Authors’ Conclusion:
- There is no one conclusion to this paper, but rather a number of conclusions regarding the various aspects of breath testing. Here are the most relevant:
- Rome does not condone:
- methane breath testing
- fructose or sorbitol breath testing for carbohydrate malabsorption
- lactulose breath testing for SIBO in those with IBS
- breath testing for gas-related disorders, even though some data do show increased production in gas-related disorders, the data here are too inconsistent/low quality
- Rome supports
- lactose breath testing for carbohydrate malabsorption
- glucose breath testing for SIBO, but only for those with conditions predisposing one to malabsorption such as hypochlorhydria, anatomical abnormalities or gastrointestinal motility failure
- For the glucose-SIBO breath test, they recommend a cut off of 10-12 ppm. Using 50 g of glucose in a 120 min test
- Rome feels the diagnostic value of glucose breath testing is “quite good” but also that the results should be interpreted with caution and should be looked at in the context of the patient’s clinical history – in part to guard against a false +/- result
- Rome feels bacteria likely do play a role in IBS
- Rome does not condone:
Interesting Notes:
- Smelly flatulence has a high correlation with hydrogen sulfide production.
- Recent studies have shown that sulphur-containing compounds, like hydrogen sulphide, dimethyl sulphide and methanethiol, are mainly responsible for the unpleasant smell of human faeces. In particular, hydrogen sulphide was the predominant sulphur gas in 78% of samples and the concentration of this gas has the strongest correlation with odor.
- “Unlike CO2, bacterial metabolic processes represent the only source of H2 and CH4 in the bowel”
- Prebiotics may exert their benefit in IBS and SIBO by acidifying the GI tract and thus decreasing gas production. Note: prebiotics can help some with IBS/SIBO but they can also cause reactions.
- It has been shown that acidification of stool pH by ingestion of a nondigestible sugar, such as lactulose, decreases H2 production, this condition is overcome by MgSO4 pre-treatment and consequent increase in colonic pH.
- Low H2 levels may occur if CH4 overgrowth is present as CH4 organisms consume H2.
- Strocchi et al. demonstrated that both increase in number or activity of methane-producing bacteria, and high fecal H2 tension can be responsible for the rise in H2 consumption.
- Laxatives and enemas can be used as a method to reduce hydrogen.
- It has been demonstrated that a combination of laxatives and enemas depresses hydrogen production very markedly.
Clinical Takeaways:
- This is challenging because the North American consensus paper and the Rome Foundation consensus paper come to very different conclusions. But here are a few thoughts I feel to be most relevant.
- SIBO breath testing can be helpful but is not perfect, therefore testing should be looked at as one part of the decision-making process. A patient’s history and symptoms are equally, if not more important to consider.
- False positive and false negative testing results can occur, so avoid only ‘treating the tests’. Also, be cautious in definitively diagnosing someone with SIBO if they have little to no symptoms.
- Which is a better test, glucose or lactulose? I believe there is a case to be made for either. I am currently researching a few details here and will report back with any noteworthy findings.
- Gas appears to play a role in IBS and in other gas-related syndromes, but the exact role is still unclear.
- Smelly flatulence may indicate hydrogen sulfide SIBO.
- Oral dysbiosis may cause some cases of the elevated baseline on SIBO breath testing.
- Some people produce no hydrogen.
Dr. Ruscio Comments
The Rome Foundation’s statement is good to be aware of. I fear some SIBO circles have become overzealous with SIBO testing and with how much is drawn from test results. This can lead to overtreatment, over testing, unfounded fear and increased expense.
Over the past 2-3 years, I have been using the testing less. I used to test, treat, retest and repeat until patients reached improvement. However, after doing this for a while plus thinking and reflecting I have updated my approach. What I usually do now is test to get a baseline, in patients who have already taken some initial steps toward gut health but have not achieved optimal response. Specifically, this usually means they have tried at least one diet and/or one type of gut healing intervention like probiotics (if someone hasn’t done this we might forgo any/all testing and simply start with these basics). Then we:
- Treat until an optimal symptomatic response is achieved – once this is achieved there is optional confirmatory retesting.
- If optimal symptomatic improvement is not achieved – we retest to see how their SIBO status correlated with their current condition to guide future treatment.
This approach seems reasonable as it is as effective as a more testing heavy method (in my observation), but I would argue produces results faster (less time is allocated for retesting) and cheaper (less testing expense is incurred).
I mostly use lactulose because I fear missing distal SIBO. However, I use this test cautiously and with a cutoff time of 80-100 minutes to guard against false positive results. I have some unanswered questions comparing a shorter time window lactulose test versus a higher dose/longer window glucose test. I am currently looking into this and if I uncover anything here that changes my opinion I will report back.
A Systematic Review and Meta-Analysis of Interval Training Versus Moderate-Intensity Continuous Training on Body Adiposity.
https://www.ncbi.nlm.nih.gov/pubmed/28513103
Study purpose
- To assess if high-intensity (HIIT) or sprint interval training (SIT) was more effective for fat loss than traditional cardio (moderate intensity continuous training, MICT).
Intervention:
- A meta-analysis of studies that were a minimum of 4 weeks in duration. Of the 6,074 studies found, 31 were included.
Main Results:
- SIT/HIIT produced comparable reductions in body fat as MICT.
- Within-group analyses demonstrated reductions in total body fat (%)
- HIIT/SIT: -1.26
- MICT: -1.48
- and fat mass (kg)
- HIIT/SIT: -1.38
- MICT: -0.91
- There were no differences between HIIT/SIT and MICT for any body fat outcome
- Within-group analyses demonstrated reductions in total body fat (%)
- HIIT/SIT does not appear to provide the same results in less time, but rather HIIT/SIT provides similar results when using a similar time and energy expenditure is used.
- For body fat reduction HIIT/SIT is an effective alternative to MICT and achieves equivalent levels of fat loss when similar time commitment and/or energy expenditure is used.
- HIIT/SIT provides a better impact on cardiorespiratory fitness, blood pressure, insulin sensitivity and/or muscle mass.
- HIIT/SIT can therefore be advocated particularly when cardiorespiratory fitness, blood pressure, insulin sensitivity or muscle mass improvement is a primary target (15,16,18).
- If utilizing a short session of HIIT/SIT than MICT, it appears that MICT might be better for body fat reduction.
- Secondly, whether HIIT/SIT is an effective ‘time-efficient’ exercise strategy for body fat management remains contentious. To the contrary, we observed a near-significant superiority of MICT over HIIT/SIT when HIIT/SIT training time and/or energy expenditure was less
- Neither HIIT/SIT nor MICT on their own resulted in clinically meaningful reductions in body fat.
Additional Results:
- Interval training compared to “cardio” (MICT) appears to elicit time-efficient and superior improvements in aerobic fitness, ventricular and endothelial function, insulin sensitivity and blood pressure.
- The health benefits of interval training have been reviewed in detail elsewhere (13–16). These studies clearly show that compared with traditional moderate-intensity continuous training (MICT), interval training is a potent and time-efficient strategy for eliciting superior improvements in aerobic fitness (13,14,16) and ventricular and endothelial function in patients with cardiovascular disease (15,17) and leads to greater or comparable improvements in insulin sensitivity (16) and blood pressure (18).
- SIT training may be the only form of the three to lead to reduced calorie intake
- Comparable effects of HIIT/SIT and MICT on appetite perceptions (including hunger, fullness, satiation and desire to eat) have been demonstrated in men (79,80) and in children (81) with no differences in ad libitum energy intake between HIIT and MICT (80–82), but significantly less with SIT than MICT.
Authors Conclusion:
- “Analyses comparing MICT with HIIT/SIT protocols of lower time commitment and/or energy expenditure tended to favor MICT for total body fat reduction (p = 0.09).
- HIIT/SIT appears to provide similar benefits to MICT for body fat reduction, although not necessarily in a more time-efficient manner.
- However, neither short-term HIIT/SIT nor MICT produced clinically meaningful reductions in body fat.”
Interesting Notes:
- “Overall, it appears that EPOC is unlikely to account for any apparent greater fat loss potential with HIIT/SIT.”
- SIT was defined as
- This is defined as ‘all-out’ sprints (>100% of the maximal rate, VO2max) interspersed with recovery periods. These protocols typically employ short bursts (8–30 s) of supra-maximal sprint efforts requiring a relatively large anaerobic contribution, which are approximately equivalent to those undertaken in running events of ~100–200 m or during explosive intermittent bursts during team sports. SIT is commonly employed in young and/or healthy populations and has been associated with a range of health benefits including large improvements in cardiorespiratory fitness (13). However, the safety and utility of SIT in clinical populations are yet to be established.
- HIIT training was defined as
- This classifies protocols targeting intensities between 80% and 100% peak heart rate or aerobic capacity. HIIT is sometimes called aerobic interval training, and protocols typically employ bursts of activity lasting between 60 and 240 s, which are within the aerobic capacity of the individual (sub-maximal), but extremely strenuous. For most individuals, this may equate with an intensity that, if undertaken without rest, could otherwise be sustained for ~5–10 min before fatigue. The intermittent nature allows enough recovery for multiples of these efforts to be accumulated.
- MIT (“cardio”) was defined as
- This describes ‘traditional’ exercise protocols performed continuously at a steady state for a set duration (usually 20–60 min). Moderate-intensity activity is defined as an intensity that elicits a heart rate response of 55–69% HRmax or elevates the rate of oxygen consumption to 40–59% of VO2max (27)
Clinical Takeaways:
- HIIT/SIT does not appear to offer better body fat reduction in less time.
- HIIT/SIT appears comparable to MICT for body comp when using similar time and energy commitment programs.
- HIIT/SIT offers better results for cardiorespiratory fitness, blood pressure, muscle mass, insulin senility and ventricular and endothelial function.
- Using HIIT/SIT in shorter duration or lower energy expenditure program than MICT may lead to inferior reductions in body fat.
- None of these forms of exercise produced a clinically meaningful reduction in body fat.
Dr. Ruscio Comments
It appears HIIT/SIT is not the ‘time saving with better results for fat loss’ type of programming it is sometimes espoused to be. However, HIIT/SIT does produce better results in a number of other important parameters like blood glucose, blood pressure, endothelial function and muscle mass.
Bottom line, if you can get people doing some HIIT/SIT this should make them healthier than people who are only doing traditional cardio, but it won’t produce any measurable difference in body fat. With exercise, pick your battles. It’s better to get someone doing something they enjoy consistently than someone follows ‘the ideal program’ inconsistently. So, don’t be overly idealistic.
Measurement of Hydrogen Sulfide During Breath Testing Correlates to Patient Symptoms
http://www.gastrojournal.org/article/S0016-5085(17)30993-9/abstract
Study purpose
- To determine the association of hydrogen sulfide (H2S) with patient symptoms
Intervention:
- 99 patients were assessed
- a breath test was administered using 10 g lactulose and 25 g fructose
- H2 and CH4 were measured via Quintron unit according to standard SIBO testing protocol
- H2S was assessed via Alphasense, Essex, UK
- patients filled out a questionnaire assessing gastrointestinal symptoms
- gas levels and symptoms were then compared
Main Results:
- H2S levels and symptoms correlated, specifically for diarrhea and fatigue.
- Using a sensitivity analysis, a significant relationship was seen between the level of H2S and specific symptoms.
- For diarrhea, AUC levels of H2S ≥ 6.0 were associated with greater severity of diarrhea (P=0.028, see table).
- The same cutoff was notable for a greater degree of fatigue in the high H2S category (P=0.035).
- Those with high hydrogen levels (H2) were more prone to have high hydrogen sulfide (H2S) levels. This counters what some believe, “a negative H2 test could indicate someone has only H2S instead”
- Interestingly, the H2 AUC was higher in the high H2S group (367±232 ppm) compared to the low H2S group (244±176 ppm) (P=0.02) consistent with H2 consumption to produce H2S by sulfate-reducing bacteria. Age and gender were not confounding variables in this analysis.
Additional Results:
- na
Authors Conclusion:
- “This is the first clinical examination of detectable H2S in human BTs in North America. H2S may be an important missing link to SIBO, as H2S is bioactive and like methane appears to be important in predicting clinical symptoms such as diarrhea and fatigue.”
Interesting Notes:
- na
Clinical Takeaways:
- Hydrogen sulfide SIBO has been documented and correlates with diarrhea and fatigue.
- Those with high hydrogen may be an elevated risk of hydrogen sulfide SIBO, contrary to prior thinking.
- Other research has shown antibiotic therapy can treat hydrogen sulfide SIBO. (2, 3)
Dr. Ruscio Comments
H2S SIBO is a good example of why treatment decisions should not solely be based upon lab data. Someone could have normal labs while they actually had undetectable ‘dysbiosis’ as H2S SIBO or even SIFO, and this is why lab testing should be viewed as only one data point in the decision-making process. While this study found H2 SIBO correlated with increased risk H2S SIBO, the study linked below did not find a correlation between +/- H2 SIBO and H2S SIBO – so the association of H2 to H2S SIBO is still to be determined.
This study validated that a +H2S breath test correlated with symptoms. Another study both correlated H2S breath testing to duodenal cultures AND found that treatment of H2S SIBO with antibiotics reduced H2S gas levels and this reduction correlated with symptomatic improvement. (4, 5)
I would presume that herbal antimicrobials would effect H2S SIBO, just as herbals have been documented to have an impact on both H2 and CH4 SIBO.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!