Practitioner Research Review – September 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Autoimmune/Inflammatory Syndrome Induced by Adjuvants and Thyroid Autoimmunity
https://www.ncbi.nlm.nih.gov/pubmed/28167927
Study purpose:
- To assess the impact of adjuvants (contained in vaccination) on thyroid autoimmunity.
Intervention:
- A review of the literature.
Main Results:
- There is limited data examining the link between vaccination and thyroid autoimmunity. A few case studies have been reported documenting thyroid autoimmunity post vaccination after influenza vaccination and H1N1 vaccination.
Additional Results:
- “The association between adjuvant exposure and autoimmunity manifests itself in five autoimmune conditions sharing similar autoimmunity manifestations (2, 3), such as the postvaccination phenomena, the macrophagic myofasciitis syndrome (MMF), the Gulf war syndrome (GWS), siliconosis, and the sick building syndrome (SBS) (4, 5).”
- These 5 conditions can be classified into one syndrome, the autoimmune/inflammatory syndrome induced by adjuvants (ASIA).
- “Extensive research has identified the genetic background, contributing to the development of ASIA syndrome in predisposed individuals following adjuvant exposure.”
- Risk factors:
- Several alleles of the HLA class II, such as DRB1 locus
- “When used in vaccines, adjuvants are purposely used as immunogenicity enhancing agents that are essential for directing the adaptive immunoresponse (9). However, they might also trigger undesired autoimmune reactions that question the use of adjuvants and their safety in the context of DRB1*01 genetic background (10).”
- R’s note: a personal or family history of autoimmune conditions may also increase risk
- Several alleles of the HLA class II, such as DRB1 locus
- A number of severe cases of ASIA have been reported post-vaccination with HPV, HBV, and seasonal influenza.
- “Despite vaccines’ proven record of safety and efficiency, aluminum hydroxide was used in these vaccines along with the viral antigens as an adjuvant.”
- “Genetically predisposed patients are more likely to exhibit late manifestations and are in a higher risk of developing ASIA syndrome.”
Authors’ Conclusion:
- There is little documentation for vaccination causing thyroid autoimmunity, but this is likely due to lack of awareness. Caution should be exercised regarding vaccination in genetically predisposed individuals.
- “Therefore, we believe that the minority of cases is not owing to rarity of association between adjuvants and AITD rather than the lack of awareness among physicians of such association. Consequently, physicians must be mindful that thyroiditis and other thyroid disorders can be induced by diverse adjuvants and therefore to reconsider non-essential vaccination in genetically predisposed individuals for autoimmune diseases.”
Interesting Notes:
- “…primary ovarian failure (POF) has been linked to ASIA, especially after vaccination (21–25).”
- “HPV vaccine has been reported as an important issue in ASIA syndrome, already being related, for instance, to Guillain-Barré syndrome and other neuropathies, such as SLE, vasculitis, ITP, and autoimmune hepatitis (32–36).”
- Vaccination-induced autoimmunity may not manifest for months or years.
- “Autoimmune well-defined diseases, as well as the non- specific immune disorders, following vaccination can present as a subacute vaccination side effect or appear months or years after the boosters (39–43).”
- Well performed trials have documented increased risk for development of other autoimmune conditions when the HPV vaccination was administered to subjects currently having an autoimmune disease.
- “… a cohort study with 211 young female patients with autoimmune diseases and 857 matched controls, they showed that patients exposed to quadrivalent HPV vaccine were in a higher risk of developing type 1-diabetes mellitus (OR = 1.2) (45).”
Clinical Takeaways:
- Vaccinations do have the documented effect of stimulating autoimmunity. Those with genetic risk (HLA class II, DRB1 locus, and family history) are at highest risk for vaccination-induced autoimmunity, and therefore caution should be advised. Caution doesn’t mean complete avoidance.
Dr. Ruscio’s Comments
The issue of vaccination may not be a dichotomous one, but rather an issue that requires identifying those at greatest risk of harm from vaccination and then making modifications for these patients. For infants and children, a vaccination plan that focuses on the most essential vaccinations administered at a delayed schedule seems reasonable. For adults, focusing on the most essential seems reasonable.
It’s also important to mention that the number of cases appears very low overall. We do know that infection is one initiator of autoimmune conditions. Since vaccination is essentially an attenuated/controlled infection, the link here is plausible. However, what I am unclear on at this moment (and what we may not know yet) is do vaccinations increase the prevalence of autoimmune conditions in at-risk populations, or do vaccinations merely make an AI that would eventually manifest, manifest earlier?
A definitive blood test for post-infectious irritable bowel syndrome?
http://www.tandfonline.com/doi/pdf/10.1080/17474124.2016.1242411
Study purpose:
- To establish if there is a reliable blood test for IBS.
Intervention:
- This study reviewed supporting literature to determine if the vinculin and CdtB antibody blood test is viable to establish IBS.
Main Results:
- IBS is, in part, caused by antibodies against vinculin and/or CdtB.
- “…suggesting that antibodies to the CdtB toxin were cross-reacting with a neuronal protein in the host gut. Through a series of studies, this was identified as the cytoskeletal protein vinculin.”
- Vinculin is a cytoplasmic actin-binding protein and an important component of focal adherens junctions (FAJ) and tight junctions, with roles in structural integrity and epithelial barrier formation 22.
- Significantly, C. jejuni-infected rats exhibited reduced vinculin expression in the small intestinal wall, and levels of antibodies to CdtB correlated both with the degree of loss of vinculin and with the development of SIBO in these animals 22.”
- Infection produces CdtB antibodies, which can cross react with intestinal tissue (vinculin).
- “This series of studies now supports a potential pathophysiologic pathway in the development of post-infectious IBS. Acute gastroenteritis with resulting systemic exposure to CdtB leads to positive seroconversion. Subsequently, homology between CdtB and vinculin leads to the generation of autoantibodies to vinculin.”
- The anti-vinculin and CdtB antibody blood test has been validated in diarrheal IBS to distinguish from other causes of diarrhea, like IBD and celiac.
- “These biomarkers were tested in a large-scale (180 center) study of subjects with IBS-D, comparing to subjects with celiac disease, Crohn’s disease, ulcerative colitis and healthy controls (23). These two biomarkers were found to be highly useful in identifying and distinguishing IBS-D from other causes of diarrhea. … a post-test probability of IBS of nearly 95% (23).”
- This test may suffer from a high level of false negative.
- “the sensitivity was below 50%”
- The test is most accurate for IBS-D, slightly less accurate for IBS-M, and not meaningful for IBS-C.
- “The results demonstrated that anti-CdtB and anti-vinculin titers had a statistically significant negative gradient from IBS-D to IBS-M, then to IBS-C and healthy individuals (p<0.001) (24). There was no statistical difference between antibody levels in subjects with IBS-C as compared to healthy individuals. Therefore, these biomarkers can be used to identify subjects with IBS-D and IBS-M, but not IBS-C (24).”
- “A positive test is seen in 56% of subjects with IBS-D, giving these patients a positive diagnosis. These patients would no longer need the additional testing to rule out other diseases required by the Rome criteria.”
Authors’ Conclusion:
- “… the newly discovered plasma biomarkers anti-CdtB and anti-vinculin are diagnostic for IBS-D and now IBS-M (but not IBS-C). The use of this test has led to IBS becoming a diagnosis of inclusion based on a pathophysiologic mechanism that includes post-infectious IBS and SIBO.”
Interesting Notes:
- “up to 50% of visits to gastroenterologists may be due to IBS”
Clinical Takeaways:
- Testing for vinculin and CdtB antibodies can be useful to establish the underlying cause of diarrhea and mixed-type IBS, and to prevent further testing for celiac and/or IBD.
Dr. Ruscio’s Comments
It’s important to note that this test was not validated for constipation-type IBS. In fact, a recent study showed that the vinculin and CdtB antibody test was not an accurate measure for constipation-type IBS https://www.ncbi.nlm.nih.gov/pubmed/28451914, which further supported the findings from this study.
The vinculin/CdtB antibody test appears useful for IBS-D and IBS-M. It can help prevent unneeded testing for celiac and IBD. However, there is also the question of what is the optimum treatment if someone has a positive test. Prokinetics are often suggested to be highly important in those with positive vinculin/CdtB testing, which I am open to. But, keep in mind that motility can repair all on its own as we reduce inflammation in the gut https://drruscio.com/sibo-can-recover/. Prokinetics may help, but other therapies like a low FODMAP diet, probiotics, and anti-bacterial treatment should also produce beneficial effects, in my opinion.
I mention this because it appears some providers are either a) confused as for how to treat the vinculin/CdtB findings or b) overly reliant on prokinetics. I am currently reviewing a study (write-up to follow) which may have shown that anti-bacterial treatment (Rifaximin) was able to reduce the vinculin/CdtB antibodies. If this is true, it will be important to keep in mind, because this would establish that prokinetics are not the only therapy that can help restore motility, but rather that a holistic approach to heal the gut may be the soundest approach.
Biochemical Testing of the Thyroid: TSH is the Best and, Oftentimes, Only Test Needed – A Review for Primary Care.
https://www.ncbi.nlm.nih.gov/pubmed/27231117
Study purpose:
- To review the utility of arguably the three most important thyroid tests: TSH, free T4 (fT4), and TPO.
Author’s Conclusion:
- “It is important for primary care providers to have an understanding of the shortcomings and proper interpretation of these tests to be better able to discuss thyroid function with their patients.”
Interesting Notes:
TSH, fT4, and fT3 Feedback Loops
- “…the relationship between these thyroid hormones and TSH is not linear but log-linear, such that very small changes in free T3 and/or free T4 will result in very large changes in TSH.”
- TSH fluctuates dramatically to maintain normal fT4 levels, thus, according to this paper, it is a better assessment tool for thyroid status as it is far more reactive/sensitive.
- “…a 2-fold change in free T4 will result in a 100-fold change in TSH.
- Thus, a free T4 change from 1.0 ng/dL to 0.5 ng/dL will result in a TSH rise from 0.5 mIU/mL to 50 mIU/mL.
- On the other hand, a rise in TSH from 1.0 mIU/mL to 5.0 mIU/mL reflects a drop in free T4 from 1.0 ng/dL just 0.9 ng/dL.”
- We may not want to overreact to small changes in TSH because it may not mean anything is wrong with the thyroid, but rather that dysfunction in another system of the body is present.
- “TSH may be mildly suppressed in acute illness and mildly elevated during recovery from acute illness. However, TSH values are typically not suppressed to < 0.1 mIU/mL or elevated to > 10 mIU/mL in these circumstances.”
- Because of this, it’s important to see repeat imbalance in TSH before clinical action is taken, as one high or low TSH may not be meaningful.
- “The importance of these issues is mainly that any clinical decision should not be made (in a non-pregnant patient) based on a single TSH value if it is within or close to the normal range.”
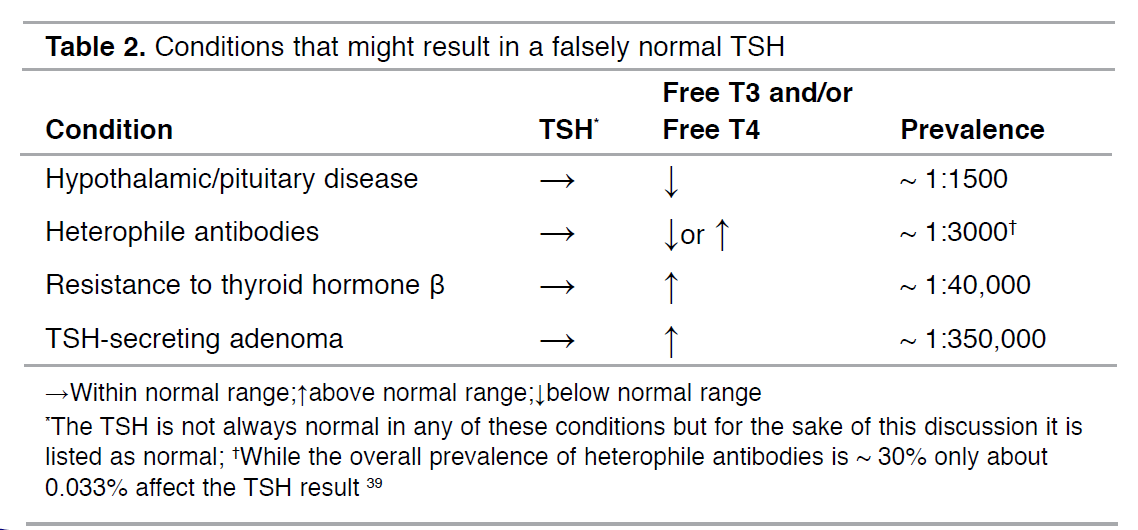
- The authors offer the following table to guide interpretation:
TSH
- The normal range for TSH is likely between 0.5-2.5.
- “most normal” range is between 0.5 mIU/mL and 2.50 mIU/mL.”
- However, this doesn’t mean that one requires thyroid hormone treatment when outside of these ranges. My advice would be to first retest, then if the imbalance persists, focus on other sources of stress/illness that might be driving the minor perturbation in TSH. However, and importantly, when administering thyroid hormone, the goal of TSH should be between 0.5-2.5.
- “It is for this reason that the target TSH in the management of hypothyroidism is within this latter range”
- “Note that the goal range for replacement therapy is different than the range at which hypothyroidism is diagnosed (ie, while a TSH of 4.2 mIU/mL may warrant an increase in levothyroxine (L-T4) dose, it does not warrant initiation of replacement therapy in a non-pregnant patient).”
- Starting or adjusting thyroid hormone dose when TSH is above 2.5 is OK for during pregnancy.
- “Pregnancy is the one circumstance wherein initiation or adjustment of replacement therapy with L-T4 is indicated for a TSH within the upper normal range.”
- TSH secretion experiences a circadian rhythm with the highest levels secreted in the early morning. This can cause a natural fluctuation of up to 2 points. This is why it is often recommended to standardize time of testing to morning. Also, this is why one should retest before jumping to conclusions based upon one small increase in TSH.
- “… this circadian rhythm may cause a variation in TSH by a mean of between 0.95 mIU/mL to 2.0 mIU/mL.”
- “and in one small study 50% of patients with a mildly elevated TSH between 8:00–9:00 am had a normal TSH (< 4.0 mIU/mL) when assessed between 2:00–4:00 pm.”
- TSH can also naturally vary from month to month and indicate no problem is present.
- “Also underappreciated is the individual variation in TSH that occurs for no apparent reason. In a study assessing TSH values monthly for one year in healthy men, this apparent random variation occurred with a mean TSH of 0.75 mIU/mL and a range of 0.2–1.6 mIU/mL..”
- Small changes in TSH are likely not the cause of one’s symptoms, see below. This is also likely why there has been no consistent benefit from giving thyroid hormone to those with SCH, especially when TSH is below 10. You could always elect a trial of thyroid therapy, but most patients will likely be non-responsive.
- “…it should be explained that if/when the thyroid gland becomes completely non-functional, the TSH rises dramatically to levels often exceeding 100 mIU/mL. Common sense, therefore, needs to be used when attributing any given symptom to a patient’s thyroid status. That is, a TSH of 6.7 mIU/mL is not the cause of extreme fatigue or mood changes, whereas a TSH of 40.0 mIU/mL may indeed explain these same symptoms”
Subclinical Hypothyroid , TSH, and Thyroid Antibodies
- SCH is far more common than true hypothyroidism.
- “The prevalence of subclinical hypothyroidism is quite high at between 3.9% and 8.5% (versus the 0.2%– 0.4% prevalence of overt hypothyroidism).”
- This might make some remark that ‘SCH is the cause of my patient’s symptoms’ and thus requires treatment, which would be overzealous when considering over 50% may spontaneously normalize.
- “First, reassessment and not immediate replacement therapy is the best initial step in management. Indeed, in one study, spontaneous normalization occurred in 52% of patients with an initial TSH of 5.0-9.9 mIU/mL, while only 5.6% developed overt hypothyroidism over a mean follow-up of 31.7 months.” https://www.ncbi.nlm.nih.gov/pubmed/15472181
- The degree of elevation of TSH and the presence of thyroid antibodies increases the risk that a SCH patient will develop full hypothyroid; risk may increase to up to 55%.
- “It is extremely useful to have an understanding of the 20-year follow-up data of the Whickham survey in this regard. In that study, subjects with an elevated TSH (> 6.0 mIU/mL) alone developed overt hypothyroidism at a rate of just 2.6% per year; or 33% over the 20 years of follow-up. The presence of anti-TPO antibodies in addition to an elevated TSH imparted a higher risk of 4.3% per year or 55% at the end of follow-up.” https://www.ncbi.nlm.nih.gov/pubmed/7641412 (n= 1877)
- Again, you can perform a short trial of thyroid hormone in those with symptoms and mildly elevated TSH. If this shows clear benefit, continue. But remember to be objective.
- “…some providers consider a 3-month trial of low dose L-T4 therapy in patients with persistent mild elevation of TSH, then continuing therapy in those with improved symptoms and stopping it in those with no improvement.”
- Elderly subjects are least likely to improve after thyroid hormone for mildly elevated TSH as TSH appears to gradually increase with age.
- There are conditions that may result in a falsely normal TSH, but they are quite rare:
Free T4
- fT4 is required to diagnose hypothyroid in the presence of only mildly elevated TSH, so ordering this test in this situation seems logical.
- The method of testing fT4 used by many labs may be highly inaccurate (this includes one of the forms of T4 offered by LabCorp).
- “Most laboratories utilize the direct analog immunoassay (IA) for the measurement of free T4, and again the validity of the results are debated and poorly standardized.”
- The more accurate form of free T4 is by liquid chromatography-tandem mass spectrometry (LC-MS/MS). Available through LabCorp and Quest, here are the required codes.
- LabCorp: https://www.labcorp.com/test-menu/35856/thyroxine-tsub4-sub-free-dialysis-mass-spectrometry-endocrine-sciences
- Quest: http://www.questdiagnostics.com/testcenter/TestDetail.action?ntc=94196
- “In a comparison of the IA and LC-MS/MS method in 109 patients, the correlation between free T4 and TSH was quite poor for the IA method and substantially better for LC-MS/MS.”
- Note: Terminology can be a bit confusing. LC is used for HPLC and the term MS can be used for MS/MS.
Thyroid Antibodies
- May have their greatest utility in those who are infertile.
- “anti-TPO ABs is recommended in the setting of infertility and/or recurrent miscarriage—grade “A” in clinical guidelines (4). Many endocrinologists and gynecologists will recommend treatment with low-dose L-T4 therapy in anti-TPO ABs positive, euthyroid patients with a history of infertility and/or recurrent miscarriage. However, the efficacy of this practice is not fully proven with some (52), but not all (53), studies showing benefit.”
Reverse T3
- This paper essentially concludes that rT3 is elevated in “non-thyroidal illness,” therefore rT3 does not have any clinical relevance. This position is understandable as rT3 does not tell you where the problem is coming from.
Clinical Takeaways:
- There is a lot here, but here are a few thoughts:
- TSH is the most impactful measure of thyroid function.
- T4 can be helpful, but many forms of T4 are inaccurate.
- TPO antibodies and TSH can be used as predictive measures.
- TPO might be most important for those who are pregnant.
- Reverse T3’s utility might be overstated.
Dr. Ruscio’s Comments
This paper made several good points. While I did not agree with everything listed in it, I have pulled out the points that are most impactful. Big picture, this paper helps support the notion that the expanded thyroid panels might not be as clinically useful as many would have you believe. TSH and an accurate free T4 appear most useful and there is also a place for TPO antibodies. The value of free and reverse T3 does not appear to be as important.
Mouthwashes with hydrogen peroxide are carcinogenic, but are freely indicated on the Internet: warn your patients!
https://www.ncbi.nlm.nih.gov/pubmed/24351145
Study purpose:
- To determine if a popular mouthwash and teeth whitening recommendation, hydrogen peroxide, is carcinogenic.
Intervention:
- One author’s commentary.
Main Results:
- Hydrogen peroxide might be a carcinogen.
- “Tooth bleaching agents, all hydrogen peroxide-based, are carcinogenic agents. In other words, they potentiate the action of other chemicals (which are widely present in our daily routine) over the DNA of cells present in the oral mucosa, just like alcohol does. This effect on the DNA, which is produced by hydrogen peroxide, has been proved by many researches (1,10,11,12,13,17,19,20).”
- “In the oral mucosa, hydrogen peroxide potentiates the effect of many other carcinogenic agents found in patient’s mouth. These carcinogenic agents may originate from food, cosmetics, hygiene products, pesticides, herbicides, tobacco, alcohol, virus, among others (1,17).”
- Chronic alcohol or hydrogen peroxide use may increase risk of oral cancer.
- “Mouth washing with hydrogen peroxide, using products made with alcohol or drinking alcohol everyday may lead to the risk of oral chemical carcinogenesis (5,14).”
- When dentists use whitening agents, they work to ensure minimal exposure to the chemicals used. This, of course, does not happen when using peroxide as a mouthwash.
- “When hydrogen peroxide acts directly on tissues, it is transformed into hydroxyl radicals and superoxides that are extremely toxic and reactive. They produce devastating effects by oxidizing vital components, such as cell membrane and DNA, and may cause mutations.”
- While hydrogen peroxide may whiten teeth, it may damage other tissues of your mouth.
- “Hydrogen peroxide reddens the mucosa and gingiva by wounding them with tissue dissolution and inflammation. Hydrogen peroxide burns and may lead to necrosis of gingival papillae. It completely cleans the teeth because it demineralizes the enamel and also removes dirt or pigments. The enamel becomes porous (2,6).”
Author’s Conclusion:
- “Those websites, blogs and social network profiles trespass the limits of public trust and should be immediately sued by the government for committing a crime against public health.”
Clinical Takeaways:
- We may want to refrain from recommending or using hydrogen peroxide as a mouthwash or for teeth whitening.
Dr. Ruscio’s Comments
This article makes some concerning claims regarding hydrogen peroxide. This is only one article, and I would like to see what the overall body of evidence shows. I am especially curious to see what a deeper examination of the literature suggests, because I suspect some bias from the author. Why? Because they make some very strong claims. In my experience, strong and emotional claims often indicate someone is so passionate about a topic that they have lost objectivity. Nonetheless, I thought this article was important to share because I know using hydrogen peroxide is fairly popular in some natural health circles. Finally, I reached out to a few of my colleagues in dentistry and there was some agreement with this paper.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!