Practitioner Research Review – May 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Concomitant Prevalence of Low Serum Diamine Oxidase Activity and Carbohydrate Malabsorption.
https://www.ncbi.nlm.nih.gov/pubmed/28042564
Study purpose
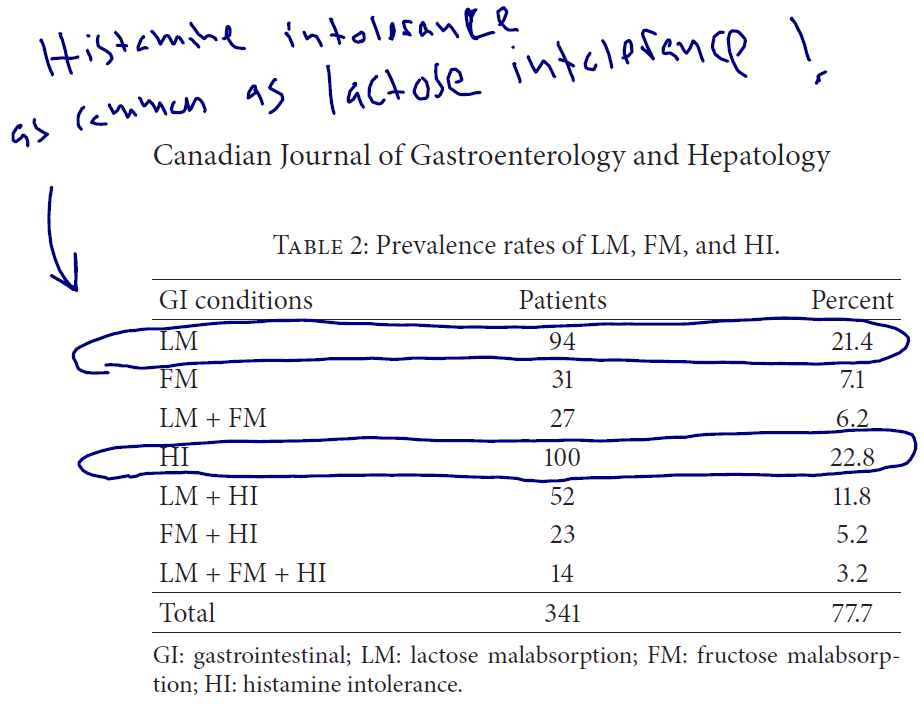
- “to analyze the concomitant prevalence rates for lactose malabsorption (LM), fructose malabsorption (FM), and histamine intolerance (HI) in patients with so far unexplained gastrointestinal (GI) symptoms.”
Intervention:
- A total of 439 outpatients, who presented unclear abdominal discomfort, underwent lactose (50 g) and fructose (25 g) hydrogen (H2) breath tests. Additionally, serum diamine oxidase (DAO) measurements were performed.
Main Results:
- Impact on condition, symptoms, lab markers, etc.
Additional Results:
- Roughly 43% of subjects had low DAO
- “All in all, 51 individuals (11.6%) were identified with a serum DAO level < 3U/mL, 138 patients (31.4%) had a serum DAO level between 3 and 10U/mL.”
- 23% showed histamine tolerance – making it as common as lactose intolerance in this group
- 1/3 of those diagnosed with fructose or lactose malabsorption were also shown to have histamine intolerance. So, 1/3 of your patients with carb malabsorption may also have histamine intolerance.
Authors’ Conclusion:
- “Different combinations of LM, FM, and HI are present in individuals with unclear abdominal discomfort/pain. In clinical practice we suggest testing for LM, FM, and additional HI in the diagnostic work-up of these patients. Depending on these various diagnoses possible, patients should get an individualized dietary advice.”
Interesting Notes:
- Abdominal pain, bloating, and diarrhea are some of the leading symptoms associated with histamine intolerance.
- Diagnosing histamine intolerance – DAO blood levels less than 10 highly increases risk.
- “According to the literature [8, 13], in individuals with serum DAO activity < 3U/mL, HI was expected, while in patients with serum DAO levels between 3 and 10U/mL, HI was considered possible. Patients with DAO levels < 10 U/mL were identified with HI only if they showed two or more GI symptoms of HI (e.g., nausea, vomiting, meteorism, and/or abdominal pain) and a positive response to a low histamine diet [8, 13].”
- The histamine degrading enzyme, DAO, is released by the villi of the small intestine. When the intestine is damaged, it may reduce the manufacturing of this enzyme – similar to lactose and lactose intolerance.
- How to treat histamine intolerance
- “Therapy of HI should be based on a consequent avoidance of histamine-rich food (e.g., spinach, tomatoes, long-ripened or fermented products, alcohol) or histamine liberators (e.g., citrus fruits, chocolate).”
Clinical Takeaways:
- In patients who are only partially responsive to other dietary changes, the addition of a low histamine diet may also be helpful.
Dr. Ruscio’s Comments
I have seen enough patients respond to a low histamine diet to clearly see that this is something worth attention. This study did an excellent job of documenting how prevalent histamine intolerance might be.
While histamine intolerance can manifest with digestive symptoms, it can also manifest with other symptoms, which can include:
- Neurological: irritability, depression, brain fog
- Dermatological: rashing, flushing, hives, runny nose
- Insomnia, fatigue
Remember that a key giveaway on this can be people who react negatively to probiotics or probiotic rich/fermented foods, which can be high in histamine.
I disagree with the authors’ conclusion of performing all three tests (lactose, fructose, and histamine). The reason for this is it will get expensive and be cumbersome for patients. If you perform a trial of the Paleo Low FODMAP diet, you will cover both lactose and fructose eliminations. If someone has only partially responded to Paleo Low FODMAP, then adding a short trial of also following low histamine is advisable. By doing this you can have a good idea of someone’s ideal diet in 3-5 weeks and save hundreds on testing that would only lead you back to trying these types of diets anyways.
Also, remember that as you work to heal the intestines and correct any underlying sources of damage (celiac, non-celiac gluten sensitive, SIBO/candida/dysbiosis, IBD, H. Pylori, etc.…) you should see histamine tolerance improve.
Mast Cells and Irritable Bowel Syndrome: From the Bench to the Bedside.
https://www.ncbi.nlm.nih.gov/pubmed/26755686
Study purpose
- “therapies targeting mast cells, such as mast cell stabilizers (cromoglycate and ketotifen) and antagonists of histamine and serotonin receptors, have been tried in IBS patients, and have partially exhibited considerable efficacy. This review focuses on recent advances in the role of mast cells in IBS, with particular emphasis on bridging experimental data with clinical therapeutics for IBS patients.”
Intervention:
- A review of available data
Main Results:
- See below
Additional Results:
- “A placebo-controlled trail in 60 IBS patients showed that 8 weeks of treatment with ketotifen obviously increased the threshold for discomfort in IBS patients with visceral hypersensitivity, reduced IBS symptoms, and improved the health-related quality of life.[7]”
- Ketotifen = Zyrtec OTC
- “Preliminary clinical data indicated that a 6 month of DSCG treatment significantly reduced release of tryptase from jejunal biopsies, and increased clinical improvement of bowel function in D-IBS.[6]”
- DSCG (Disodium cromoglycate) is a mast cell stabilizer, commonly used as Rx Gastrocrom.
- “A double blind, randomized controlled trial evaluated the effects of the H1R-antagonist ebastin in IBS patients, in which 12 weeks of ebastin treatment resulted in a significant improvement in global symptom relief, abdominal pain, and quality of life.[102]”
- “Therapies targeting mast cells, such as mast cell stabilizers (cromoglycate and ketotifen) and antagonists of histamine and serotonin receptors, have been tried in IBS patients in several studies, and partially exhibited good efficacy in symptom improvement.[6,7]”
- Many pathways can activate mast cells (MCs) and mast cell activation is not limited to classic IgE activation, including stress and bacteria.
- Mast cells release histamine and other inflammatory mediators.
- “MCs in the gut, and participate in multiple pathophysiological processes and diseases beyond allergy, which including IBS, functional dyspepsia, inflammatory bowel disease, and intestinal infections.”
- Some studies show IBS patients have more mast cells than healthy controls, while other studies do not show this but rather show IBS patients have facilitated activation of mast cells.
- “MC stabilizers such as ketotifen and doxantrazole increased the threshold of pain and improved abdominal discomfort in IBS patients [35]”
Authors’ Conclusion:
- “Taken together, previous findings strongly argue in favor of MCs as remarkable players in the pathogenesis and pathophysiology of IBS.”
Interesting Notes:
- “Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal disorders worldwide, with the prevalence ranging from 1.1% to 29.2% in the general population diagnosed by the Rome III criteria”
- “MCs hyperplasia and activation lead to abnormal gastrointestinal sensitivity, motility, and secretion, which in turn contribute to the hallmark symptoms of IBS—abdominal pain and/or discomfort, bloating, and abnormal bowel function (diarrhea and/or constipation).”
- “Mast cells cause mucosal inflammation via neuronal stimulation provoked by stress. Psychological stress such as dichotomous auditory stimuli was reported to make mast cells release mediators in IBS. The mediators including histamine, serotonin, protease, cytokines, and chemokines could develop mucosal inflammatory responses.”
- “MCs stabilizers (chromones), which act primarily by stabilizing the plasma membrane of MCs, significantly improved abdominal pain and stool consistency in patients with D-IBS.25 Similarly, ketotifen increased the rectal threshold for discomfort, markedly reduced the severity of abdominal pain, and improved quality of life in IBS patients.[25]”
- When MCs are activated, that initiates a positive feedback loop (self-feeding) of inflammation.
- MCs do impact motility.
- “Numerous evidence showed a positive relationship between the number of mucosal MCs and intestinal permeability [61]”
- “MCs are proposed as key players in the initiation and maintenance of the inflammatory circuitry in the intestine.”
- “MCs also act as gatekeepers to protect the host against bacterial infections”
- “… growing evidence support the view that intestinal commensal or probiotic bacteria suppress MC activation.”
- “Acute or chronic stress exposure has widely impacted on intestinal functions and MC activation.”
- Stress can induce leaky gut mediated by mast cells; this could be blunted by the administration of cortisol suppressing agents.
Clinical Takeaways:
- Mast cells are intimately involved in IBS and agents/interventions that stabilize mast cells and or lower histamine may be a viable therapeutic options for patients that do not respond to other therapies.
Dr. Ruscio’s Comments
Mast cells are part of a self-feeding immune/inflammatory cycle in the gut that requires an ‘unwinding period’ to normalize. What this may look like is the standard approach needed for many chronic/severe IBS patients. More specifically, an initial phase of a restrictive diet (paleo, low FODMAP, low FODMAP/SCD, low histamine, elemental diets) combined with other treatments (probiotics, Habx, enzymes), which allows dampening of this feedback loop. After a number of months, this then allows the patient to successfully broaden their diet and reduce their treatments. Time may simply be a factor needed for this feedback loop to unwind, so be patient with your patients and reassure them that if they relapse and/or need ongoing treatment, it does not mean they are ‘failing.’ Sometimes the improvements are slow and gradual, and it just takes time.
I am starting to think that histamine lowering agents and/or gut repair agents are best used end phase for those who need to address the above problem. For most/many patients, histamine lowering agents and/or gut repair nutrients are not needed (in my opinion), because once you address gut fundamentals they will respond fully.
Drug therapy in the short term may also help to unwind this self-feeding loop in more severe cases.
Helicobacter pylori and autoimmune disease: Cause or bystander
https://www.ncbi.nlm.nih.gov/pubmed/24574735
Study purpose
- Review the data regarding HP and its association to autoimmune diseases.
Intervention:
- Review the data regarding HP and its association to autoimmune diseases.
Main Results:
- Overall this paper shows
- There is mixed association data between H. pylori and autoimmunity and
- There is less data, which is also mixed regarding if treatment of HP improves autoimmunity.
Additional Results:
- Regarding treatment data:
- RA – two studies showed improvement in RA while two studies did not show improvement after treatment for HP
- Psoriasis – mixed data has also been found for psoriasis
- Urticaria – mixed data has also been found
- Thyroid – only one treatment study has been performed; it showed positive results
Authors’ Conclusion:
- “H. pylori remains one of the most attractive candidate pathogens that could trigger autoimmunity. The ubiquitous nature of this pathogen may explain why it has been implicated in a large number of autoimmune conditions. There is no doubt that more basic work in immunological aspects of the microbial-host interactions is needed to address the pathogenic role of this multi-faceted pathogen.”
Interesting Notes:
- “Helicobacter pylori (H. pylori) is the main cause of chronic gastritis and a major risk factor for gastric cancer. This pathogen has also been considered a potential trigger of gastric autoimmunity, and in particular of autoimmune gastritis.”
- Theories as to why HP might stimulate autoimmunity
- Through increased and systemic inflammation (CRP)
- Molecular mimicry
- “H. pylori is one of the very few infectious agents (along, for example, with Epstein-Barr virus) that have been considered a common denominator in more than 30 autoimmune disorders.”
Clinical Takeaways:
- Conservative treatment of HP is a consideration in those with autoimmune conditions.
Dr. Ruscio’s Comments
Overall, this paper shows 1) there is mixed association data between H. Pylori and autoimmunity and 2) there is less data, which is also mixed regarding if treatment of HP improves autoimmunity. In asymptomatic HP carriers with autoimmunity, we can make the strongest case for treating HP with natural agents, since they have little to no side effects. In symptomatic (ulcers, gastritis, dyspepsia) HP carriers, any treatment approach is advisable whether or not the person has an AI.
It is also interesting to consider this: could part of the reason that some of the treatment studies show benefit be because the antibiotics (metronidazole, amoxicillin…) used to treat HP are also treating other dysbiosis/infections like SIBO, Yersinia, etc.…?
Cannabinoids and autoimmune diseases: A systematic review
https://www.ncbi.nlm.nih.gov/pubmed/26876387
Study purpose
- To summarize the available data regarding cannabis and autoimmune diseases
Intervention:
- To summarize the available data regarding cannabis and autoimmune diseases
Main Results:
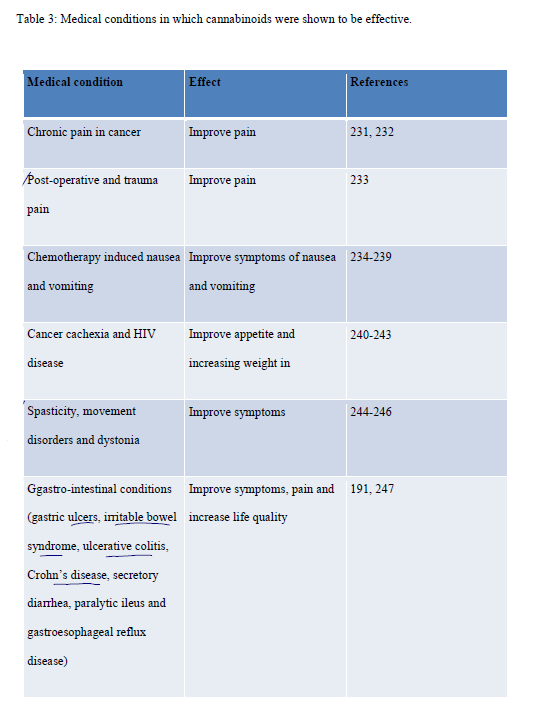
Inflammatory bowel disease
- “In a prospective placebo-controlled study with 21 Crohn Disease patients [200], cannabis induced clinical remission in 50% of patients. 80% of the participants had nonresponse or intolerance to anti–TNF-alfa.” (Note: anti-TNF-alfa is drug therapy.) “Although, the improvement was only symptomatic, with no induction of remission comparing to placebo. When patients discontinued the cannabis therapy, relapses were noticed in 2 weeks.”
- “Other cohort study of patients with IBD using cannabis [201] also reported that the patients perceive that it improved abdominal pain. Patients with UC, in particular, reported cannabis to improve diarrhea.”
- “In another observational study [202], this time with in 30 patients with Crohn’s disease, medical cannabis was associated with improvement in disease activity and reduction in the use of other medications was reported.”
- “Usually, 25% to 38% of operated Crohn’s disease patients require a second operation within 5 years [203], but in a retrospective cohort study [204] only 2 of 15 patients (13%) who had surgery before cannabis consumption required surgery while consuming cannabis. Studies are still needed, but this one suggested that the use of cannabis reduces the need for surgery.””
- “Some patients with UC and CD also use cannabis to enhance appetite [205]. In a study of 13 patients using cannabis for 3 months, a statistically significant increase in the subject’s weight was observed [206]. They also presented improvement in the disease activity index, perception of general health status, and ability to perform daily activities.”
Other conditions
- One study in MS did not find cannabis slowed disease progression, but two other studies found cannabis improved spasticity and pain.
- One study showed a slight improvement in RA symptoms.
- “A randomized double-blind placebo-controlled trial published in 2014, [207] compared medium dose (3.53% THC) to low dose (1.29% THC) cannabis, to see if the analgesia was sufficient in the low doses. The purpose was that if it is as effective as the medium dose, it should be used preferentially, to avoid side effects. Both provided statistically significant 30% reductions in pain intensity when compared to placebo.”
- “One retrospective study of fibromyalgia affected patients who were chronic users of cannabis, analyzed the effect of smoked, oral and combined cannabis on symptoms and the quality of life. A significant reduction of pain and stiffness, enhancement of relaxation, and an increase in somnolence and feeling of wellbeing were observed in cannabis users. Furthermore, mental health component summary score was significantly higher (p=0.05) in cannabis users than in non-users [228].”
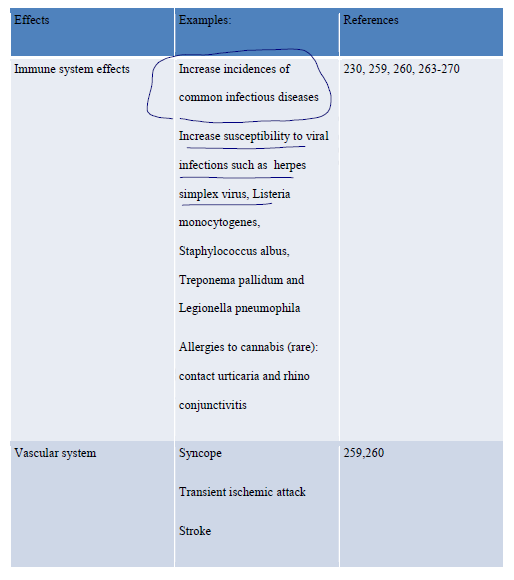
Side Effects
- “In a systematic study [230], 8371 adverse events related to medical cannabinoid use were reported, 4779 of which were reported in 23 randomized controlled trials and 3592 in 8 observational studies.”
- “Patients in cannabinoid therapy presented twice the incidence of severe adverse events than control groups. Respiratory (16.5%), gastrointestinal (16.5%) and nervous system disorders (15.2%) were the most frequently reported categories of serious adverse events among those assigned to cannabinoids.”
- “The incidence rate of non-serious adverse events was significantly higher among subjects assigned to cannabinoid therapy than among controls, dizziness being the most frequent non-serious adverse event among cannabinoid-exposed participants.”
Immune system side effects, chart
Additional Results:
- “Current research in the role of cannabinoids in the immune system shows that they possess immunosuppressive properties. They can inhibit proliferation of leucocytes, induce apoptosis of T cells and macrophages and reduce secretion of pro-inflammatory cytokines.”
- “Cannabidiol, on the other hand, has low affinity for the CB1 and CB2 receptors, resulting in no psychoactive effects. Besides, Cannabidiol is well tolerated without side effects when chronically administered to humans”
- This is known as CBD, a non-psychoactive fraction of cannabis.
- “Cannabinoids were shown, in vivo and in vitro, to exert their immunosuppressive properties through 4 main pathways: induction of apoptosis, inhibition of cell proliferation, inhibition of cytokines and chemokines production and induction of regulatory T cells (T regs).”
- “Despite all these data, some studies suggest that cannabinoids could also have pro-inflammatory effects. [128,129]: promoting allergic reactions [130]; releasing inflammatory mediators through CB1 receptors in mast cells [129], increasing B cell proliferation [95].”
- “The key to understand the role of cannabinoids in immunomodulation is to stress that their effects depend on the type of cannabinoid, on the type of cells that they are acting on and on the doses administrated. In optimal concentrations, cannabinoids can induce apoptosis in immune cells, alleviating inflammatory responses and protecting the host from acute and chronic inflammation. Thus, they can be beneficial when an immune suppression is necessary. Additional research is still needed to validate these studies in humans through clinical trials.”
- “The effects of cannabinoids include analgesia, muscle relaxation, immunosuppression, anti-inflammation, anti-allergic effects, sedation, improvement of mood, stimulation of appetite, antiemesis, lowering of intraocular pressure, bronchodilation, neuroprotection and antineoplastic effects.”
Authors’ Conclusion:
- “Cannabinoids are potent inflammatory modulators and in several animal studies, in vivo and in vitro, they have shown to have an immunosuppressive effect. However, human studies are still few.”
Interesting Notes:
- See above
Clinical Takeaways:
- Medical cannabis may benefit certain immune and inflammatory conditions. Since there is limited data, and a fair number of documented side effects, it is likely best considered after a patient has failed out of preliminary therapies.
Dr. Ruscio’s Comments
Medical cannabis caught my attention after hearing a few patients remark that it was very helpful for alleviating digestive symptoms. Interestingly, it looks like the evidence supports their observations. When I step back and look at the data here, limited as it may be, it appears that cannabis functions as an anti-inflammatory and immunosuppressive agent. However, like many agents of this class, they may also increase risk of certain infections, so striking the right balance is key.
So where does this fit into the larger clinical picture? Let’s use IBD as an example. Front line therapies for IBD should be considered before cannabis, in my opinion. So, before cannabis use: diet, probiotics, enzymes, anti-inflammatory herbs, herbal antibiotics, antibiotics, elemental diets… After this, a cautious trial of cannabis before using a powerful drug like Humira, makes sense to me. And perhaps we can assign cannabis to an equivalent position as to Mesalazine, perhaps used together to try to mitigate the amount of one agent used, but this is merely my own speculation.
Cannabis does have side effects, the main one being the ‘high’ which can interfere with performing tasks requiring full cognitive function. One final note: some people have a strong aversion to THC in my observation. Instead of the euphoric type ‘high,’ they tend to become self-conscious, paranoid, depressed, and feel generally not well on cannabis that contains even over a couple mgs of THC. However, in my limited observation, these same patients are fine when using a CBD only preparation wherein the total TCH concentration is ideally below 1-2mg per dose.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!