Practitioner Research Review – June 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Functional food addressing heart health: do we have to target the gut microbiota?
https://www.ncbi.nlm.nih.gov/pubmed/26406391
Study Purpose:
- Review the evidence regarding functional food’s benefit for cardiovascular health.
Intervention:
- Review of the literature.
Main Results:
- “Perhaps one of the most intriguing microbiota-mediated therapies for heart health currently is bile salt hydrolase (BSH) expressing probiotics.”
- Note: these probiotics release enzymes that deconjugate (deactivate) bile. This ultimately reduces their reabsorption in the terminal ileum, thus the liver then needs to produce more bile, which requires cholesterol. This then lowers blood cholesterol levels.
- “prompting hepatic de-novo synthesis of bile acids – of which cholesterol is a major component. This in turn decreases circulating and liver triglycerides and plasma LDL and very-low lipoprotein cholesterol (VLDL) levels.”
- “The probiotic Lactobacillus reuteri NCIMB 30242 is one particularly active BSH candidate that has been brought to market. When delivered in capsule or yoghurt to otherwise healthy hypercholesterolemic individuals, the probiotic intervention caused reduction of circulating LDL by 9–12%, total cholesterol by 5–9%, and the ratio of apolipoprotein B to A (apoB/apoA) by up to 13%.”
- “Furthermore, Lactobacillus reuteri NCIMB 30242 was shown to reduce two major factors of atherogenesis, CRP and fibrinogen, while also inhibiting noncholesterol sterol absorption.”
Additional Results:
- N/A
Authors’ Conclusion:
- “The microbiota offers a modifiable target, which has the potential to progress or prevent cardiovascular disease development.”
Interesting Notes:
- Methanogenic archaea have been proposed as a method for reducing TMAO.
Clinical Takeaways:
- Probiotics may aid in heart disease prevention, in part, via their cholesterol lowering effect. A multi-strain blend that includes Lactobacillus acidophilus may be best.
Dr. Ruscio’s Comments
Do you need a ‘special’ probiotic? Not likely in my opinion, as a standard blend as seen in VSL#3 has shown to have bile lowering activity in mouse models.
- Most recently, a probiotic mixture of Streptococcus thermophilus, Bifidobacterium spp., and Lactobacillus spp., marketed as VSL#3, has demonstrated significant BSH activity in a mouse model. https://www.ncbi.nlm.nih.gov/pubmed/24656817
This is likely why when we look at the clinical data we see that systematic reviews and meta-analyses show that probiotics, which are multi-strain, have benefit in cholesterol lowering. The inclusion of L. acidophilus appears to be important in the blend also.
- “A significant reduction was found in LDL in trials which contained Lactobacillus acidophilus strain compared to other types of strains”. https://www.ncbi.nlm.nih.gov/pubmed/26340330
- “Lactobacillus acidophilus strain reduced TC and LDL-C levels to a greater extent than other bacterial strains.” https://www.ncbi.nlm.nih.gov/pubmed/26473340
Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus.
https://www.ncbi.nlm.nih.gov/pubmed/28323273
Study Purpose:
- Update and improve when we order SIBO breath testing (BT) and how we interpret the results.
Intervention:
- 17 clinician-scientists were surveyed to develop a consensus.
Main Results:
- BT is useful in the diagnosis of
- Methane-associated constipation,
- Evaluation of bloating/gas, and
- Carbohydrate maldigestion, but
- Not in the assessment of oro-cecal transit.
- A rise in hydrogen of ≥20 p.p.m. by 90 min during glucose or lactulose BT for SIBO was considered positive.
- Methane levels ≥10 p.p.m. was considered methane positive.
- SIBO should be excluded prior to BT for carbohydrate malabsorption to avoid false positives.
- A rise in hydrogen of ≥20 p.p.m. from baseline during BT was considered positive for maldigestion.
Additional Results:
Testing prep
- Antibiotics should be avoided for 4 weeks prior to the breath test.
- No conclusion regarding stopping pro/prebiotics prior.
- If tolerated by the patient, promotility drugs and laxatives should be stopped at least 1 week prior to breath testing.
- Avoid fermentable foods 1 day prior, and fasting 8-12 hours prior.
- No smoking, avoid rigorous activity.
- No need to stop PPIs prior to testing.
Indications for testing
- Small bowel culture is not satisfactory for assessing SIBO.
- Consensus panel suggests
- Breath testing as diagnostic tool for SIBO.
- To evaluate for excessive methane in association with constipation and slowing of gastrointestinal transit.
- SIBO breath testing in assessing conditions with bloating.
- Breath testing for carb malabsorption.
Performing the test
- 10g lactulose, using more may speed transit and alter results.
- 75g glucose, predominantly due to convenience.
- Rule out SIBO before testing for carb malabsorption.
- Test H2, CH4, and CO2.
- Breath tests may be performed shortly after cessation of antibiotic therapy to confirm eradication.
Interpretation:
- A rise of ≥20 p.p.m. from baseline in hydrogen by 90 min should be considered a positive test to suggest the presence of SIBO.
- Two peaks are not required.
- Until further data is available, we suggest that a level of ≥10 p.p.m. be considered positive for methane on a breath test.
- Inconclusive data regarding a methane of ≥3 p.p.m..
Authors’ Conclusion:
- See above.
Interesting Notes:
- Those with CH4 are 5 times more likely to have constipation, not guaranteed.
- However, lactulose has been shown to shorten oro-cecal transit time (57), and the test has been shown to have poor reproducibility with wide variation among healthy subjects (1).
Clinical Takeaways:
- There are many here, read above for the details.
Dr. Ruscio’s Comments
Lots of important details here. Here are a couple that I feel to be most clinically impactful.
- The shortened time window for the lactulose test will reduce its high level of false positives.
- Double peak is no longer relevant – my clinical suspicion for some time…
- Refined guidelines for methane interpretation. I have felt that labeling someone as ‘SIBO positive’ with a 3 or 4 ppm methane is a bit overzealous. Someone can still be treated for a 3-4, but we don’t have to label them as ‘positive.’ Remember, the more diagnoses you assign to a patient, the more distressed they can become, so don’t throw around diagnoses or talk of diseases/disorders lightly.
Why is this important for continued recognition of SIBO in the health/medical community? Because we need to get on the same page for exactly how we test and define SIBO.
- “A systematic review found 13 case-control studies that used breath testing to diagnose SIBO. Detailed examination of these studies reveals that they used 13 different methodologies to conduct the breath test or interpret the results.”
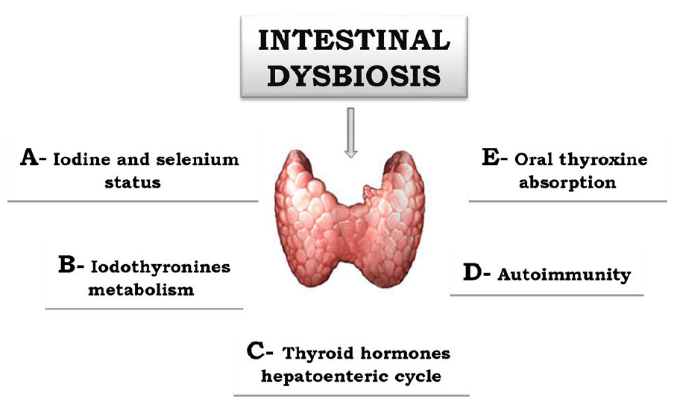
Does microbiota composition affect thyroid homeostasis?
https://www.ncbi.nlm.nih.gov/pubmed/25516464
Study Purpose:
- A commentary on the gut-thyroid connection.
Intervention:
- N/A
Main Results:
- “It is well known, however, that some disorders of the upper intestinal tract are associated to different microbiota profiles and concurrently to an increased need for thyroxine.”
- Celiac
- Lactose intolerance
- Hypochlorhydria
- Note: those with H. pylori do better when using liquid thyroid Rx.
Additional Results:
- N/A
Authors’ Conclusion:
- “The state of art of microbiota effects on thyroid economy is far from being fully clarified. As described above, the upper intestinal tract is crucial for the whole balance of both exogenous and endogenous thyroid hormones.”
Interesting Notes:
- Intestinal dysbiosis may trigger thyroid autoimmunity.
- Hypothyroid has been associated with SIBO. (https://www.ncbi.nlm.nih.gov/pubmed/17698907)
- SIBO has a high affinity for selenium (https://www.ncbi.nlm.nih.gov/pubmed/18829286), therefore SIBO might reduce selenium levels. This may then contribute to development of thyroid autoimmunity.
- Rat studies have shown that intestinal bacteria can bind thyroid hormone.
Clinical Takeaways:
- Those with hypothyroid or thyroid autoimmunity should be screened for SIBO.
- Speculatively – SIBO may contribute to thyroid AI by depleting selenium.
- Those with dysbiosis may need a higher dose of thyroid Rx or an easier-to-absorb form of Rx.
Dr. Ruscio’s Comments
Not a lot to say here, I think the info speaks for itself. The impact of the gut on thyroid hormone absorption, metabolism, and thyroid autoimmunity is substantial. This is why I recommend starting with the gut in most thyroid cases.
Can UV Exposure Reduce Mortality?
https://www.ncbi.nlm.nih.gov/pubmed/21454422
Study Purpose:
- To assess how sun and ultraviolet exposure influences risk of death.
Intervention:
- “prospective study of 38,472 women in Sweden who were followed for 15 years”
Main Results:
- “…a significant reduction in all-cause mortality and in cardiovascular mortality associated with several measures of sun exposure. In addition, ultraviolet exposure from tanning beds is associated with a significant increase in all-cause mortality and cancer mortality.”
Additional Results:
- Sun exposure – Overall mortality was reduced among those who
- had been sunburned 2 or more times a year as teenagers compared with those who had been sunburned 1 or fewer times.
- Overall mortality and CVD mortality was reduced among those who had taken sunbathing vacations more than once a year during 3 decades.
- Tanning beds – Conversely, solarium use once or more per month for at least a decade increased the risk of all-cause deaths compared with those who never used solariums, as well as total cancer deaths.
Author’s Conclusion:
- See ‘Main Results.’
Interesting Notes:
- “The study has an excellent design (a prospective cohort), repeated measures of sun exposure and diet and is able to control for a number of potential confounders, such as pigmentation, BMI, education, and exercise.”
- “It is well established that chronic sun exposure does not increase risk for developing melanoma although the mechanism for that observation is unclear.”
- The authors make the note that intermittent sun exposure is associated with 1.6% increased risk of melanoma while chronic sun exposure is protective. Key point.
Clinical Takeaways:
- Sun exposure is protective against death from any cause, tanning bed use increases risk of death from any cause.
- Chronic sun exposure protects from melanoma, intermittent sun exposure increases risk of melanoma by 1.6%.
Dr. Ruscio’s Comments
Again, the data here are pretty clear and compelling: sun exposure appears to be good for you and may even protect against melanoma. The finding that tanning beds are harmful should be emphasized and helps clarify what was formerly an issue of debate. Advise your patients to enjoy the sun, but always practice protection as needed to avoid burning.
Crossover Control Study of the Effect of Personal Care Products Containing Triclosan on the Microbiome
http://msphere.asm.org/content/1/3/e00056-15
Study Purpose:
- To assess if triclosan and triclocarban, components of many household and personal care products (HPCPs), may alter the oral and gut microbiota, with potential consequences for metabolic function and weight.
- Triclosan and triclocarban are commonly used commercial microbicides found in toothpastes and soaps.
Intervention:
- Double-blind, randomized, crossover study. N=16.
- Participants were given triclosan- and triclocarban-containing (TCS) or non-triclosan/triclocarban-containing (nTCS) household and personal care products for 4 months, and then switched to the other products for an additional 4 months.
- Blood, stool, gingival plaque, and urine samples and weight data were obtained at baseline and at regular intervals throughout the study period.
Main Results:
- “Although there was a significant difference in the amount of triclosan in the urine between the TCS and nTCS phases, no differences were found in microbiome composition, metabolic or endocrine markers, or weight.”
Additional Results:
- A non-significant weight gain was reported in 30% of subjects when using triclosan compared to when not using.
- “Two subsequent studies have been contradictory on the matter, one reporting decreased BMI associated with increasing triclosan and another finding no association between triclosan levels and weight.”
Authors’ Conclusion:
- “Though this study was limited by the small sample size and imprecise administration of HPCPs, triclosan at physiologic levels from exposure to HPCPs does not appear to have a significant or important impact on human oral or gut microbiome structure or on a panel of metabolic markers.”
Interesting Notes:
- “Although toothpaste with triclosan reduces plaque and gingivitis, no other benefits to human health have been established to support the use of TCS in other HPCPs.”
- “In December of 2013, the FDA issued a ‘proposed rule’ requiring manufacturers of antibacterial hand soaps and body washes to provide evidence within 1 year that their TCS products are both safe and more effective than plain soaps in preventing illness (12). In response to both governmental and public concerns, TCS have now been largely removed from commercial soaps in the United States. However, triclosan remains in some toothpaste and hospital products, and triclocarban is still incorporated in nonconsumable household items. The effects of broad exposure to TCS on healthy human.”
Clinical Takeaways:
- Triclosan and triclocarban do not pose a risk of detriment to the microbiota or metabolism, based on this small study.
Dr. Ruscio’s Comments
It’s important to take data like this into account, because overzealous recommendations can create unneeded difficulty and fear in a patient’s life. While habitually using antibacterial soaps and personal care products is likely not a good idea, we also do not want to create an air of need for absolute avoidance.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!