Free Practitioner Research Review- July 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap; however, the research studies are a collection of the most clinically meaningful research that has been published recently.
Histamine intolerance and dietary management: A complete review
https://www.ncbi.nlm.nih.gov/pubmed/27590961
Study purpose
- Review dietary management of histamine intolerance.
Intervention:
- A review of literature.
Main Results:
- There is inconsistency in the data regarding histamine content of foods.
- Highest histamine foods ranked in decreasing order:
- “‘dried anchovies’, ‘fish sauce’, ‘fermented vegetables’, ‘cheese’, ‘other fish and fish products’ and ‘fermented sausages.”
- “People with gastrointestinal problems (gastritis, irritable bowel syndrome, Crohn’s disease, gastric and colon ulcers) are also at risk since the activity of the oxidases in their bowels is generally lower than in healthy individuals.” Note: at risk for histamine sensitivity
- Treatment
- “A histamine-free diet, if necessary, supported by antihistamines or the substitution of DAO, leads to an improvement of symptoms.”
- “Alcohol and long-ripened or fermented (and therefore histamine-rich) food, such as aged cheese, cured meat, and yeast products; histamine-rich food, such as spinach or tomatoes; or histamine liberators, such as citrus fruit, should be avoided.”
- “histamine degradation can be supported by the administration of vitamin C and vitamin B-6, which leads to an increase in DAO activity.”
Clinical Takeaways:
- Histamine intolerance is a legitimate issue and is more prone to occur in those with GI conditions.
Dr. Ruscio’s Comments
Since there is inconsistency in the data regarding dietary histamine content, you will see disagreement in low histamine diet guides. In my observation, the major sources of histamine are well identified and will overlap in most dietary guides, so keep it simple and focus on a general reduction of histamine. Don’t fret over the details. This also means that listening to one’s body upon reintroduction will be important.
When treating histamine intolerance, start with the same protocol laid out by case studies:
- Diet and lifestyle
- Probiotics and enzymes
- Dysbiosis
If response is minimal, consider a low histamine diet and low histamine support, such as antihistamines or vitamin synergists (vitamin C, B-6). With time, histamine tolerance should improve, just like we see with allergen tolerance or FODMAP tolerance.
Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study.
https://www.ncbi.nlm.nih.gov/pubmed/28223728
Study purpose
- “To identify a set of contributors, and weight and rank them on a pathophysiological basis.”
Intervention:
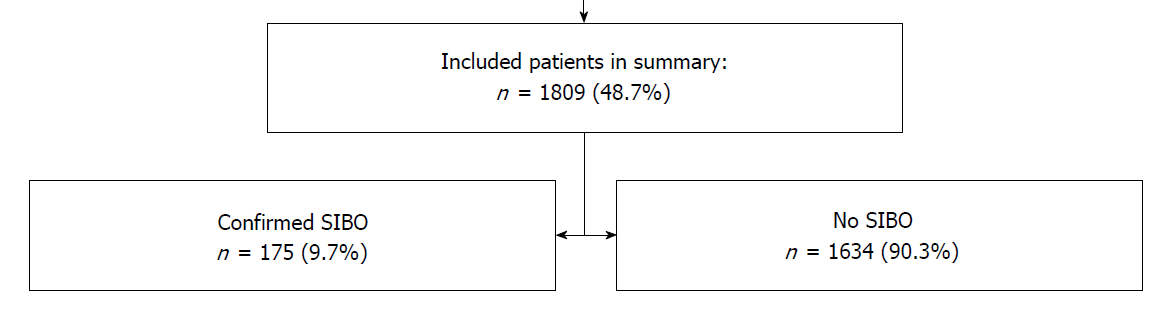
- “Patients who have undergone a lactulose or glucose hydrogen breath test to rule out small intestinal bacterial overgrowth (SIBO) for various clinical symptoms, including diarrhoea, weight loss, abdominal pain, cramping or bloating, were seen as eligible for inclusion in a retrospective single-centre study.”
- “A total of 1809 patients who had undergone hydrogen breath testing were analysed”
Main Results:
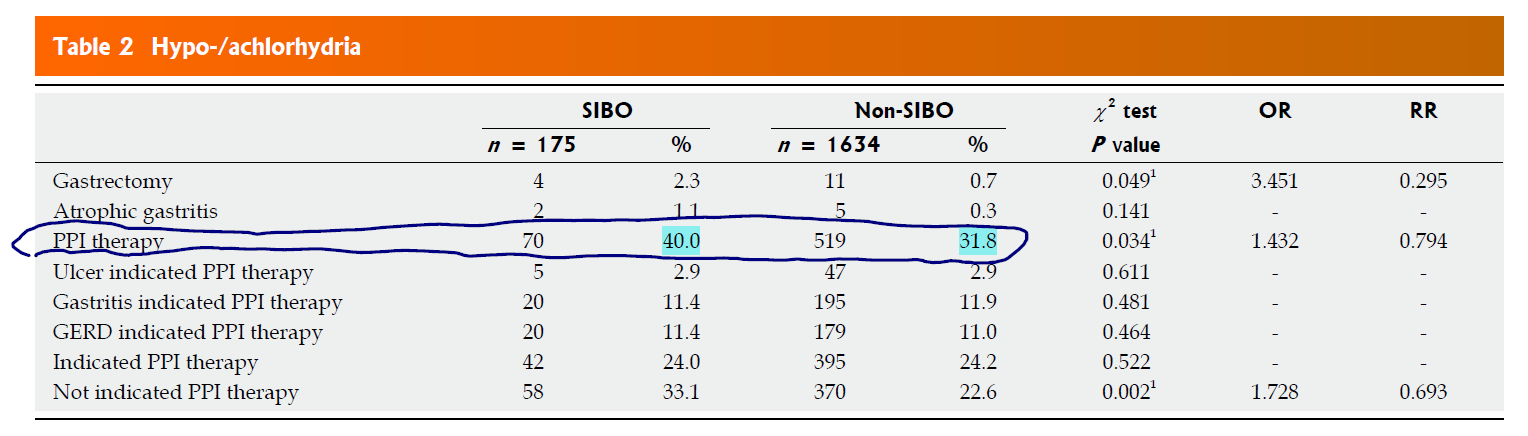
- The following were all significantly associated with SIBO
- Gastrectomy
- PPI therapy
- Any resecting gastric or colonic surgery
- Stenosis
- Gastroparesis
- Neuropathy
- Immunosuppressive therapy
- Hypothyroid or levothyroxine use
- Diabetes, type 2
Additional Results:
- Percentage of subjects with SIBO compared to controls in
- Hypothyroid (9.7% vs 4.0%)
- Levothyroxine use (17.1% vs 6.5%)
- PPI therapy also appeared more common in SIBO patients compared to controls
- “Loss of the ileocecal valve did not increase risk…”
- “…while a history of appendectomy occurred more often in non-SIBO patients (8.2% vs 6%), indicating a protective factor.”
- “Cholecystectomy tended to be protective (4.6% vs 7.8%).” Note: perhaps due to increased secretion of bile, which can occur after gallbladder removal. Not all studies show this same effect however.
- Impaired motility was associated with SIBO.
- Patients with hypothyroidism and patients with levothyroxine therapy showed a higher prevalence of SIBO compared to controls:
- Hypothyroidism (9.7% vs 4.0%)
- Levothyroxine (17.1% vs 6.5%)
- “A case control study by Lauritano et al [27] has already revealed a high prevalence of SIBO in patients with autoimmune thyroiditis and hypothyroidism.” Note: SIBO here was present in 54% of cases compared to 5% of controls. Treatment of SIBO here did not improve thyroid hormone levels, however.
- “One might speculate that hypothyroidism leads to hypomotility, but, surprisingly, levothyroxine therapy was even more associated to SIBO and not able to reverse the effect of hypothyroidism.”
Authors’ Conclusion:
- “The most important contributors for the development of SIBO in ascending order are immunosuppression, impairment of intestinal clearance and levothyroxine use, but they do not sufficiently explain its emergence.”
Clinical Takeaways:
- Those with hypothyroid or on thyroid medication are at significant increased risk of SIBO.
Dr. Ruscio’s Comments
This study illustrates a very important concept, which is there appears to be relatively a very strong association between SIBO and hypothyroidism, or the use of levothyroxine. In this study, these were even more associated with SIBO than prior intestinal surgery or the use of immunosuppressive drug use, although they were all shown to significantly associate to small intestinal bacterial overgrowth.
And there’s a few other items here that are also very interesting. Most notably that loss of the ileocecal valve did not increase risk. And there’s some contention around the role of the ileocecal valve in SIBO. And my thinking is that the importance of the ileocecal valve or specific ileocecal valve therapies has probably been a bit overstated. And while not all the data agree to my cursory knowledge on this, the summary of the evidence does seem to suggest a minimal role of the ileocecal valve in SIBO.
Also interesting is that cholecystectomy, or removal of the gallbladder, seems to be protective. Now, sometimes people erroneously think that the removal of the gallbladder will decrease or eliminate bile production, but that’s not true. The gallbladder is a temporary storage area for bile. But if you remove the gallbladder, you still have bile produced in the liver. And you actually have, potentially in some cases, a more continuous release of the bile. And as these authors speculate, potentially because of that slow, steady drip of bile, you’re having more of an antimicrobial effect, which bile has, and therefore joint protection against SIBO.
Now, this isn’t the first study to show an association between hypothyroidism and SIBO, as I also noted above, so that’s important to keep in mind. And also, it’s important to remember that in this study, it doesn’t appear that the association to SIBO is thyroid hormone dependent, because those who are hypothyroid and unmedicated showed less risk than those who were diagnosed as hypothyroid and had been on thyroid medication, and therefore had their thyroid hormone levels in the normal range, which suggests it is independent of thyroid hormone levels. And it may have something to do with the underlying thyroid disease itself that is not thyroid hormone dependent that has this impact.
In summary, it’s important to remember that there seems to be an increased prevalence of SIBO in those with hypothyroid. So I would recommend to consider this as something to test in hypothyroid patients, especially in hypothyroid patients that have digestive conditions. Remember that if someone’s had their gallbladder out, it doesn’t seem to be what someone termed “a death sentence,” and may actually be protective. So if there are strong indications for a gallbladderectomy, that’s not something that we should recommend against in our patient population.
Thyroid peroxidase antibody positivity is associated with symptomatic distress in patients with Hashimoto’s thyroiditis.
https://www.ncbi.nlm.nih.gov/pubmed/22285302
Study purpose
- Assess the association between general symptoms and Hashitmoto’s antibody levels.
Intervention:
- 64 patients with Hashitmoto’s had their antibodies assessed and filled out a general health questionnaire.
Main Results:
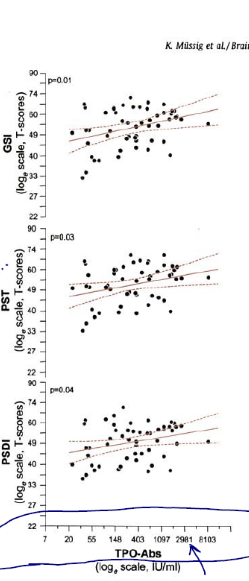
- TPO antibody positivity (defined at TPO>100) significantly predicted poorer psychosocial well-being.
- Note: the average level of TPO in this group was 1,122.
Additional Results:
- Other studies have found similar associations.
- The authors cite two other studies have found an association between thyroid autoimmunity and well-being.
- TG antibodies did not associate to well-being.
- A simple concept emerges here: the higher the antibodies, the poorer the well-being – see diagram.
Authors’ Conclusion:
- “…high TPO-Abs are associated with poor physical and psychological well-being and appear to predict future healthy perception.”
Interesting Notes:
- Hashimoto’s may impact circulation to the brain independent of thyroid hormone levels.
- Thyroid antibodies may also directly affect the brain in a pro-inflammatory manner.
- For example, those with AIT have more brain tissue antibodies than healthy controls.
- TPO antibodies can also directly bind to astrocytes.
- Increased levels of thyroid antibodies have been found in the cerebral spinal fluid of Hashimoto’s patients.
- The effects of Hashimoto’s on mood may be independent of thyroid hormone levels. https://www.ncbi.nlm.nih.gov/pubmed/28260699
Clinical Takeaways:
- Those with thyroid autoimmunity experience lower physical and psychological well-being. However, the level of autoimmunity matters, as the lower the autoimmunity the less the risk.
Dr. Ruscio Comments
This is a very interesting study, which showcases an important association, that association being the association between thyroid autoimmunity and physical and psychological well-being. What’s also important here is that the devil may be in the details. Oftentimes, those who have thyroid autoimmunity are overzealously feared into thinking it’s a somewhat terminal diagnosis. Now, while we want to act and do everything we can to dampen thyroid autoimmunity, it’s also important that we realize that the level of positivity is important to take into consideration.
This study hints that those with high levels of thyroid autoimmunity have poor outcomes. Specifically, the average level of TPO positivity here was 1,122. It’s important to keep this in mind, because if you only read the conclusion of this paper, you would erroneously think that having TPO antibodies above 100 was correlated with poor psychological and physical well-being. However, as you can see in the write-up here, the researchers simply defined being positive for Hashimoto’s as having TPO antibodies above 100.
So what they’re actually saying in their conclusion in that those that had Hashimoto’s had poor psychological and physical well-being, but it was actually at an average level of 1,122 wherein that poor psychological and physical well-being was documented. So how this all translates back to day-to-day practice and a conservative and cost-effective model of functional medicine said quite simply is, if someone has a low-level positivity of thyroid autoimmunity, we may not need to continue treating the thyroid autoimmunity.
The specifics of exactly what a low level of thyroid autoimmunity is are not totally clear, but we can draw some inferences from the data that someone in the low hundreds may be considered a clinical win, based upon my opinion, which is based upon the best evidence we have to answer this question at this point in time.
Hydrogen sulphide in exhaled breath: a potential biomarker for small intestinal bacterial overgrowth in IBS.
https://www.ncbi.nlm.nih.gov/pubmed/27163246
Study purpose
- Assess the utility of hydrogen sulfide (H2S) breath testing for suspected SIBO compared to the traditional SIBO breath test.
Intervention:
- 151 subjects with IBS-D (via Rome III) were enrolled and tested with glucose-hydrogen breath test, small bowel culture, and breath H2S.
Main Results:
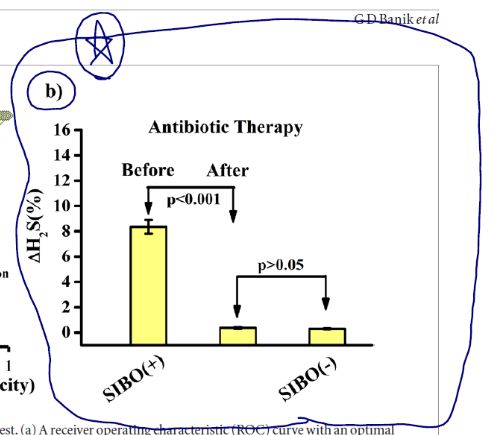
- SIBO breath test positive patients also had higher levels of breath H2S.
- However, those with IBS-D and who were SIBO breath test negative had higher breath levels of H2S.
- Antibiotic therapy led to a decrease in breath H2S and an improvement in symptoms – Figure b).
Additional Results:
- “Individuals with ΔH2S% ⩾76% at t = 45 min were considered to be SIBO positive.”
- H2S change of 1.76% by 45 minutes = positive for H2S SIBO
- “… and this corresponded to 93.6% sensitivity and 89.4% specificity with 91.3% diagnostic accuracy (95% confidence interval).”
- “We found the diagnostic PPV and NPV of 98% and 91%, respectively between the IBS patients with SIBO and without SIBO.”
Authors’ Conclusion:
- “We have shown that breath H2S can be used as a potential molecular marker for non-invasive evaluation of SIBO and even after in response to the standard eradication therapies of the bacterial overgrowth.”
Interesting Notes:
- H2S is highly toxic to the gut and is produced by hydrogen consuming microbes.
- H2S production might contribute to IBS.
- H2S is released in the breath.
Clinical Takeaways:
- H2S (hydrogen sulfide) SIBO may be present in those with IBS, but who are negative via hydrogen SIBO breath test.
Dr. Ruscio’s Comments
In those with IBS or IBS-like symptoms who are then tested for SIBO and negative, it can be a bit disheartening. This study provides a novel finding, wherein we might be able to provide patients with a cause of their IBS or IBS-like symptoms. That cause may be hydrogen sulfide SIBO. So when traditional hydrogen breath testing is negative, hydrogen sulfide might be positive and might be the underlying cause of the IBS or IBS-like symptoms.
Now, in this study, the authors chose IBS-D, or diarrhea-type IBS, because it’s more prevalent. However, we don’t know if this same finding will apply for IBS-C, or a constipation-type IBS. I would be inclined to think that it would, but we don’t know that for a fact. Another very important thing about this study, and something that ties back to what you do with this information in the clinic, is that when treated with standard antibiotic therapy, the levels of hydrogen sulfide in the breath decreased. And that also correlated with an improvement in symptoms in subjects.
So this tells us that even though we can’t necessarily test for hydrogen-sulfide SIBO at present, we can treat with antibiotics, and I would speculate the same would apply for herbal antimicrobial therapy, and we’d see a positive impact on the hydrogen sulfide in the breath that also correlates with an improvement in symptoms.
So remember not to fall into the trap that you would need to have a test in order to treat. If you performed a, what I would recommend, lactulose hydrogen methane SIBO breath test, and that came back negative, someone may still be a candidate for treatment because they may have hydrogen-sulfide SIBO.
Now, I think we can make a better case for initially treating with herbal medicines because they may be a bit milder and a bit safer than antibiotics. But, in any case, this is a nice reminder that we don’t need to have a test in order to treat something. Testing can be helpful, but again, this study shows us that in patients with IBS-D, that are negative for traditional SIBO testing, they may have hydrogen sulfide as the root cause. And treatment with standard antibiotic therapy has been shown to prove that hydrogen sulfide positive test correlates with their symptoms.
So if we can’t do the testing, but we see the symptoms, and we treat the symptoms, and the symptoms get better, that may indirectly tell us that we’ve had a favorable impact on hydrogen sulfide in the gut.
Selenium supplementation could restore euthyroidism in subclinicalhypothyroid patients with autoimmune thyroiditis.
https://www.ncbi.nlm.nih.gov/pubmed/28042649
Study purpose
- Randomized controlled prospective study to investigate the effects of selenium treatment on patients with autoimmune thyroiditis and mild sub-clinical hypothyroidism (TSH < 10 mU/L).
Intervention:
- Patients with autoimmune thyroiditis and mild sub-clinical hypothyroidism received 83 mcg selenomethionine per day, orally for four months.
- Roughly 80 cases versus 80 controls
Main Results:
- 3% of treated patients (cases) restored normal thyroid function
- 1% of non-treated controls restored normal thyroid function
Additional Results:
- The average TPO level was ~460 U/mL (cases 447 ± 108 vs. controls: 480 ± 140, mean ± SD U/mL).
- The response in thyroid function did not appear to be due to improvement in thyroid autoimmunity. Both the responders and non-responders saw a decrease in TPO, but only the responders restored normal TSH.
Authors Conclusion:
- “Selenium supplementation could restore euthyroidism in one third of subclinical hypothyroidism patients with autoimmune thyroiditis.”
Interesting Notes:
- “Treatment with levothyroxine has been recommended for all subclinical hypothyroid patients with TSH levels > 10 mU/L, whereas for those with TSH < 10 mU/L treatment remains controversial.”
- “when children with iodine and selenium deficiencies were supplemented with selenium alone, which led to thyroid destruction and myxoedematous cretinism, suggesting that selenium should not be supplemented prior to correction of the iodine deficit.”
- Up to 62% of subclinical hypothyroid patients will spontaneously remit. The chances of remission are increased if TSH <10 and there is no thyroid autoimmunity.
- “Spontaneous recovery has been recorded in patients affected by HT with subclinical hypothyroidism, although the frequency of this phenomenon is unclear [11, 12]. Diezz et al. showed that during a five-year follow-up period, TSH levels became normal in the absence of treatment in 62% of patients. However, normalization of serum TSH concentrations is more likely to occur in patients with negative antithyroid antibodies, TSH serum levels of < 10 mU/I, and within the first two years of diagnosis [13].”
- Another study has also found selenium can correct subclinical hypothyroid, and that the addition of Myo-Inositol might enhance the effect. https://www.ncbi.nlm.nih.gov/pubmed/24224112
- Some evidence suggests that those in countries with lower selenium supply will see decreased TPO levels from supplementation and those who are in sufficient countries will not.
Clinical Takeaways:
- “Selenium supplementation could restore euthyroidism in one third of subclinical hypothyroidism patients with autoimmune thyroiditis.”
Dr. Ruscio’s Comments
This study provides a few important insights regarding subclinical hypothyroid. Now, remember that subclinical hypothyroid is defined as high TSH paired with normal T4, according to the conventional ranges. This study showed a 30% rate of correction of subclinical hypothyroid after the administration of only about 80 micrograms of selenium, so that’s very encouraging. What else is interesting is that the time interval here was about four months.
Now, based upon some of the other research that we’ve discussed, the studies hint that most, if not all, of the benefit from selenium supplementation will occur by three to six months of supplementation, so this is in alignment with that.
Also, it’s interesting to consider that those in countries with a low selenium supply may respond more in terms of their TPO antibodies to selenium supplementation than those in countries with adequate selenium supply. So this reinforces that the impact of selenium is because of a repletion of an insufficiency. And this also hints at, or supports, the thinking that selenium should not be taken in perpetuity, but rather be taken in a shorter term so as to replete an insufficiency. This is again likely why we see most of the improvement from selenium being realized after three to six months of supplementation.
What else is interesting here is that in this study, the average TPO antibody was roughly 460, and that the improvements seen in the TSH from selenium supplementation did not appear to be caused by improvements in TPO. Why is this? It’s likely because a TPO of 460 is not highly abnormal, and might be considered a clinical win. So there might be a different mechanism, other than improvement in thyroid autoimmunity, that’s accounting for the improvement in TSH, again likely because the average level of TPO antibodies being 460 may not be considered abnormal or highly abnormal.
Another important note is to replete selenium and iodine at the same time in those who are iodine insufficient. It’s easy to assume, as I used to, that we may want to start selenium first so as to try to quell any flaring of autoimmunity initiated by iodine supplementation. However, this study made an interesting remark that, at least in one study, iodine has been shown to make people worse. And so the better approach is to replete both iodine and selenium at the same time.
Also, remember that this study makes an important point that about 60% of those with subclinical hypothyroidism will spontaneously remit, so we don’t need to be overzealous and pointing out to a patient that we found something and that they might have a disease. In fact, there’s a majority probability that this is just an inconsequential finding and that they will revert back to normal if we did nothing else and just let some time pass.
Now, you have a higher chance of spontaneous remission or just remission if there’s no autoimmunity present and that the TSH is below 10. So factor that into whether or not you decide to give a patient supplemental selenium that has subclinical hypothyroid. If someone has no antibodies and has a TSH below 10, they may not even need the selenium supplementation. If they have thyroid autoimmunity and a TSH above 10, then the supplementation and other actions to improve our immunity may make more sense or be more justified.
And then regarding testing, do we need to test? I don’t think so. We certainly can make a case for it. But because there’s no definitive data that tells us a certain level of selenium deficiency will predict a positive response to selenium supplementation, it’s probably most efficient to try a short-term conservative trial of selenium supplementation, and leave it at that.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!