Practitioner Case Study – January 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Low FODMAP versus prebiotics in IBS, a head-to-head-trial.
- Anti-Thyroperoxidase Antibody Levels >500 IU/ml Indicate a Moderately Increased Risk for Developing Hypothyroidism in Autoimmune Thyroiditis.
- Gut-to-brain or brain-to-gut, which pathway is more important?
- Using SIBO breath testing to predict response to antibiotics in patients with IBS.
- An evidence based thyroid questionnaire.
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Marry, 46yo female.
- Previous dx: GERD, SIBO, Tachycardia, esophageal stricture
- Chief complaints:
Visit 1 (4/27/16) – History and Exam:
Mary presents as a generally healthy 46yo female who has a good diet and lifestyle. She has experienced a slow progression of her chief complaints. Her reflux/heartburn dates back to 18yoa.
Her symptoms are manageable with diet (low FODMAP/Fast Tract combo) and supplements (glutamine, enzymes) however she is still symptomatic. Her bowel regularity/consistency became worse after Abx, most notably after SIBO Abx, and subsequent Habx (herbal antimicrobials) may have also provoked it.
She reacts negatively to HCl. She also noted ‘the better she eats the worse she feels’.
Initial impression
- Mary may have dysbiosis secondary to antibiotics (C. diff, candida, etc…). The negative reaction to HCl, heartburn, bloating and nausea may also suggest gastritis or even an ulcer. The esophageal stricture may be caused by the reflux/heartburn. The emotional instability and inability to handle stress may indicate female hormone imbalance and/or fatty acid imbalance.
Visit 2 (a few days later, 5/4/16) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Glucose SIBO breath test
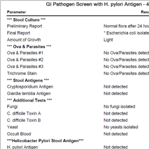
- BioHealth 401H
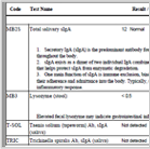
- Diagnostechs custom panel
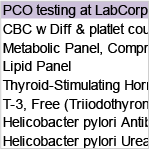
- Blood panel
Recommendations
- Continue with previous diet (low FODMAP/Fast Tract combo)
- Modified fasting (using bone broth or Masters Cleanse) and elemental/semi-elemental diet experimentation – 2-4 day trial
- Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- – Note: Curcumin may protect esophageal cells for dysplastic changes. Vitamin D has been shown helpful in IBS. Emotional instability may be due to fatty acid deficiencies.
- Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- GI:
- – Natural prokinetic, probiotics (lacto/bifido blend, S. boulardii, soil based),
- – Natural acid lowering compound (melatonin, vitamins, and amino acids)
Visit 3 (2 months later, 7/13/16) – Lab Interpretation and Treatment Evaluation
Lab interpretation:
- Lab finding are unremarked, see below
- – Aerodiagnostics Glucose SIBO breath test – negative
- – BioHealth 401H – normal
- – Diagnostechs custom panel – normal
- – Blood panel – generally normal
Subjective Assessment:
- Fasting – Mary did not respond well to any fasting intervention; she experienced a regression of heartburn and stomach upset.
- Improved:
- – Heartburn
- – Moderately improved PMS and brain fog
- – Bloating & nausea
- – Alternating loose stools/diarrhea
- Worse:
- – Natural acid lowering compound – caused fatigue and was not tolerated
- – Attempting reintroduction of gluten free flours and starches caused general regression (I did not instruct this but Mary decided to experiment).
- Overall – 75% improved subjectively. Mary also commented that she wasn’t sure if the probiotics were helping her.
Impression:
- The negative response to fasting reinforces reflux, ulcerations, and/or gastritis. This should make Mary a good candidate for acid lowering interventions; unfortunately she was unable to tolerate the first formula we tried. Her response to a natural prokinetic was therefore not surprising.
- Her PMS and brain fog improving suggests the fatty acids and hormone support were needed. Note: there is no need to test hormones when using herbs that have an adaptogenic effect on balancing female hormones as we did. A great place to save a patient money.
- Overall Mary is moving in the right direction.
Recommendations:
- Discontinue the natural acid lowering compound. Avoid starches and GF flours as best you can. Discontinue any modified fasting or use of elemental/semi-elemental diet formulas.
- Continue previous program:
- – Diet (low FODMAP/Fast Tract combo)
- – Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- – Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- – GI:
- – Natural prokinetic, probiotics (lacto/bifido blend, S. boulardii, soil based)
- Maintain this program for now, follow up in 2 months.
Visit 4 (2 months later, 9/16/16):
Subjective Assessment:
- Improved:
- – Mary had generally maintained her previous improvements with the following exceptions
- Worse
- – Runny nose even though not sick, abdominal pain, nausea, anxiety, palpitations
- Mary also reported again ‘she feels better the worse she eats’. She also noted that when she eats lots of fermented foods and/or Kombucha she seems to feel worse.
Impression:
- The fact that Mary was experiencing a flare of runny nose (even though not sick), abdominal pain, nausea, anxiety, and palpitations are highly suggestive of histamine overload. She also reported that too much fermented food intake seems to flare her. This further suggest histamine overload. So we had her follow a low histamine diet and discontinued all probiotics (which are a source of histamine) while maintaining her previous treatments listed above.
Recommendations
- Follow a low histamine diet and discontinue all probiotics while maintaining your previous program. Follow up in 4-8 weeks.
Visit 5 (10/28/16):
Subjective Assessment:
- Improved:
- – Stomach pain, reflux, runny nose, stools, bloating, brain fog
- Mary felt the low histamine diet was very helpful. She also noticed the both the lacto/bifido probitic AND the soil based probiotic caused negative reactions, but the S. boulardii was OK.
Impression:
- Reducing Mary’s histamine load was very helpful and was the last piece needing to be addressed to reach full symptomatic resolution.
- The fact she had been off a natural acid lowering agent suggests this was not needed for reflux/heartburn, stomach pain. Interestingly, histamine is involved in gastric acid secretion so by improving/reducing her histamine load we likely address the root cause of any hyperacidity that might be present. It is important to encourage Mary to adhere to whatever follow up her conventional GI is recommending to make sure someone is keeping tabs on any potential histological changes in the esophagus. Hopefully our work together will ensure her esophageal histology improves, but we shouldn’t leave this to chance.
Recommendations:
- Continue previous program
- – Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- – Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- – GI:
- – Natural prokinetic, probiotics (S. boulardii)
- But make the following changes
- – Work to expand your dietary boundaries both with your FODMAP/Fast Tract restrictions and with your histamine restrictions
- Follow up in 2 months
Visit 6 (12/30/16):
Subjective Assessment
- Mary has maintained all previous improvements and even reports she feels slightly better.
- She has been able to slightly expand her dietary boundaries.
Impression:
- Mary has done great, no more improvement is needed. We can maintain this program for a few more months and then start on curtailing her off the items in her current program to find minimal maintenance plan.
Recommendations:
- Follow up in 2-3 months
Dr. Ruscio’s Comments
When Mary came into my office she had already treated SIBO, but this treatment appeared to make her bowels worse. At her exam she did present with symptoms that could be consistent with SIBO; however, her labs did not support this, nor did they support any other dysbiosis, or other metabolic abnormalities. She also exhibited symptoms consistent with ulcer/gastritis and female hormone imbalances.
She responded well to initial treatment with botanicals for female hormone balancing, and herbal upper GI prokinetic. She did not respond well to fasting-type interventions (which reinforces an ulcer/gastritis/hyperacidity). The effect of probiotics was difficult to ascertain initially. At her subsequent follow up visits Mary started to experience symptom regressions that can be consistent with histamine overload (anxiety, brain fog, runny nose, palpitations). We then had her follow a low histamine diet and discontinue all probiotics (most probiotics being a source of histamine) – she responded very well. Also remember that histamine signals HCl release, so this modification may have been all that was needed to address gastritis/ulceration/hyperacidity – the fact that her symptoms were improved further reinforces this. The above was the combination of factors that Mary needed to achieve satisfactory improvement in all/most of her symptoms. She is thrilled with her results.
This case could have been made more complicated with methylation testing, neurotransmitter evaluations, female hormone assays, HCl/pH assessment, endoscopy, etc., but they were not needed. We focused on practical, clinical fundamentals and achieved excellent results at a small cost and in a short time period.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!