Patient Info:
- Marry, 46yo female.
- Previous dx: GERD, SIBO, Tachycardia, esophageal stricture
- Chief complaints:
Visit 1 (4/27/16) – History and Exam:
Mary presents as a generally healthy 46yo female who has a good diet and lifestyle. She has experienced a slow progression of her chief complaints. Her reflux/heartburn dates back to 18yoa.
Her symptoms are manageable with diet (low FODMAP/Fast Tract combo) and supplements (glutamine, enzymes) however she is still symptomatic. Her bowel regularity/consistency became worse after Abx, most notably after SIBO Abx, and subsequent Habx (herbal antimicrobials) may have also provoked it.
She reacts negatively to HCl. She also noted ‘the better she eats the worse she feels’.
Initial impression
- Mary may have dysbiosis secondary to antibiotics (C. diff, candida, etc…). The negative reaction to HCl, heartburn, bloating and nausea may also suggest gastritis or even an ulcer. The esophageal stricture may be caused by the reflux/heartburn. The emotional instability and inability to handle stress may indicate female hormone imbalance and/or fatty acid imbalance.
Visit 2 (a few days later, 5/4/16) – Testing and Initial Recommendations
Testing
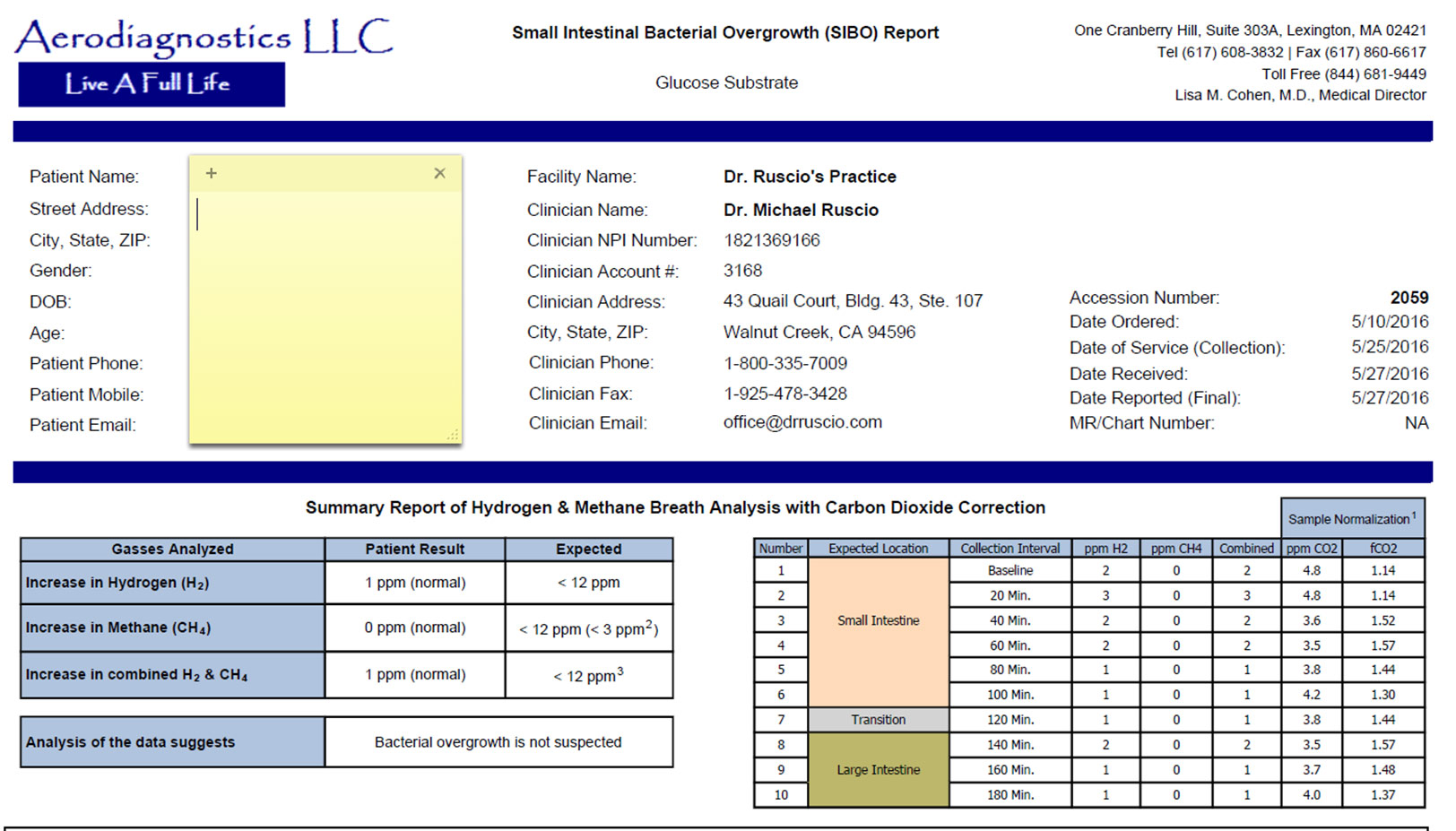
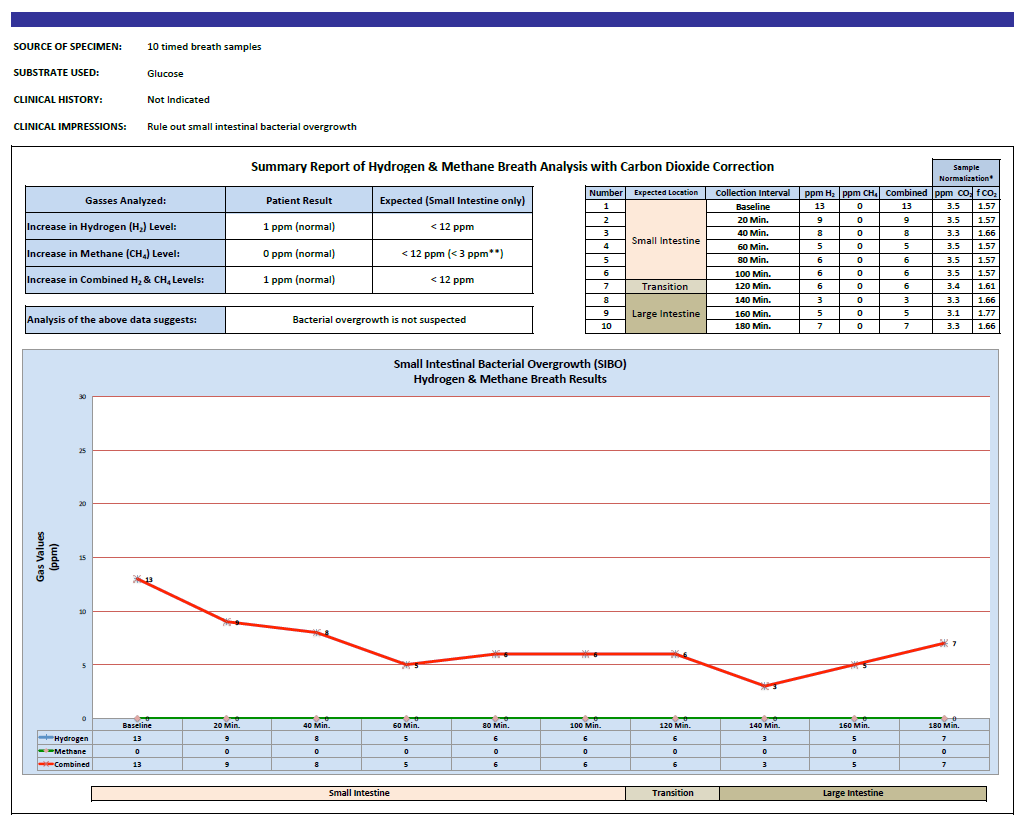
- Aerodiagnostics Glucose SIBO breath test
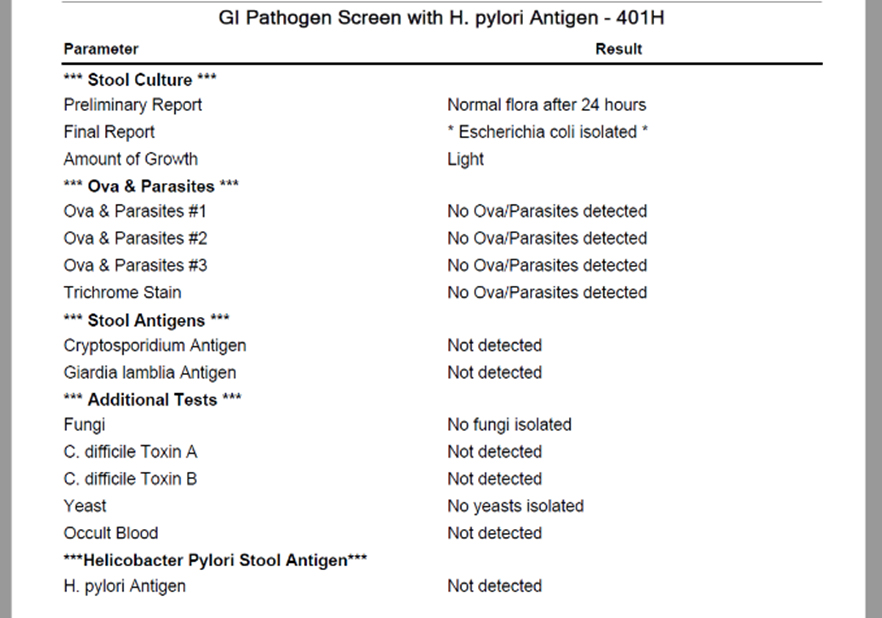
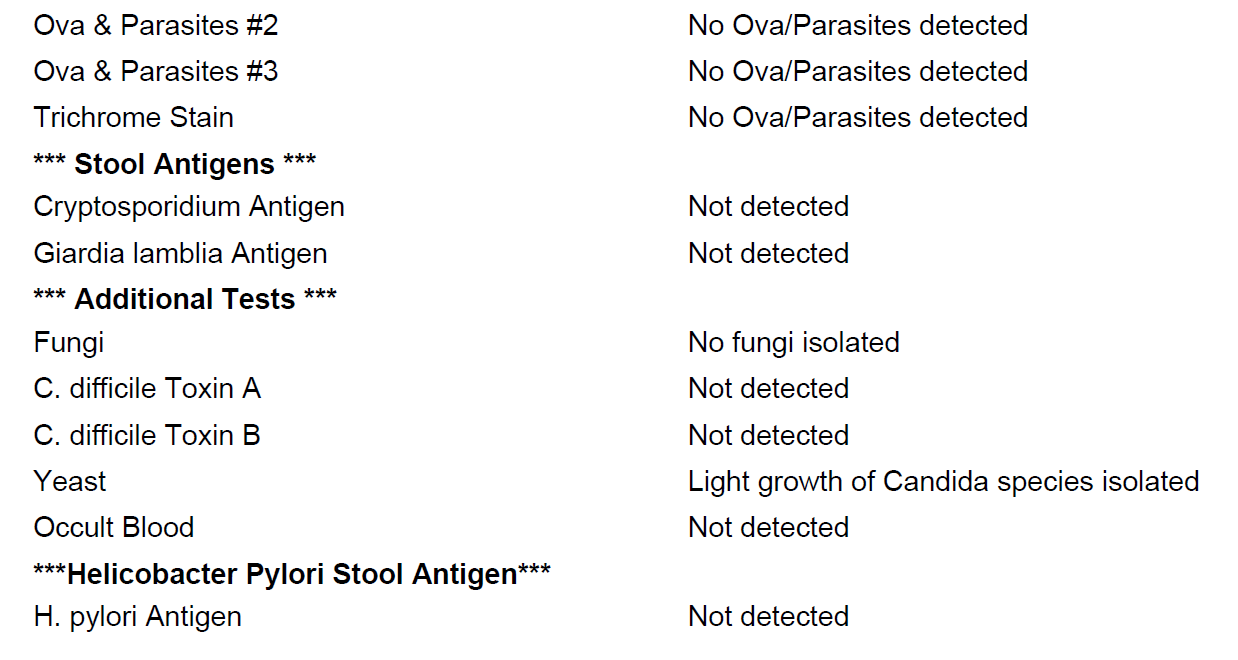
- BioHealth 401H
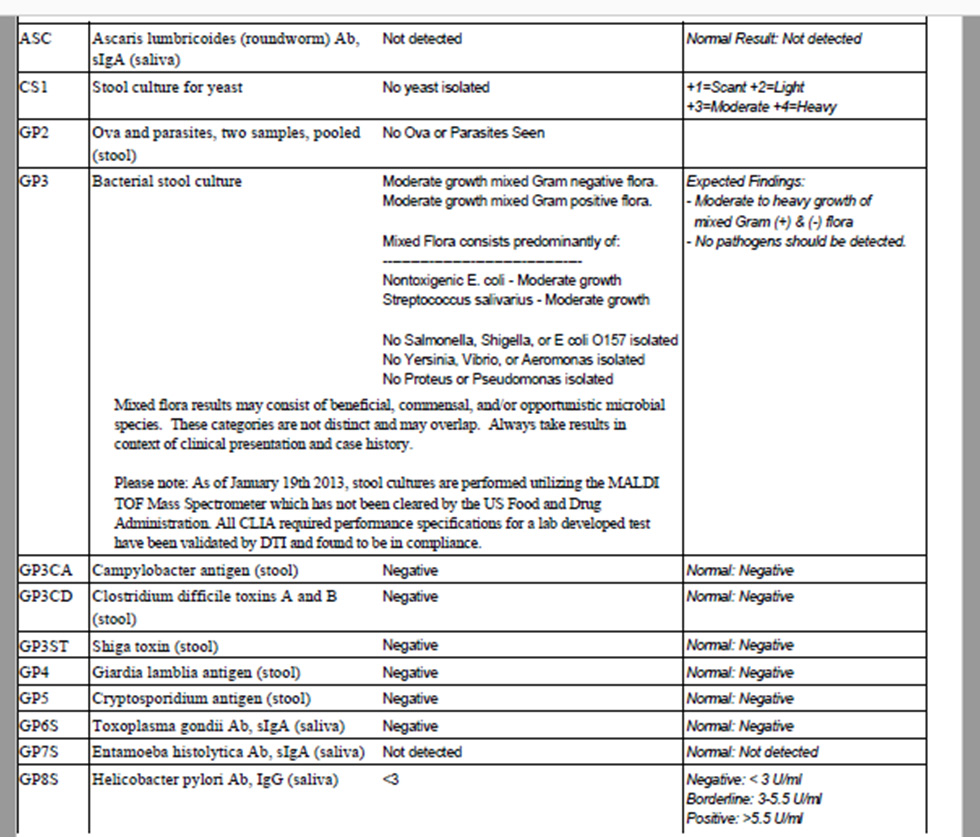
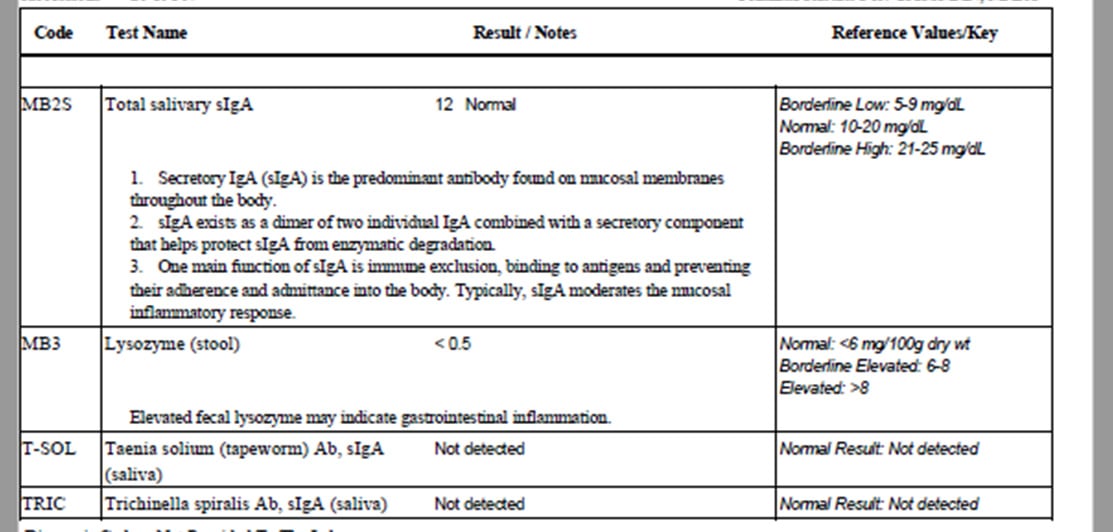
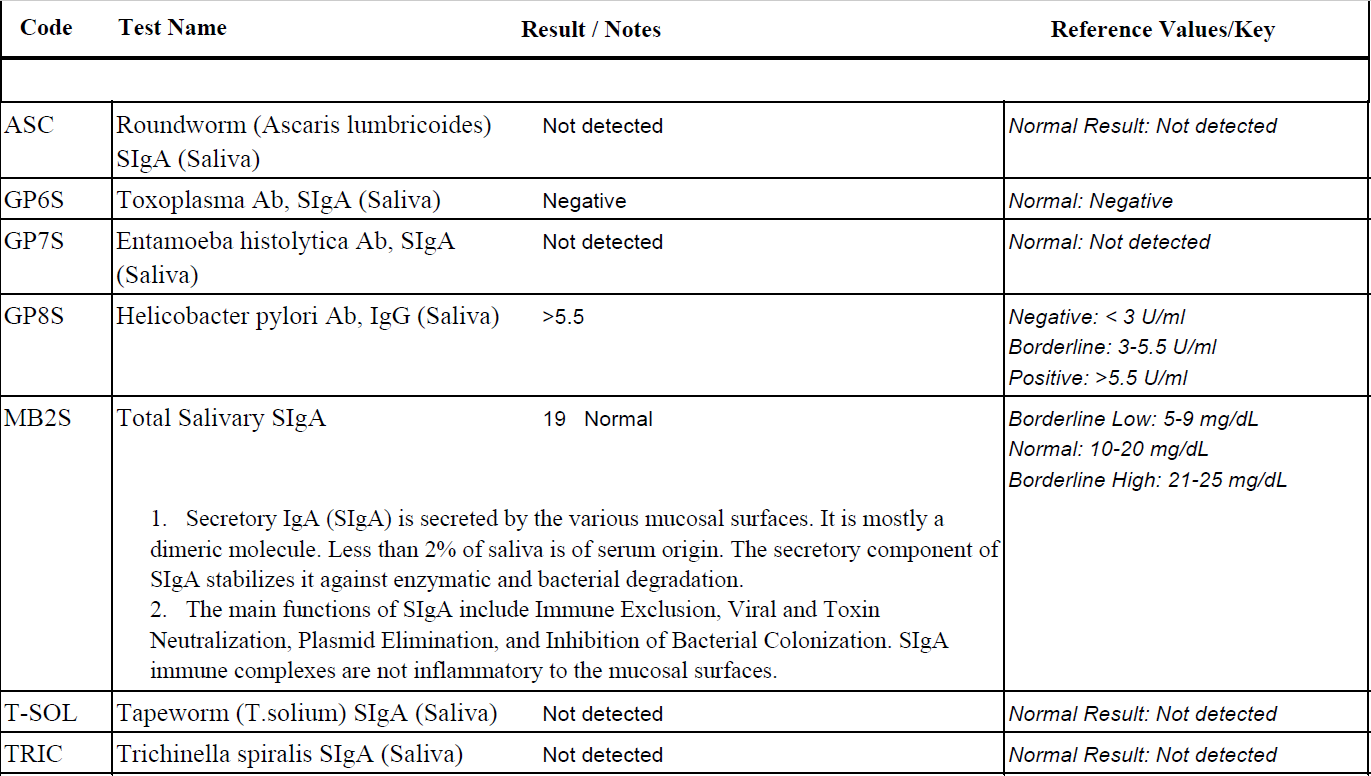
- Diagnostechs custom panel
- Blood panel
Recommendations
- Continue with previous diet (low FODMAP/Fast Tract combo)
- Modified fasting (using bone broth or Masters Cleanse) and elemental/semi-elemental diet experimentation – 2-4 day trial
- Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- Note: Curcumin may protect esophageal cells for dysplastic changes. Vitamin D has been shown helpful in IBS. Emotional instability may be due to fatty acid deficiencies.
- Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- GI:
- Natural prokinetic, probiotics (lacto/bifido blend, S. boulardii, soil based),
- Natural acid lowering compound (melatonin, vitamins, and amino acids)
Visit 3 (2 months later, 7/13/16) – Lab Interpretation and Treatment Evaluation
Lab interpretation:
- Lab finding are unremarked, see below
- Aerodiagnostics Glucose SIBO breath test – negative
- BioHealth 401H – normal
- Diagnostechs custom panel – normal
- Blood panel – generally normal
Subjective Assessment:
- Fasting – Mary did not respond well to any fasting intervention; she experienced a regression of heartburn and stomach upset.
- Improved:
- Heartburn
- Moderately improved PMS and brain fog
- Bloating & nausea
- Alternating loose stools/diarrhea
- Worse:
- Natural acid lowering compound – caused fatigue and was not tolerated
- Attempting reintroduction of gluten free flours and starches caused general regression (I did not instruct this but Mary decided to experiment).
- Overall – 75% improved subjectively. Mary also commented that she wasn’t sure if the probiotics were helping her.
Impression:
- The negative response to fasting reinforces reflux, ulcerations, and/or gastritis. This should make Mary a good candidate for acid lowering interventions; unfortunately she was unable to tolerate the first formula we tried. Her response to a natural prokinetic was therefore not surprising.
- Her PMS and brain fog improving suggests the fatty acids and hormone support were needed. Note: there is no need to test hormones when using herbs that have an adaptogenic effect on balancing female hormones as we did. A great place to save a patient money.
- Overall Mary is moving in the right direction.
Recommendations:
- Discontinue the natural acid lowering compound. Avoid starches and GF flours as best you can. Discontinue any modified fasting or use of elemental/semi-elemental diet formulas.
- Continue previous program:
- Diet (low FODMAP/Fast Tract combo)
- Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- GI:
- Natural prokinetic, probiotics (lacto/bifido blend, S. boulardii, soil based)
- Maintain this program for now, follow up in 2 months.
Visit 4 (2 months later, 9/16/16):
Subjective Assessment:
- Improved:
- Mary had generally maintained her previous improvements with the following exceptions
- Worse
- Runny nose even though not sick, abdominal pain, nausea, anxiety, palpitations
- Mary also reported again ‘she feels better the worse she eats’. She also noted that when she eats lots of fermented foods and/or Kombucha she seems to feel worse.
Impression:
- The fact that Mary was experiencing a flare of runny nose (even though not sick), abdominal pain, nausea, anxiety, and palpitations are highly suggestive of histamine overload. She also reported that too much fermented food intake seems to flare her. This further suggest histamine overload. So we had her follow a low histamine diet and discontinued all probiotics (which are a source of histamine) while maintaining her previous treatments listed above.
Recommendations
- Follow a low histamine diet and discontinue all probiotics while maintaining your previous program. Follow up in 4-8 weeks.
Visit 5 (10/28/16):
Subjective Assessment:
- Improved:
- Stomach pain, reflux, runny nose, stools, bloating, brain fog
- Mary felt the low histamine diet was very helpful. She also noticed the both the lacto/bifido probitic AND the soil based probiotic caused negative reactions, but the S. boulardii was OK.
Impression:
- Reducing Mary’s histamine load was very helpful and was the last piece needing to be addressed to reach full symptomatic resolution.
- The fact she had been off a natural acid lowering agent suggests this was not needed for reflux/heartburn, stomach pain. Interestingly, histamine is involved in gastric acid secretion so by improving/reducing her histamine load we likely address the root cause of any hyperacidity that might be present. It is important to encourage Mary to adhere to whatever follow up her conventional GI is recommending to make sure someone is keeping tabs on any potential histological changes in the esophagus. Hopefully our work together will ensure her esophageal histology improves, but we shouldn’t leave this to chance.
Recommendations:
- Continue previous program
- Nutritional support: curcumin, vitamin D/K, Magnesium, Omega 3, 6, 9 blend
- Hormonal: female hormone support herbal blend (black cohosh, dong qui, chaste tree)
- GI:
- Natural prokinetic, probiotics (S. boulardii)
- But make the following changes
- Work to expand your dietary boundaries both with your FODMAP/Fast Tract restrictions and with your histamine restrictions
- Follow up in 2 months
Visit 6 (12/30/16):
Subjective Assessment
- Mary has maintained all previous improvements and even reports she feels slightly better.
- She has been able to slightly expand her dietary boundaries.
Impression:
- Mary has done great, no more improvement is needed. We can maintain this program for a few more months and then start on curtailing her off the items in her current program to find minimal maintenance plan.
Recommendations:
- Follow up in 2-3 months
Dr. Ruscio’s Comments
When Mary came into my office she had already treated SIBO, but this treatment appeared to make her bowels worse. At her exam she did present with symptoms that could be consistent with SIBO; however, her labs did not support this, nor did they support any other dysbiosis, or other metabolic abnormalities. She also exhibited symptoms consistent with ulcer/gastritis and female hormone imbalances.
She responded well to initial treatment with botanicals for female hormone balancing, and herbal upper GI prokinetic. She did not respond well to fasting-type interventions (which reinforces an ulcer/gastritis/hyperacidity). The effect of probiotics was difficult to ascertain initially. At her subsequent follow up visits Mary started to experience symptom regressions that can be consistent with histamine overload (anxiety, brain fog, runny nose, palpitations). We then had her follow a low histamine diet and discontinue all probiotics (most probiotics being a source of histamine) – she responded very well. Also remember that histamine signals HCl release, so this modification may have been all that was needed to address gastritis/ulceration/hyperacidity – the fact that her symptoms were improved further reinforces this. The above was the combination of factors that Mary needed to achieve satisfactory improvement in all/most of her symptoms. She is thrilled with her results.
This case could have been made more complicated with methylation testing, neurotransmitter evaluations, female hormone assays, HCl/pH assessment, endoscopy, etc., but they were not needed. We focused on practical, clinical fundamentals and achieved excellent results at a small cost and in a short time period.
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome.
https://www.ncbi.nlm.nih.gov/pubmed/27747984
Study purpose:
- To evaluate the effect of a low FODMAP diet compared to a diet high in prebiotics on IBS symptoms and related co-morbidities.
- Markers tracked
Intervention (double blinded):
- 20 patients with IBS (IBS-D and IBS-M) followed a low FODMAP (LFD) diet for 3 weeks, then
- ½ patients received 16g/day of FOS prebiotics, the other ½ received a placebo as maltodextrin
- Then all patients performed another 3 weeks on low FODMAP
- Then the groups were switched – ½ patients reviewed FOS and the other ½ received maltodextrin
Results:
- “There was a significant improvement in all IBS symptoms after 3 weeks of LFD”
- “…an overall patient satisfaction of 85%” was reported on the low FODMAP diet
- Those on the low FODMAP diet also experienced a significant improvement in
- When then transitioning to either placebo or FOS
- When on FOS, patients experienced a worsening of
Additional results:
- Cytokines: A reduction in inflammatory cytokines was noted in those on the low FODMAP diet, but not for those on FOS. Specifically IL-6 and IL-8.
- Microbiota: Paradoxically, patients became slightly more dysbiotic while on low FODMAP but then slightly less dysbiotic when on FOS. This included a reduction of Bifidobacterium.
- SCFAs: low FODMAP caused a slight reduction
Authors’ Conclusion:
- “Our findings support the efficacy of a LFD in alleviating IBS symptoms, and show changes in inflammatory cytokines, microbiota profile, and SCFAs, which may have consequences for gut health.”
Discussion:
- No specific bacterial changes appeared to correlate with cytokines, SCFAs, or symptoms.
- Bifidobacterium paradox: Bifidobacterium decreased on the low FODMAP diet when symptoms improved, then Bifido increased on FOS when symptoms flared. However, many trials have shown Bifidobacterium probiotics to be one of the most effective probiotics for IBS.
- A few other studies have also showed decreased immune activation on low FODMAP diet, including reductions in histamine. (“Proinflammatory cytokines and histamine are both synthesized and secreted by inflammatory cells”).
- The authors also make an important note that the microbiota rapidly changes based upon diet and that any bacterial loss on low FODMAP could easily be corrected by changing one’s diet i.e. low FODMAP will not cause you to lose bacteria permanently.
Clinical Takeaways:
- The low FODMAP diet is a highly effective intervention for IBS. Prebiotics should be used with caution in IBS.
Dr. Ruscio’s Comments
When we step back and look at all of this, what does it mean? How do we interpret the fact that as symptoms improved and inflammation decreases, we also see a loss of bacteria (including “good bacteria” like Bifidobacterium), a decrease in SCFAs, and patients seem to become more dysbiotic? My thinking is that those with IBS and IBD have an exaggerated immune response against their commensal GI bacteria i.e. their microbiotas. When we feed what the immune system is attacking, we see increased symptoms and inflammation. It might be that, in part, the dysbiosis seen in IBS and IBD is occurring secondary to the overzealous immune system – meaning it’s an adaptation to protect the host. In any case, we can prevent ourselves from making poor clinical decisions if we follow the clinic outcome studies and avoid speculating as to what a good treatment might be based upon observation or mechanism. In this case, while the exact mechanism may be confusing, it’s clear that the low FODMAP diet is effective clinically while prebiotics appear detrimental clinically.
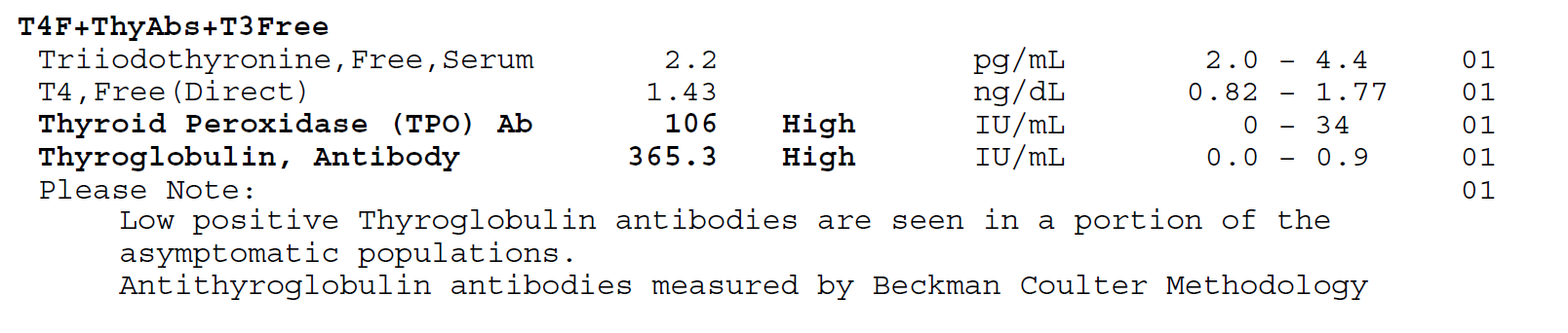
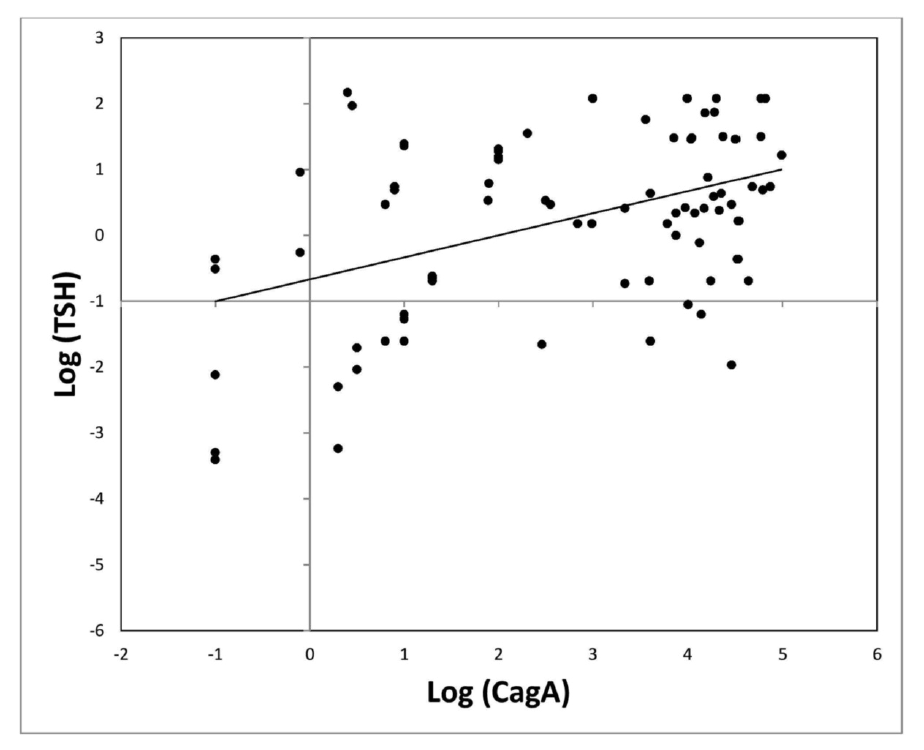
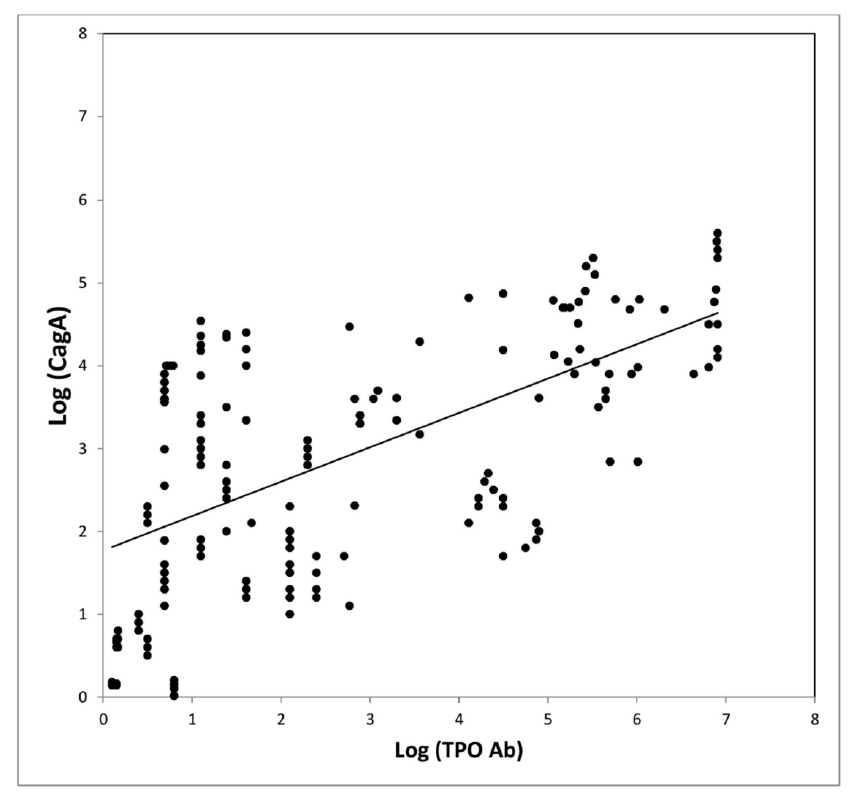
Anti-Thyroperoxidase Antibody Levels >500 IU/ml Indicate a Moderately Increased Risk for Developing Hypothyroidism in Autoimmune Thyroiditis.
http://www.ncbi.nlm.nih.gov/pubmed/27607246
Study purpose:
- “to investigate the association between thyroid antibody levels and the risk for developing hypothyroidism” – essentially to see if thyroid autoimmunity predicts future hypothyroidism.
- TPO and Tg antibodies (thyroperoxidase and thyroglobulin) were assessed in correlation with hypothyroidism (TSH).
Intervention:
- 335 patients were assessed for correlation between thyroid antibodies and hypothyroidism
- 21 of these patients underwent long term monitoring to track association between thyroid autoimmunity and later development of hypothyroidism
Main Results:
Correlation between thyroid antibodies and hypothyroidism
- TPO or Tg antibodies <100 and between 100–500 had no significant different TSH levels.
- TPO >500 was significantly associated with moderate risk for elevations in TSH.
- If TPO AND Tg antibodies were each both above 500, it was also significantly associated with increased elevations in TSH.
- Tg antibodies alone >500 did increase risk elevated TSH but not significantly.
- Dr. R’s Note: this means TPO may be more important in predicting hypothyroidism.
Correlation between thyroid antibodies and future hypothyroidism
- 21 of the 335 patients were tracked for an average of 6.2 years to assess the association between thyroid antibodies and future development of hypothyroid
- No progression toward hypothyroidism was seen for 29% (6/21) of patients
- 71 % (15/21) patients showed progression toward hypothyroidism
- Progression defined as an increase of the TSH level over the time
- However, even though the increase was a statistically significant increase in those with TPO >500, it did not appear to be clinically meaningful. The average TSH increase was 0.5 per 6.2 years
- Which explains why “almost all patients in this group stayed in the euthyroid stage (TSH < 4.6” – meaning almost all patients that progressed toward hypothyroid did not actually become hypothyroid.
- Only one patient became truly hypothyroid after 8.2 years of follow up.
Authors’ Conclusion:
- “Our data indicate largely elevated levels of TPO-Abs being associated with a moderately increased risk of developing hypothyroidism.”
Interesting Notes:
- “Clinically, AIT is among the most common human autoimmune disease with an annual incidence worldwide.”
- Other studies have examined the relationship between thyroid autoimmunity and hypothyroid but this is the first one to assess if the magnitude of autoimmunity impacts the association.
Clinical Takeaways:
- Keeping TPO antibodies below 500 may decrease ones chance of future progression to hypothyroid.
- Tg antibodies appear to have less predictive utility than TPO.
Dr. Ruscio’s Comments
With this study, we make a case for interventions that lower antibodies – this is speculative but reasonable. Also, this information creates a realistic expectation for what pathological versus ‘non-pathological’ levels of antibodies are. For example, I have said that in my observation TPO antibodies between 100-300 are a ‘clinical win’ and that Tg doesn’t appear to be have a clear association. This study reinforces that and expends what a minimal risk level of TPO might be to below 500.
This is an important educating point for your patients because many patients are fearful that any elevation of antibodies is highly pathological. This can create stress and fear and cause patients to pursue more elaborate treatments when they may not be justified. In fact, according to this study’s results, we could speculate that the fear instilled by a clinician mismanaging this conversation could be worse than the actual disease itself. So remember, if someone is feeling well and their TPO antibodies are below 500 they are likely in good shape. Also, remember that this study found that even if someone is above 500 they will only experience roughly a 0.5 elevation in antibodies every 6.2 years. This should be reassuring the patients and clinicians alike.
Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study
http://www.ncbi.nlm.nih.gov/pubmed/27444264
Study purpose:
- To assess which pathway is more influential – the brain-gut connection or the gut-brain connection.
Intervention:
- 1,900 people were prospectively tracked for 1 year to assess if psychological symptoms appeared before GI symptoms or vice versa. Anxiety, depression, IBS, and general quality of life were tracked.
Main Results:
- In 1/3rd of subjects psychological symptoms appeared before GI symptoms
- In 2/3rd of subjects GI symptoms appeared before psychological symptoms
Authors’ Conclusion:
- “While brain–gut pathways are bidirectional, a major subset begin with gut symptoms first and only then psychological distress develops, implicating primary gut mechanisms as drivers of the gut and extra-intestinal features in many cases.”
Discussion:
- “These data suggest low grade gut inflammation in IBS and FD (e.g. via mast cell or eosinophil infiltration) with cytokine release may at least in a subset directly induce the observed psychological comorbidity so deeply characteristic of the syndromes.”
- “the gut likely drives psychological alterations in a major group of cases with FGIDs (functional gastro-intestinal disorders).”
- Not all data agree with the gut-brain connection being more common, http://www.gastrojournal.org/article/S0016-5085(12)62189-1/abstract
- “A new model of a microbe-gene-inflammation interaction, where infection can lead to excessive tumour necrosis factor alpha and other cytokine production in vulnerable individuals is beginning to emerge and may in part explain this gut–brain interaction.”
- “…those whose FGID symptoms that arise primarily from gut pathways will not respond well to psychological therapy, but will respond to gut directed therapies that reverse key abnormalities such as an abnormal microbiome.”
Clinical Takeaways:
- In those with both GI symptoms and anxiety/depression – start with the gut and then reevaluate.
Dr. Ruscio’s Comments
The gut and brain share a bi-directional relationship. Clinically, the question often arises where to start first – the gut or the brain? Much of this will depend on what you find in history and examination, however this study does suggest that starting with the gut may be more important for the majority. It’s also important to remember that not all GI disorders manifest as GI symptoms, so it is possible that if someone had only anxiety/depression (or other neurological symptoms) there still may be a silent GI issue driving this.
Predicting a Response to Antibiotics in Patients with the Irritable Bowel Syndrome
https://www.ncbi.nlm.nih.gov/pubmed/26362282
Study purpose:
- To assess if SIBO breath test results predicted response to antibiotic treatment.
Intervention:
- 561 patients with Rome II diagnosed IBS performed a lactulose breath test. Hydrogen and methane were assessed every 15 minutes for 3.5 hours
- A variety of antibiotics were used, including rifaximin, amoxicillin/clavulanic acid, levofloxacin, doxycycline, ciprofloxacin, neomycin, or metronidazole.
- “A positive response to antibiotics was defined as an improvement in the patient’s global IBS symptoms of at least 50 %”
Main Results:
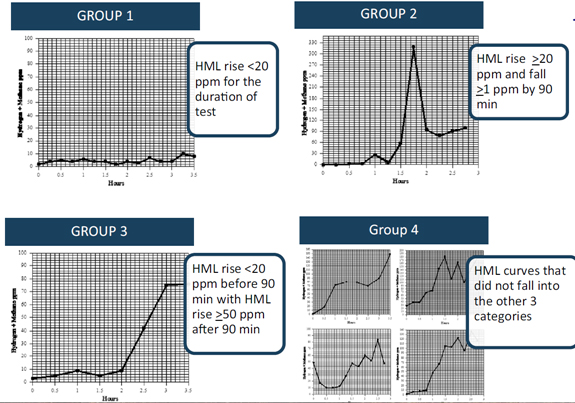
- Test results were broken down into 4 SIBO test presentations
- (Group 1) those whose HML did not increase by >20 ppm throughout the duration of the test
- (Group 2) those with an HML rise >20 ppm with a drop of at least 1 ppm after the initial rise but before 90 min
- (Group 3) those whose HML did not increase by >20 ppm by 90 min but subsequently increased by > 50 ppm
- (Group 4) those graphs that do not fall in one of the aforementioned categories
- Antibiotic response according to group:
- Group 1 = 94.7 % 175
- Group 2 = 81.4 %
- Group 3 = 47.2 %
- Group 4 = 79.9 %
- “… the fact that absence of any rise in gases (group 1) predicted the best response (94.7 % improvement rate) is an unexpected, novel observation.”
Additional Results:
- Ciprofloxacin was most effective treatment, followed by Rifaximin + Neomycin.
Authors’ Conclusion:
- “A lactulose breath test appears to be useful in predicting response to antibiotics in patients with the irritable bowel syndrome. A hydrogen + methane rise <20 ppm throughout the duration of the test is most predictive. This observation contradicts the classic definition of a positive lactulose breath test.” Note: strongest response was in group 1.
Interesting Notes:
- “Antibiotics for presumed small intestinal bacterial overgrowth have been shown to improve irritable bowel syndrome symptoms in at least 40 % of subjects.”
- “About 15 % of the population of North America are thought to suffer from IBS.”
- “… when studies attempted to compare differences in breath tests between patients with IBS and healthy controls, results were disappointing . This is possibly why, when Pimental et al. reported the results of a large multicenter study using rifaximin to treat patients with IBS, breath testing was not used to select patients.”
Clinical Takeaways:
- Those without SIBO may respond symptomatically to antibiotics (or antimicrobials). Those with classical SIBO may also respond. However, those with a ‘false positive’ presentation (group 3) may respond poorly to treatment.
Dr. Ruscio’s Comments
Perhaps the reason why lower gas levels (Group 1) predict a better response to one round of treatment is because if someone has higher gas levels then more than one round of treatment would be needed. This was suggested in another recent study: https://drruscio.com/how-long-should-you-treat-sibo/ .
It’s also important to mention that Group 2, which is more of a classical SIBO presentation, did respond well (81.4%). Additionally, Group 3 responded much less (47.2%), and this is likely because this pattern is more representative of a false + with SIBO. https://drruscio.com/what-is-the-best-test-for-sibo-lactulose-or-glucose-breath-testing/
With all this said, remember that SIBO testing is not the end-all-be-all for IBS treatment. Practical treatment monitoring will likely obtain the best results.
Hypothyroid symptoms and the likelihood of overt thyroid failure: a population-based case–control study
https://www.ncbi.nlm.nih.gov/pubmed/25305308
Study purpose:
- To determine what symptoms are most closely associated with autoimmune hypothyroid.
Intervention:
- Symptoms were compared in new overt autoimmune hypothyroidism (n=140) and thyroid disease-free controls (n=560)
Main Results:
- Hypothyroid patients suffered mostly from
- Tiredness (81%), dry skin (63%), shortness of breath (51%), hair loss (30%)
- “…we identified 13 ‘hypothyroidism-associated symptoms’:
- globulus sensation, difficulty swallowing, anterior neck pain,
- wheezing, shortness of breath, palpitations,
- constipation, hair loss, dry skin, restlessness,
- mood lability, tiredness, and vertigo.”
- Reporting 3 or more of these symptoms was significantly associated with autoimmune hypothyroid
- If fatigue is not present than hypothyroidism is unlikely
- If dry skin is not present than hypothyroidism is unlikely
Additional Results:
- Average Case Result
- TSH = 54.5
- TPO = 4588
- Tg = 131
- Average Healthy Control Result
- TSH = 1.24
- TPO = <30
- Tg = <20
Authors’ Conclusion:
- Paraphrased – symptoms alone do not adequately predict hypothyroidism, so any suspicion should prompt a blood test.
Interesting Notes:
- This study did not assess every possible symptom that could be associated with hypothyroidism, for example, cold intolerance and less sweating were not assessed.
- The overall predictive value of symptoms is low.
Clinical Takeaways:
- Based upon these findings, we can sharpen our intake paperwork’s thyroid section, but any suspicion should be verified by a blood test.
Dr. Ruscio’s Comments
If you would like to sharpen your intake paperwork, you could use these 13 symptoms as your thyroid assessment. I would list fatigue and dry skin first, and be cognizant that the presence of one or both of these two symptoms combined with checking 3 or more total symptoms is a significant predictor.
It’s also interesting to look at the lab values here. TSH was, on average, frankly elevated in these patients. The TPO antibodies were also much higher than the 500 cut-off we discussed in the previous study – which makes sense. However, and as we discussed in the previous study also, Tg antibodies did not seem to correlated with autoimmune hypothyroid.
Marie asks, “Would microbial herbs for SIBO also take care of SIFO?”
Dr. Ruscio’s, DC, Answer:
This is a good question. Technically, we don’t know because we have so little research on SIFO. However, this presents a chance to practice simple empiric medicine – meaning we can use symptomatic change to indirectly tell us if a treatment is addressing SIFO. If you see any of the following, you may want to then consider a course of herbals that are mainly anti-fungal:
- Little or no response to anti-bacterials
- Initial response to anti-bacterials that is then diminished or even regresses to worse than baseline after ending
- Other documentation of yeast/fungus/candida is present; stool culture, microscopy, antibodies
- The patient has a history of yeast infection or oral thrush
- The patient has been successfully treated with anti-fungal in the past
- The patient has a yeast, moldy odor
I typically use a broad spectrum herbal treatment that addresses both bacteria and fungus, so this would be addressing both SIBO and SIFO, or at least we think it would. However, if a patient is highly reactive/sensitive, I will start by using single ingredient anti-bacterials (usually two at a time). If any of the above were noted when using anti-bacterials only (or Rifaximin) then a course of anti-fungals herbs (or anti-fungal Rx) could be warranted. Sometimes very sensitive patients do better with Rx over herbals because there is less to react to in terms of volume to consume and number of compounds they contain.
So in short, yes it’s likely that herbal anti-microbials that are known to be anti-fungal will address SIFO. However, you have to use good clinical observation and monitoring to guide the process.
If you have not made the transition to digital paperwork, here is a company that offers reasonably priced HIPAA compliant digital paperwork. The interface is very easy to use for both office and patients.
Hypothyroid, Hashimoto’s, H. Pylori and Epstein-Barr virus – when to treat and more importantly when not to treat.
Patient Info:
- June, 63yo, female
- Previous dx: hypothyroid
- Rx: 125 mcg Levothyroxine
- Chief Complaints:
Visit 1 (day 1) – History and Exam:
June had previously responded well to the paleo diet, she; lost some weight, had better energy, noted her joint pain went away and that her stomach aches were gone. She also clearly noted she does not do well with dairy or gluten. Even though dietary changes were helpful she then hit a plateau and was left with the above symptoms. She had a family history of Hashimoto’s, suggesting her hypothyroid was due to autoimmunity.
All lifestyle factors seemed to be in good order. She responded very well to thyroid Rx when she had initially started treatment. She also exhibited many signs of adrenal fatigue and female hormone imbalance (fatigue, caffeine dependence, irritability, insomnia, hot flashes, decreased libido, brain fog, vaginal dryness, depression/anxiety).
Initial impression
- I suspected that June had some gastrointestinal dysbiosis, adrenal fatigue, female hormone imbalances and thyroid autoimmunity as the main underlying factors contributing to her sequelae. The fact that she had noted a strong aversion to gluten suggests she may be NCGS, which may increases the chances of subsequent dysbiosis. It also suggest she may need to adhere to more strict avoidance in the long term.
- I was not overly concerned about thyroid hormone conversion or levels since she noted a very positive response to her initial thyroid Rx.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
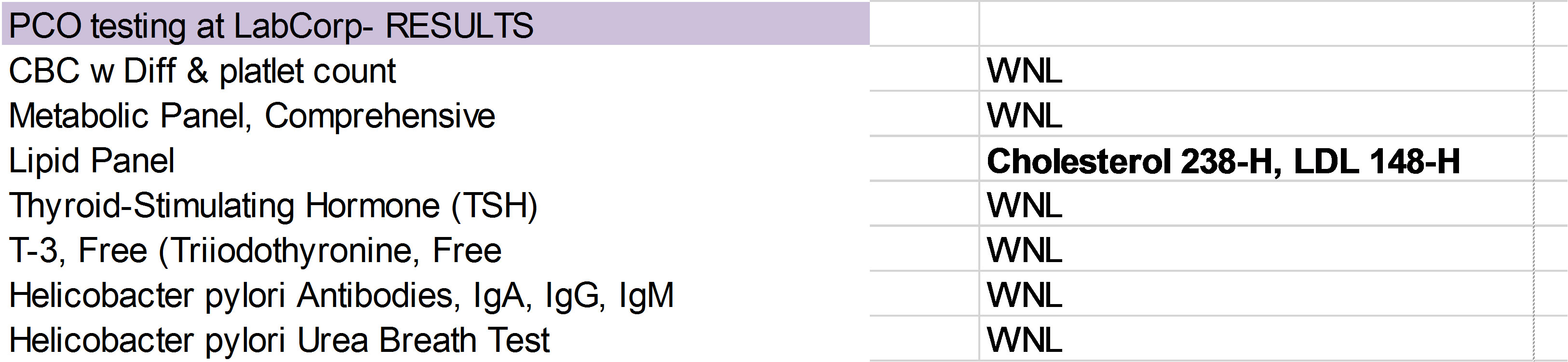
- Custom blood panel, LabCorp
- CBC w Diff & platlet count
- Metabolic Panel, Comprehensive
- Iron Panel: iron, TIBC, Iron Sat., Ferritin
- Thyroid-Stimulating Hormone (TSH)
- Thyroxine, Total (T-4, Total)
- T3, Total (Triiodothyronine, Total)
- rT3
- Homocysteine
- Thyroid Abs
- Diagnostechs select panel of 15 markers
- Medical Diagnostics Laboratories infection panel
Recommendations
- Diet: autoimmune paleo diet
- Hormonal: Bioidentical HRT cream (estrogen/progestogen mixture), adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
Visit 3 (day 30) – Lab Interpretation and Treatment Evaluation
Lab interpretation:
- Custom blood panel
- Unremarked other than Hashimoto’s
- Diagnostechs select panel of 15 markers
- Main finding is H. Pylori
- Medical Diagnostics Laboratories infection panel, main findings (lab image too large to include).
- H. Pylori IgG and IgA positive
- EBV reactivation
Subjective Assessment
- Digestion “way better”
- Improved; energy, sleep, cravings
- Weight loss: 4-5lbs
- Can now tolerate eggs
Impression:
- Dietary changes, adrenal support, female hormone support and digestive support are working nicely. Treatment of H. Pylori and/or EBV may lead to further symptomatic improvement and reduction in thyroid abs. We will start with her GI and then consider anti-viral treatment.
Recommendations
- Maintain previous program
- Diet: autoimmune paleo diet
- Hormonal: Bioidentical HRT cream (estrogen/progestogen mixture), adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
Visit 4 (day 60)
Subjective Assessment:
- Improved
- Energy, way better
- Lost 10lbs total to date
- People are saying she looks great
- Worse:
- Digestion, since starting herbal Abx – bowel changes, stomach aches
- Itching, irritability
Impression:
- Overall we are moving in the right direction as evidenced by the aggregate of her symptomatic findings. However, herbal antimicrobials appear to be causing irritation – which I expected to dissipate once the course was through. I did however recommend she take the remainder of her course of antimicrobials with food to mitigate any reaction.
Recommendations:
- Maintain previous program;
- Diet: autoimmune paleo diet
- Hormonal: Bioidentical HRT cream (estrogen/progestogen mixture), adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- Continue with antimicrobials but take with food instead of on empty stomach.
Visit 5 (day 90)
*June had just previously finished a 2 month course of herbal antimicrobials.
Subjective Assessment:
- Improved
- Weight has now gone from 164 lbs. originally to 151 lbs.
- June has maintained all previous improvements
- The GI irritation, anxiety and irritability have now subsided
- Worse:
- N/A
Impression:
- Any reactions previously were from the antimicrobials and are now cleared. Overall June is doing great. We will wait 60 days to allow antibodies to fall and then retest. We will also have her start on her food reintroduction.
Recommendations:
- Maintain previous program;
- Diet: autoimmune paleo diet
- Hormonal: Bioidentical HRT cream (estrogen/progestogen mixture), adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- Perform dietary reintroduction to normal paleo diet, avoid any foods that cause a negative reaction
- Wait 60 days and then perform retesting
- Perform retesting of LabCorp blood panel
- Retest previous findings from Medical Diagnostic Labs but through LabCorp to utilize insurance
Visit 6 (month 6)
June has now been off antimicrobials for roughly 3 months, and has performed dietary reintroduction.
Lab Findings:
- Retesting of LabCorp blood panel
- fT4 1.47 to 1.85 (high)
- TPO 106 to 103
- TGab 365 to 201
- Retest previous findings from Medical Diagnostic Labs but through LabCorp
- EBV; EA IgG 671, VCA 199, NA >600 *early antigen, viral capsid antigen, nuclear antigen
- HP IgG >8, IgA 16.6
Subjective Assessment:
- Improved
- June has maintained all previous improvements
- Worse
- N/A
- She has noticed she does not do well with nuts or chocolate
Impression:
- Any reactions previously were from the antimicrobials and are now cleared.
- June needs to generally avoid gluten, nuts and chocolate.
- June may need to decrease her thyroid Rx, likely due to enhanced GI absorption. However, June and I decided for us to focus on her gut and thyroid autoimmunity and have her endo make dose adjustments to thyroid Rx as they aredeemed necessary.
- Thyroid autoimmunity has improved slightly. EBV and HP are still positive – hard to gauge if they have improved because we have retested with different lab. Her marked symptomatic improvement make these results less concerning.
- Overall June is doing great but perhaps we can get her thyroid antibodies lower with additional treatment.
Recommendations:
- Maintain previous program
- Diet: autoimmune paleo diet/normal paleo diet hybrid based upon reintroduction
- Hormonal: Bioidentical HRT cream (estrogen/progestogen mixture), adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- Starting a 2-month round of H. Pylori treatment and starting antivirals
- Curtailed H. Pylori treatment: mastic based formula combined with anti-biofilm cocktail
- Antivirals including: monolaurin, Reishi, silver, and quercetin
- Wait 30 days after completing this protocol and then retest (H. Pylori and EBV).
Visit 7 (month 9)
June had recently completed a 2-month round of HP and EBV treatment.
Lab Findings:
- LabCorp retest (H. Pylori and EBV).
- HP IgG >8, IgA 18.4 *essentially no change*
- EBV EA 51.1 *previously was 671, major improvement*
- Note: we retested only the EBV EA (early antigen) as this may be the most important fraction to dictate treatment response.
- Subjective Assessment:
- June has maintained all previous improvements
- She had not noticed any additional improvement with this last round of treatment
Impression:
- June is doing great symptomatically and so we will start to curtail her treatment program, we will start with weaning off the bioidentical hormone support.
- Additional treatment of H. Pylori did not provide any additional benefit to her symptoms nor to her labs, suggesting these levels may be normal for her.
- EBV treatment did lower her EA (early antigen) fraction significantly.
- We need to assess if this has impacted thyroid autoimmunity in the near future. We should also retest HP and EBV antibodies one more time to monitor activity.
Recommendations:
- Continue on this program
- Diet: autoimmune paleo diet/normal paleo diet hybrid based upon reintroduction
- Hormonal: adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- Slowly wean off bioidentical hormone support
- Wait 1.5 months and then retest H. Pylori and EBV again.
Visit 8 (month 11)
Lab Findings:
- LabCorp retest H. Pylori and EBV).
- EBV EA 44.6 *essentially no change*
- HP IgG >8, IgA 23.5 *essentially no change*
Subjective Assessment:
- June has maintained all previous improvements
- Weaned off hormonal support without any problems, is now completely off.
Impression:
- Bioidentical hormone curtail was successful.
- EBV and HP antibody levels appear stable
- We should reassess thyroid autoimmunity now since HP and EBV appear stable.
Recommendations:
- Continue on this program
- Diet: autoimmune paleo diet/normal paleo diet hybrid based upon reintroduction
- Hormonal: adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- Through discussion June and decided that we did not need to retest her thyroid antibodies now since she was doing so well and that we would follow up as needed.
Visit 9 (1 year and 3 months later)
- Overall June is still doing well but she wanted to check back in on H. Pylori, EBV and her thyroid autoimmunity.
- June is also now on a lower dose of thyroid Rx, Levothyroxine 75 mcg.
Lab Findings
We asked June to collect these labs before coming into the office.
- AThyroid-Stimulating Hormone (TSH)
- T-4, Free (Thyroxine, Free)
- T-3, Free (Triiodothyronine, Free)
- 0.130-L
- 1.74
- 2.5
- Epstein-Barr Profile (EBV)
- IgG 198-H, Nuclear IgG >600.0-H, Early Ab IgG 26.8-H *slight improvement*
- Helicobacter pylori Antibodies,
IgA, IgG, IgM - Helicobacter pylori Urea Breath Test
- Thyroid Autoantibodies (TPO and TGA)
- IgG >8.0-H, IgA 20-H,
IgM-normal - Positive Abnormal
- TPO 73-H, Thyroglobulin 310.3-H
Subjective Assessment:
- June has maintained all previous improvements
Impression:
- June is doing great and has even been able to decrease her thyroid Rx dose. In fact she may even be able to decrease her dose further based upon today’s lab findings.
- Her H. Pylori antibodies are essentially unchanged. Her EBV early antigen (EA) has improved slighity, in time and with not treatment.
Recommendations:
- Continue on this program;
- Diet: autoimmune paleo diet/normal paleo diet hybrid based upon reintroduction
- Hormonal: adrenal adaptogenic herbal blend
- GI: Lacto/bifido probiotic, digestive bitters
- June and I discussed trying a protocol of magnesium, selenium, and CoQ10, which had recently been shown to dampen thyroid autoimmunity. We had also decided to treat H. Pylori one more time. We agreed to have her start today on the following:
- Perform 2 month of H. Pylori treatment; herbal antimicrobials, mastica, and S. boulardii.
- Start Mg, Se, CoQ10 and stay on this until our follow up
- Before our next visit perform retesting of H. Pylori and thyroid autoimmunity through LabCorp
Visit 10 (6 months later, from last visit)
June is generally feeling the same, which is very good.
Retesting of H. Pylori and thyroid autoimmunity through LabCorp
- Thyroid-Stimulating Hormone (TSH)
- T-4, Free (Thyroxine, Free)
- Helicobacter pylori Antibodies,
- Helicobacter pylori Urea Breath Test
- Thyroid Autoantibodies (TPO and TGA)
- 0.261- L
- 1.61
- IgA, IgG, IgM – IgG >8.0- H, IgA 20.3-H
- Positive Abnormal
- TPO 76-H, 312-H
Subjective Assessment:
- June has maintained all previous improvements
Impression:
- We reaffirmed June may need less thyroid Rx. She is still on 75 mgc Levo and may even need to decrease her dose again.
- Additional treatment of H. Pylori did not produce any results in her symptoms or her thyroid autoimmunity. H. Pylori is likely functioning as a commensal in June’s microbiota.
- June’s thyroid antibody findings are likely as good as they can get. Regarding TPO antibodies, this level is associated with very minimal risk of progression of hypothyroid. Interpretation of TGab levels are less clear; this level may put her at increased risk for hypothyroid progression, but there is not much else we can treat to improve this. More importantly, the fact that she is needing less thyroid hormone and feeling well is a good prognostic indicator that her thyroid function is improving.
Recommendations:
- Continue on this program
- Diet: autoimmune paleo diet/normal paleo diet hybrid based upon reintroduction
- GI: Lacto/bifido probiotic, digestive bitters
- Discontinue Mg, Se, and CoQ10 protocol. Also slowly wean off the adrenal adaptogens.
- Follow up as needed.
Dr. Ruscio’s Comments
June’s case teaches us a lot. It illustrates the power of the gut as June was able to decrease her dose of thyroid hormone as her gut healed. The gut healing likely came from probiotics, digestive bitters, and by reducing the total load of H. Pylori.
It also teaches us that we do not need to treat lab results until they are “normal”. Sometime an “abnormal” finding is perfectly normal. H. Pylori and EBV illustrate this. Most notably the EBV early antigen improved markedly but still remained ‘abnormal/elevated’.
Had this case been handled wrong June would be walking around with “fear of autoimmunity.” She may have very likely been exposed to several rounds of unnecessary treatments trying to force the antibodies lower. Overtreatment of autoimmunity is one the most damaging practice mistakes I see in the field.
June is feeling terrific. Yes she has some “abnormal” lab findings but it’s our job as well-educated clinicians to teach our patients what this actually means. In June’s case it doesn’t mean anything. We reduced her H. Pylori load, viral load, reduced need for medication, and improved all of her symptoms. We now get to do the best thing any clinician can expect to do…. Tell our patients to follow up if or when it’s needed.
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Effects of low-carbohydrate diet therapy in overweight subjects with autoimmune thyroiditis: possible synergism with ChREBP.
https://www.ncbi.nlm.nih.gov/pubmed/27695291
Study purpose:
- To assess the impact of a diet devoid of carbohydrates (bread, pasta, fruit, and rice) and free from goitrogenic foods (including dairy) on thyroid function, thyroid autoimmunity and body composition
- said simply a low carb diet.
Intervention:
3 weeks on respective diet
- Treatment (low carb diet), n = 108
- Carbohydrates 12%–15%, proteins 50%–60%, and lipids 25%–30%.
- Dr. R’s note: this may equate to roughly 200 grams of carbs/day
- Instructed to eat large leafy and other types of vegetables and only lean parts of red and white meat, avoiding goitrogenic food.
- The following items were also excluded from the diet: eggs, legumes, dairy products, bread, pasta, fruits, and rice. “This protein-rich diet plan was implemented for 3 weeks”
- Carbohydrates 12%–15%, proteins 50%–60%, and lipids 25%–30%.
- Control, n = 72
- A simple, low-calorie diet without restrictions regarding the types of food to consume, but adhered to the recommended dietetic allowances, as suggested by the National Research Institute on Food and Nutrition
- Dr. R’s note: traditional dietary advice
- A simple, low-calorie diet without restrictions regarding the types of food to consume, but adhered to the recommended dietetic allowances, as suggested by the National Research Institute on Food and Nutrition
Main Results:
- Treatment
- Significant reduction of thyroglobulin (Tg) antibodies -40% and anti-peroxidase (TPO) antibodies -44%
- Control (untreated)
- Significant increase in thyroglobulin (Tg) antibodies +9%. The level of anti-peroxidase (TPO) antibodies increased without reaching statistical significance +16%.
Additional Results:
- No significant changes in thyroid hormones were reported between groups
- Low carb diet group experienced slightly better improvements in body composition
- 83% of patients with high levels of autoantibodies were breath test positive to lactase which may suggests carbohydrate malabsorption
Authors’ Conclusion:
- The dietary regime described in this study could be implemented for the treatment of patients with autoimmune thyroid because of the possibility to reduce the inflammation state in general and of the thyroid gland
Interesting Notes:
- “It is therefore evident that an improvement in the general conditions of the patients undergoing an ad hoc dietary regime leads to both a reduction of body weight and levels of autoantibodies”. Translation – ad hoc meaning not highly planned, so this diet was followed loosely.
Clinical Takeaways:
- A SIMPLE lower carb diet (around 200 grams/day) that removes diary and bread but focuses on meats and vegetables can both dampen thyroid autoimmunity and improve body composition.
Dr. Ruscio’s, DC, Comments
The reduction of carbs and allergens (gluten, diary) likely played the largest role, while the impact of avoiding goitrogens was likely minimal. This is because reduction of iodine has been shown to lower thyroid antibodies so one would think eating goitrogens (which impede iodine absorption) may actually help thyroid autoimmunity.
The carb reduction may also have been helpful because the majority of patients expressed a degree of carbohydrate malabsorption. We could speculate that a reduction of carbs (which these subjects poorly absorbed) reduced the amount of available substrate for the microbiota to feed on and may have corrected underlying overgrowths or imbalances thus improving the environment and immune status in the gut, thus improving systemic immune function.
How does this study support a cost effective and efficient FM model? Impressive results in thyroid autoimmunity were obtained without needing food allergy testing, and without needing a highly meticulous or restrictive diet.
Insufficient documentation for clinical efficacy of selenium supplementation in chronic autoimmune thyroiditis, based on a systematic review and meta-analysis.
https://www.ncbi.nlm.nih.gov/pubmed/27683225
Study purpose:
- To summarize the available data in order to determine if selenium therapy is effective for autoimmune thyroid.
Intervention:
- Trials of low quality or at risk of biased were not included, thus this review summarized data from 9 clinical trials for the systematic review and data from 5 clinical trials for the meta-analysis.
Main Results:
- The meta-analysis did not show selenium supplementation to be beneficial
- In other studies benefit has been shown for;
- Quality of life,
- In a meta-analysis from 2010, based on four trials, [9], the authors reported decrease in thyroid peroxidase autoantibody (TPO-Ab) levels and improvement in well-being and/or mood, after 3 months of selenium supplementation, as compared to placebo. https://www.ncbi.nlm.nih.gov/ pubmed/20883174
- Similar conclusions were reached in another meta-analysis from 2014, including nine trials [10]. https://www.ncbi.nlm.nih.gov/pubmed/25574167
- But not all data agree
- Finally, a Cochrane Collaboration systematic review from 2013, also including four studies, [11] reached no conclusion regarding effects on HRQL, and did not perform a meta-analysis of change in TPO-Ab https://www.ncbi.nlm.nih.gov/ pubmed/23744563
- Thyroid ultrasound
- Quality of life,
Additional Results:
- Two studies using selenium for 6-12 months showed no change in quality of life
- Two double-blinded trials used the SF-36 form [20, 42], and both reported no significant changes following six [42] or twelve [20] months of selenium supplementation in patients not treated with LT4.
- However, 2 other studies using selenium for 3 months + thyroid hormone replacement, showed increase in QOL when compared to thyroid hormone replacement alone
- Two studies used the SF-12 form and found significant improvement in well-being by 200 μg/d sodium selenite for three months, as compared to placebo [17, 36]. In both trials, selenium supplementation was administered adjuvant to LT4,
- This may mean selenium is helpful in the short term and/or that it is helpful when co-administered with thyroid hormone in those who require the hormone.
Authors’ Conclusion:
- “Our conclusion is that current evidence does not justify the emerging use of selenium supplementation in the treatment of AIT.”
Interesting Notes:
- “Chronic autoimmune (AIT) or Hashimoto’s thyroiditis affects 1–2% of the population with increasing prevalence with age and a female preponderance.”
- “In communities replete in iodine intake, it is the predominant cause of hypothyroidism.”
- “In a recent narrative review it was suggested that selenomethionine might be more effective than selenite in lowering thyroid autoantibody levels. However, no such trends were observed for any of the clinical outcomes assessed in our study”
Clinical Takeaways:
- Selenium may not be the thyroid panacea it has been suggested to be, however it may help with thyroid gland health and with quality of life. The effect of selenium appears limited to the short term, 3-6 months.
Dr. Ruscio’s, DC, Comments
A previous meta-analysis based upon 4 trials did show benefit, however these studies only looked at a 3 month window https://www.ncbi.nlm.nih.gov/pubmed/27702392. A key insight provided by this paper was looking at the level of impact of selenium in studies that were 3 months, compared to 6 months, compared to 12 months. Looking at this data it’s clear that the effect at 3 months is present however by 12 months no benefit is show and the placebo was actually shown to be more powerful.
So what does this mean? It means selenium may have its highest utility when used in the short term. This is good news because this means we should use a more conservative treatment duration with our patients. Also recall from a previous issue that you may not need to keep administering selenium until antibodies or “normal”. Achieving TPO less than 500 may be adequate
A Randomized Clinical Trial of Berberine Hydrochloride in Patients with Diarrhea-Predominant Irritable Bowel Syndrome.
http://www.ncbi.nlm.nih.gov/pubmed/26400188
Study purpose:
- To assess berberine’s utility in the treatment of diarrheal type IBS
Intervention:
- 132 patients randomized to receive 400mg of berberine hydrochloride daily, (delivered twice daily at 200mg) or placebo for 8 weeks – double blinded.
- Patients were followed for an additional 4 weeks post treatment
Main Results:
- A reduction of diarrhea frequency, abdominal pain frequency, and urgent need for defecation frequency were significantly more pronounced in the berberine group than the placebo group.
- A trend of improvement was observed with berberine hydrochloride for IBS symptom score, depression score, and anxiety score and IBS quality of life, compared with placebo.
Additional Results:
- After being off berberine for 4 weeks the treatment’s group’s symptoms approximated that of the control – meaning the effect of berberine was not long lasting.
Authors’ Conclusion:
- “berberine hydrochloride, conveniently delivered, is well tolerated and reduces diarrhea frequency, abdominal pain frequency, and overall IBS-D symptoms score as well as anxiety and depression scores; consequently, berberine improves the quality of life of IBS-D patients.”
Interesting Notes:
- Prevalence of IBS diagnosed by the Rome III criteria in the general population is 1.1–29.2%.
- The placebo response rate in randomized clinical trials conducted in Europe may vary from 0 to 91.7%, with a mean value of 43%.
- Studies have shown that berberine has antidepressant-like effect & has inhibitory action on monoamine oxidase enzyme
Clinical Takeaways:
- Berberine appears to be an effective treatment for diarrheal type IBS and may also benefit mood and quality of life. A lower dose, 400mg/day, may be effective. The effect however, may not be long term.
Dr. Ruscio’s, DC, Comments
Both the placebo group and the berberine group improved, remember, placebo can account for sizable improvements in IBS (43% on average). However, the treatment group experienced significantly better improvements than the placebo group. After being off berberine for 4 weeks the treatment’s group’s symptoms approximated that of the control – meaning the effect of berberine was not long lasting.
What does this mean? Perhaps a higher dose or longer duration of treatment would lead to longer lasting results? Perhaps if a healthy diet was implemented at the same time the results would have been more prolonged? It essentially tells us that management/treatment of IBS is likely not a mono-therapeutic endeavor.
The Intestinal Microbiota And The Role Of Probiotics In Irritable Bowel Syndrome: A Review
https://www.ncbi.nlm.nih.gov/pubmed/26840477
Study purpose:
- To review the available data so as to determine if probiotics are a viable treatment for IBS.
Intervention:
- This was an informal review, meaning it was not a systematic review or meta-analysis. Roughly 15-20 clinical studies were reviewed. And the paper cited 74 references total.
Main Results:
- Probiotics are helpful for global symptoms, pain, bloating and flatulence.
Additional Results:
- N/A
Authors’ Conclusion:
- “… probiotics, which are generally regarded as safe and may act on the global symptoms, bloating and flatulence, which have considerable appeal. Furthermore, a rather impressive scientific rationale has emerged for the use of probiotics in gastrointestinal conditions, including IBS.”
- “However, recommendations regarding individual species or strains continue to be limited by a lack of data and the poor quality of much of the available data.”
Interesting Notes:
- “A number of reviews as well as a recent well conducted systematic review and meta-analysis have demonstrated that probiotics have a therapeutic benefit in the IBS and may improve global symptoms, abdominal pain, bloating and flatulence.” https://www.ncbi.nlm.nih.gov/pubmed/25070051
- ‘IBS is a disorder is defined by the coexistence of abdominal discomfort or pain associated with an alteration in bowel habits.’
- “Irritable bowel syndrome is a common, chronic relapsing gastrointestinal disorder that affects 7%–22% of the population worldwide.”
- “The cardinal symptom in IBS is abdominal pain occurring in association with an alteration in bowel habit; diarrhea and/or constipation.”
- “It should be remembered that although dysbiosis has been recognized in various intestinal diseases, in most cases a definitive cause-and-effect relationship remains to be established.” Dr. R’s note: I think this point is most salient with regards to the changes we see in the microbiota (not including SIBO, SIFO, or infection) – we are unclear if the altered microbiota in IBS is a cause or a result of the disease.
- This paper lists the four main classes of probiotics as
- Lactic bacteria that include Lactobacillus, Lactococcus, Bifidobacterium and Streptococcus
- Saccharomyces (S. Boulardi)
- Escherichia
- Bacillus
- It is known that Lactobacillus and Bifidobacterium species have anti-inflammatory effects in the intestine and their depletion could contribute to lowgrade inflammation. Proinflammatory cytokine levels (e.g. interleukin (IL)-6, IL-8, tumor necrosis factor-α, and IL-1β) are elevated in the systemic circulation of patients with IBS.”
Clinical Takeaways:
- Probiotics are a viable treatment for IBS.
Dr. Ruscio’s, DC, Comments
The ‘best’ probiotic type or dose has yet to be defined so determine this empirically – perform a therapeutic trial with one of the major probiotic classes at a time and evaluate the response. Use what works. If nothing works, use nothing. Treat based upon symptoms, not labs, as we do not know if ‘microbiota lab changes’ are causal.
Remember that probiotics have been noted to improve GI barrier health, modulate the immune system (especially small intestinal immunity – GALT/MALT), reduce inflammation, have antibacterial actions and shown to be an efficacious treatment in SIBO. It is likely because of all these reasons that we see improvements in IBS with probiotics.
Does this mean EVERYONE will improve? No. The most common reaction I have seen is bloating. If someone bloats then either use less probiotics, another probiotic, or no probiotic at all.
Jason asks, “I understand that FODMAPs should be avoided in IBS, but what about resistant starch?”
Another good question. Let’s think about this from a 30,000 ft. perspective. To put it loosely, resistant starch is a type of prebiotic. If prebiotics have a negative impact on IBS (likely because they are feeding a microbiota that the immune system is already prone to attack), then does using a different form make sense? Not really. At least not theoretically. This being said, you could always have someone slowly and cautiously try resistant starch supplementation or to incorporate foods that are higher in resistant starch and see how they do. If there is any sign of regression, simply instruct the patient to stop. If you proceed slowly and start with a low dose you will mitigate any negative reactions.
But, why does Jason have this desire to try resistant starch? I think this is because there was massive hype surrounding resistant starch in certain circles on the internet. So there was hype, but if you look at the science behind the hype it was SUPER speculative; lots of animal model and petri dish studies…. Little to no human outcome study data (aka clinical trials). What do we see when we look at the clinical trials with resistant starch? Nothing impressive…. I review this here if you would like the details https://drruscio.com/dr-ruscios-book-preview-all-about-fiber/ . When we combine this with the fact that those with digestive conditions like IBS, IBD, and/or GERD/reflux have a significant amount of adverse reactions to prebiotics, we see a recommendation clearly emerge. Those with digestive conditions should be cautions with all prebiotics, including resistant starch.
One of the last podcasts that Robb Wolf and I recorded illustrated how this plays out in the real world. When resistant starch was first coming into vogue, Robb commented that he tried it and felt like it was really helping him. I didn’t say much as I didn’t want to burst his bubble, but I remember thinking ‘this isn’t going to end well’ – especially considering Robb has a history of Crohn’s (public information he has shared this on the podcast so I can disclose). Unsurprisingly, when we spoke again several months later Robb commented ‘doc I think resistant starch actually made me much worse’.
So what happened? Initial placebo effect which was then followed by an adverse reaction. Exactly what you would expect when you understand what the clinical data says and you avoid jumping on everyone else’s bandwagon (*remember the placebo effect accounts for 43% response on average and up to 91% at its highest*). These are things we as clinicians need to be immune to, because if patients can’t get competent advice from us, who can they get it from?
So in short, you can try it with anyone, but I would not recommend it with those with digestive conditions. Those without digestive conditions are most likely to experience a positive response. Prebiotics do have their clinical merit, which I will provide a detailed review on in my coming book, https://drruscio.com/gutbook/
Calprotectin has been shown a viable marker for tracking disease activity in IBD and can even predict a relapse. A smart phone based at home calprotectin screening has been developed, thus making monitoring much easier for patients: https://calpro.no/products/calprosmart-office-testkit
This technology has been found viable by a recent study, https://www.ncbi.nlm.nih.gov/pubmed/26535869 . It appears Genova is also offering this test.
Patient Info:
- Lori, 50yo female
- Previous dx
- SIBO, polycystic kidney and liver disease, unknown connective tissue disease, heavy metal toxic
- Rx: Xifaxan
- Chief complaints:
- Bloating
- Polycystic liver/kidney disease maintenance
- Acid reflux
- Unidentified connective tissue disease
- Allergies; congestion, post nasal drip
Visit 1 (1/29/16) – History and Exam
Lori presents as a happy 50yo female with a healthy diet and lifestyle balance, but is a very chronic case. She has had multiple surgeries for internal adhesions, scarring, and cysts.
She is now presenting after working with many conventional medical providers and was encouraged to seek additional council with our clinic from Dr. Mark Pimentel. She is a bit of a blank slate because her internal anatomy was just recently altered (hopefully for the better) via a recent abdominal surgery to reduce connective tissue impairment of her GI. This may change how well she responds to treatment (including those she has had not responded to in the past). She has also had her gallbladder removed and has liver disease.
She has previously responded well to high dose HCl and bile. Also to the elemental diet as Vivonex Plus. Xifaxin’s effect and that of probiotics was unclear. Low dose erythromycin has not helped. She has also previously responded well to metal detox. SIBO has not retested positive in the past, making me think there is more than SIBO present.
I am unclear how much I can help due to altered anatomy and connective tissue disorder.
Initial impression
- Lori is an unusual case. The fact that she has no gallbladder and liver disease suggests she may do especially well with supplemental bile. Of course, abdominal adhesions are highly suspected, both due to her connective tissue disease and due to her recent surgery.
- Even though she has tested negative recently for SIBO, there may be another form of dysbiosis present; SIFO or H2S SIBO or fungus….
- She presented with many oral caries, so I recommended some general oral health practices. She is on far too many supplements, but had done a good job with determining what foods seemed to work for her.
Visit 2 (2/15/16) – Testing and Initial Recommendations
Testing
- AeroDiagnostics SIBO breath
- Medical Futures urinary H2S test
- BioHealth 401H stool test
- Genova Organix Dysbiosis urine test
- DiagnosTechs GI-15 stool/saliva test
- LabCorp
- Comprehensive blood panel
- Full GI panel
- *too many markers to list here
Recommendations
- Diet: continue with the diet you have found helpful.
- Lifestyle: work to find the minimal amount of self-prescribed supplements needed.
- Oral Health: oil pulling, mouth wash, probiotic toothpaste.
- GI: High dose HCl, bile, Iberogast. Lacto/Bifido probiotics, S. boulardii probiotic, digestive enzyme formula.
- Perform a consultation with ClearPassage to see if you are a candidate for their therapy to break down abdominal/pelvic adhesions.
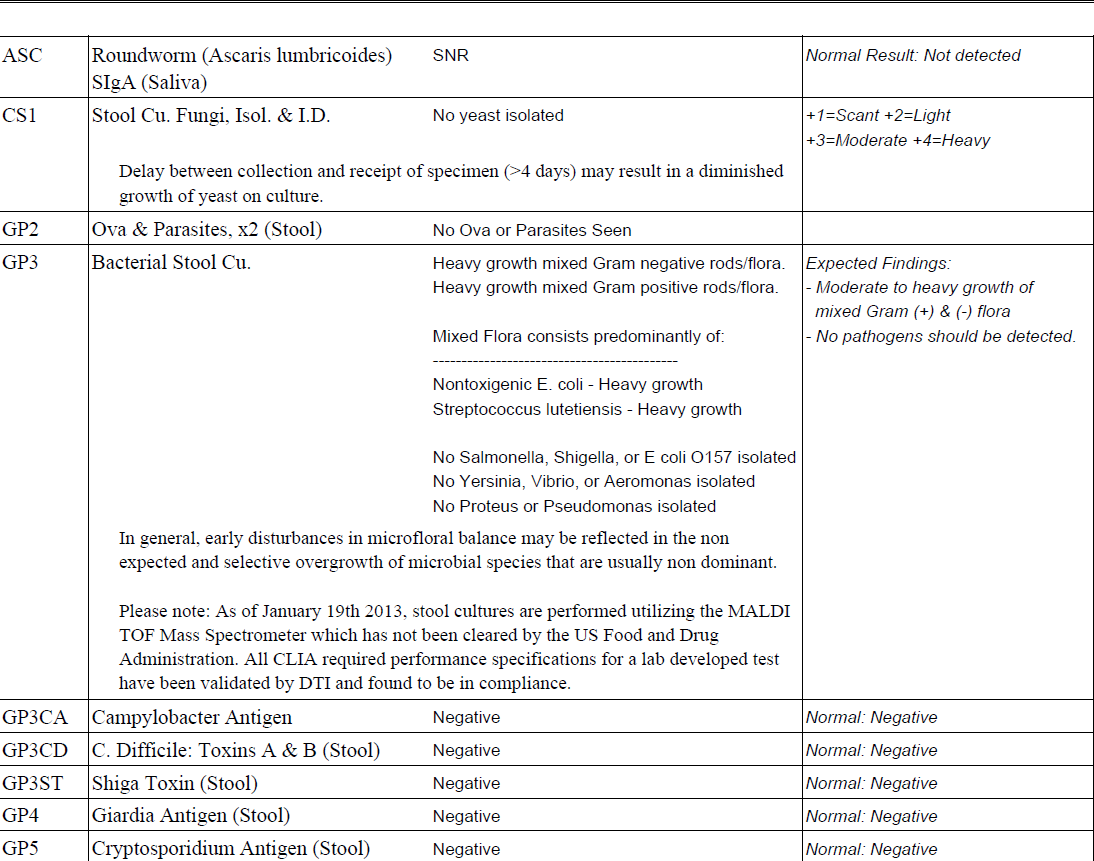
Visit 3 (5/6/16) – Lab Interpretation and Treatment Evaluation
Lab interpretation:
- Summary
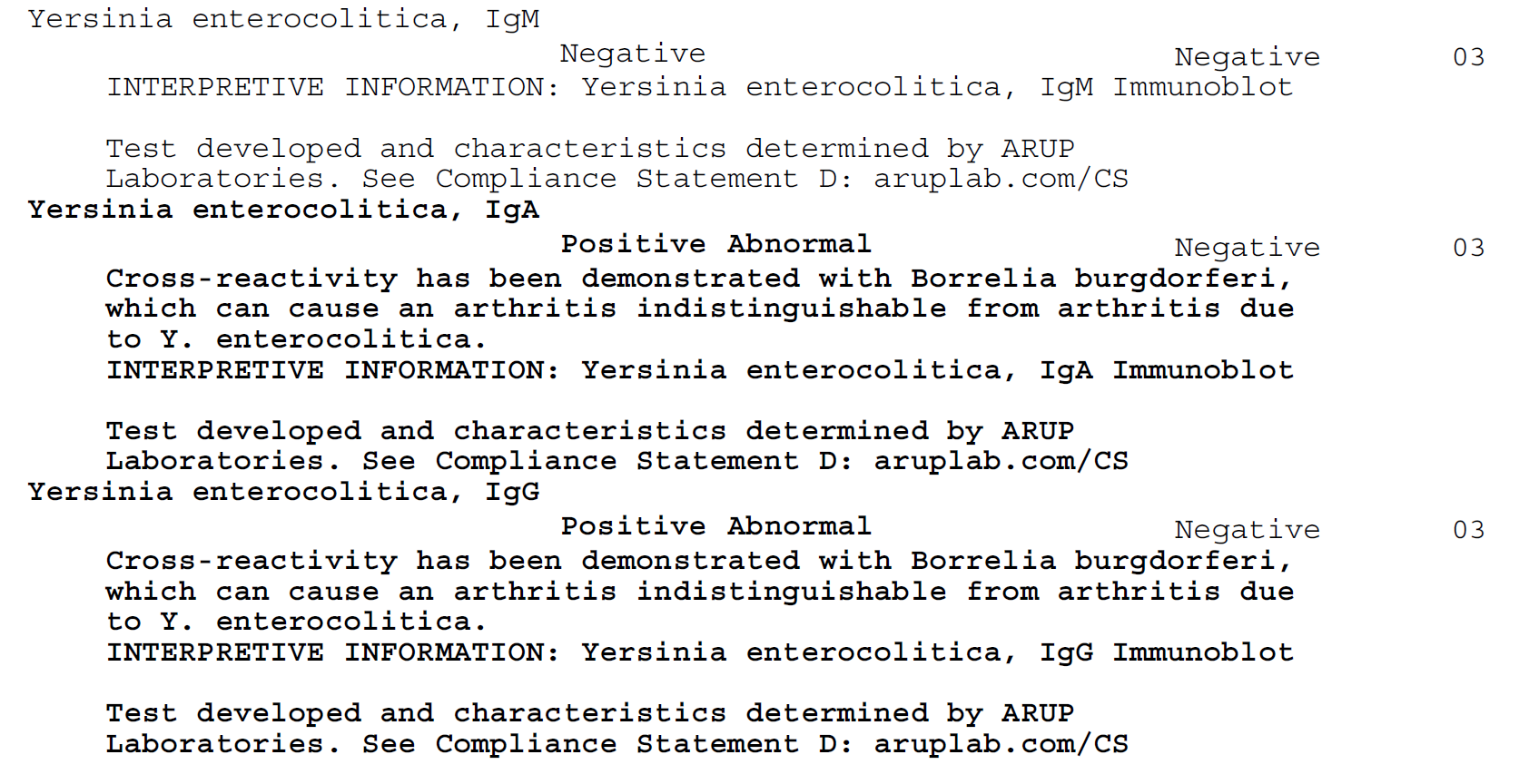
- Yersinia, light candida, borderline H2 SIBO, and bacterial dysbiosis. High HbA1c, ferritin, and potential anemia. Low WBCs. Potential IBD.
- AeroDiagnostics Glucose SIBO breath
- Normal
- Medical Futures urinary H2S test
- Inconclusive
- BioHealth 401H stool test
- Light candida
- Genova Organix Dysbiosis urine test
- Bacterial – Phenylacetate, p-Hydroxybenzoate,
- DiagnosTechs GI-15 stool/saliva test
- Normal
- LabCorp
- Comprehensive blood panel
- Hemoglobin A1c 5.9-H, Ferritin 267-H, Cholesterol 233-H, LDL 132-H
- WBC 2.5-L, MCV 103-H
- Full GI panel
- Yersinia IgA, IgG
- AMCA antibodies
-
- Comprehensive blood panel
Subjective Assessment
- ‘Feeling about the same as last visit.’
- Had a negative bloating reaction to Iberogast.
Impression:
- Lori’s case is an unusual one due to previous surgery and other dx, but we have found some minor GI findings today that when treated may yield improvement. The ferritin may be caused by inflammation, so monitor before considering low iron diet.
- So far no change symptomatically, but hoping today’s plan will yield improvement, but I also anticipate reactions along the way.
- Lori was found to be an excellent candidate for ClearPassage therapy.
Recommendations
- Continue previous
- Diet: continue with the diet you have found helpful.
- Oral Health: oil pulling, mouth wash, probiotic toothpaste.
- GI: High dose HCl, bile. Lacto/Bifido probiotics, S. boulardii probiotic, digestive enzyme formula.
- See your primary care doctor regarding your low white blood cells.
- GI:
- Herbal antimicrobial protocol for SIBO
- Semi-elemental diet; use daily to replace up to 50% of your daily meals
- Discontinue Iberogast
- Move forward with ClearPassage therapy
- Follow up in 4 weeks
Visit 4 (7/1/16)
Subjective Assessment:
- Overall, feeling 20-25% better compared to last visit.
- Feels like probiotics are working well.
- Starting care at Clear Passage on July 6th.
- Herbal antimicrobials are helpful.
- Semi-elemental diet caused flare. Homemade elemental diet caused flare.
- Bloating improved by 50% other than flares noted above.
Impression:
- Probiotics and antimicrobials are working. Elemental/semi-elemental diets are not tolerated. Hopeful ClearPassage therapy will yield significant improvements.
Recommendations:
- Continue previous
- Diet: continue with the diet you have found helpful.
- Oral Health: oil pulling, mouth wash, probiotic toothpaste.
- GI:
- High dose HCl, bile. Lacto/Bifido probiotics, S. boulardii probiotic, digestive enzyme formula.
- Herbal antimicrobial protocol for SIBO.
- ClearPassage therapy.
- Discontinue semi-elemental and elemental diet use.
- Follow up in 4 weeks.
Visit 5 (7/29/16)
Subjective Assessment:
- Just finished first 20hr session with ClearPassage. Feels another 20% better from this. CP therapist feels she is responding very well.
- Less bloating and cramping. Still does have some pain and bloating, but much improved.
Impression:
- We are on the right track, the combination of probiotics, HCl, bile, antimcirobials, and abdominal adhesion therapy has provided the greatest overall level of improvement Lori has obtained in several years.
- We will have Lori finish her current round of antimicrobials and then follow up 4 weeks later. We will not use a prokinetic due to previous negative response.
Recommendations:
- Continue previous
- Diet: continue with the diet you have found helpful.
- Oral Health: oil pulling, mouth wash, probiotic toothpaste.
- GI:
- High dose HCl, bile. Lacto/Bifido probiotics, S. boulardii probiotic, digestive enzyme formula.
- Herbal antimicrobial protocol for SIBO.
- ClearPassage therapy.
- Follow up in 4 weeks after you’ve finished your antimicrobials.
Visit 6 (9/9/16)
Subjective Assessment:
- Is maintaining her previous improvements.
- Seems to be making gradual improvements from month to month.
Impression:
- We are on the right track, the combination of probiotics, HCl, bile, antimcirobials, and abdominal adhesion therapy has provided the greatest level of improvement Lori has obtained in several years.
Recommendations:
- Continue previous
- Diet: continue with the diet you have found helpful.
- Oral Health: oil pulling, mouth wash, probiotic toothpaste.
- GI: High dose HCl, bile. Lacto/Bifido probiotics, S. boulardii probiotic, digestive enzyme formula.
- ClearPassage therapy.
- Follow up in 2 months.
- Retest previous bloodwork.
Dr. Ruscio’s, DC, Comments
At her next visit, Lori was continuing to improve slowly and steadily. I did not feel the need to retest any of her previous GI findings for 2 reasons. Firstly, her findings were not highly significant (in my opinion). Secondly, our current program had provided the best results she has obtained in a very long time. We did retest the blood panel and decided it was best to have this monitored by her hematologist and nephrologist, neither of which expressed any concerns over the continued but varied abnormalities found on her differential and CMP.
Lori’s case provides a clear example of when abdominal adhesions therapy can have high utility. This combined with providing some basic digestive support (probiotics, enzymes, HCl), a higher dose bile supplement (due to her liver/gallbladder issues), and antimicrobials was a winning combination.
It also provides a good example of how/when collaboration with other providers is a good idea. It might be tempting to try and ‘manage’ her polycystic liver/kidney disease, but this is not an area of my specialty and therefore it would be irresponsible to attempt to do so. This prevented me from attempting to micromanage the abnormalities found on her blood work. This led to less testing/treatment. Any attempts to micromanage her bloodwork would have been in vain as her respective specialist did not find the abnormalities to be a concern given Lori’s pre-existing conditions.
Lori is now on a reasonable treatment program and making slow and steady progress. She has been more than thrilled with her results. We will work to curtail/minimize her treatment program gradually in the future.
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Effective vitamin B12 treatment can reduce serum antigastric parietal cell antibody titer in patients with oral mucosal disease.
https://www.ncbi.nlm.nih.gov/pubmed/27474730
Study Purpose:
- To assess the impact of B12 administration on stomach autoimmunity (anti-parietal cell antibodies). This was a follow up to a previous study by this same group, http://www.ncbi.nlm.nih.gov/pubmed/20659263 . These cells are responsible for producing stomach acid and for absorption of B12, so the clinical implications are significant.
Intervention:
- 210 patients were given either
- One B12 injections per week as 1,000 mcg hydroxocobalamin.
- Oral B12/vitamin blend. 1 capsule twice per day. Each capsule contained:
- 10 mg of vitamin B1, 5 mg of vitamin B2, 5 mg of vitamin B6, 5 mcg of vitamin B12, 20 mg of calcium pantothenate, 50 mg of nicotinamide, 150 mg of vitamin C, and 60 mg of calcium.
- Note: this equals 70 mcg per week of oral B12
Main Results:
- B12 injection group
- “We found a significant drop of the positive antibody rate from 100% to 42.9%”
- Oral B12 group
- Antibody “titers increased to significantly higher levels”
Additional Results:
- Maintenance vitamin B12 injections once a month could retain remission of antibodies in 87% of patients compared with 10% in those without vitamin B12 injections.
Authors’ Conclusion:
- Vitamin B12 injections can reduce higher serum anti-parietal cell antibody titers to significantly lower or undetectable levels.
Interesting Notes:
- Roughly 30% of patients with parietal cell antibodies also have thyroid antibodies.
- The following symptoms were reported by patients with parietal cell autoimmunity:
- Burning sensation in the mouth 98%
- Dry mouth 80%
- Sore tongue 60%
- These are good symptoms to add to your paperwork as a prompt for testing these antibodies.
- B12 did not affect thyroid autoimmunity in those with pre-existing thyroid autoimmunity.
- “We also found that patients with higher titers needed longer periods of vitamin B12 injection treatment to achieve complete response.”
Clinical Takeaways:
- Vitamin B12 injections can arrest stomach autoimmunity. Those with oral burning, dry mouth, and/or sore tongue are at increased risk for stomach autoimmunity.
Dr. Ruscio’s, DC, Comments:
This study is very exciting. It reinforces previous findings from this group that B12 injections can arrest stomach autoimmunity. This study also showed that oral B12 did not have this effect. After weekly injections until the antibodies are normal, the results can be maintained by once monthly injections. This therapy could potentially preserve the health of stomach tissue and therefore prevent loss of the ability to produce hydrochloric acid and intrinsic factor.
How to Test and Treat Small Intestinal Bacterial Overgrowth: an Evidence-Based Approach.
https://www.ncbi.nlm.nih.gov/pubmed/26780631
Study Purpose:
- To review the available evidence regarding SIBO treatment and to offer an evidence based treatment approach.
Intervention:
- N/A
Main Results:
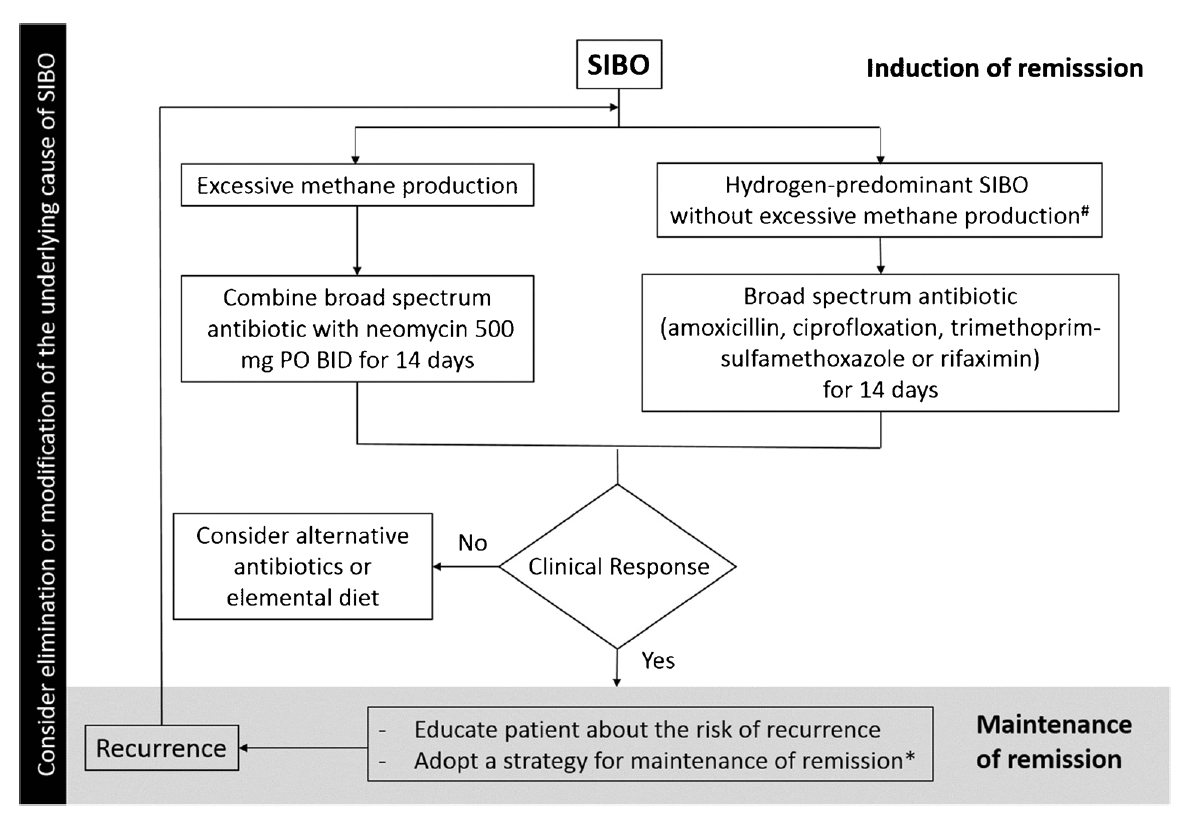
- Here is their proposed management strategy:
-
Additional Results:
- See below
Authors Conclusion:
- See below
Interesting Notes:
- “Multiple independent risk factors have been identified for SIBO including [4]: (1) anatomical abnormalities such as small intestinal diverticulosis; (2) postsurgical structural changes such as ileocecal valve resection, gastric bypass, and Roux-en-Y; (3) medications that slow the gut motility such as narcotics, anticholinergics, and anti-diarrheals; (4) hypo- or achlorhydria due to surgery, autoimmune gastritis, or proton pump inhibitors [5••, 6]; and (5) small bowel dysmotility irrespective of the cause (e.g., inflammatory bowel disease, celiac disease, radiation enteritis, small bowel adhesions, and systemic diseases associated with dysmotility such as scleroderma, diabetes, and amyloidosis) [5••, 7].”
- Note: we just discussed B12’s effect on autoimmune gastritis.
- “SIBO has been associated with multiple conditions including irritable bowel syndrome [8], rosacea [9], hepatic encephalopathy [11, 12], obesity [13], gastroparesis [14], Parkinson’s disease [15], fibromyalgia [16], chronic pancreatitis [17], end-stage renal disease [18], and inflammatory bowel diseases [19].”
- Note: this shows the following connect to the gut: skin, liver, metabolism, brain, and pancreas.
- Gastrointestinal symptoms may not always predict SIBO.
- “Human cells are not capable of producing methane or hydrogen gas [23]. The presence of these gases in the human breath signifies the metabolism of carbohydrate residues by gut, their absorption from the gut, and expiration through lungs.”
- “those with excessive methane production are five times more likely to have constipation [26]. Moreover, the severity of constipation directly correlates with the methane level [27].”
- “Although not fully validated, currently, the accepted gold standard for diagnosis of SIBO is the aspiration of small bowel fluid, followed by culture and bacterial count. Proximal small bowel culture may be falsely negative as it can miss overgrowth of bacteria in the mid and distal small bowel.”
- “In a meta-analysis of 10 placebo-controlled trials, antibiotics were shown to be superior to placebo with a combined normalization rate of 51 % for antibiotics compared with 10 % for placebo.”
- Two studies have shown neomycin along with Rifaximin to be more effective for methane SIBO than Rifaximin alone:
- “Based on this, we advocate 2 weeks of therapy with neomycin and rifaximin for treatment of patients with methane-predominant bacterial overgrowth.”
- Note: the term predominant, meaning neomycin may not be needed just because methane is above 3ppm. It may only be needed when methane is the predominant
- “Elemental diets may be an extremely safe and effective alternative to antibiotics.” One study found an 80-85% response rate to elemental diets.
- Herbal antibiotics showed a 46% normalization rate of SIBO breath testing according to one study.
- “Lauritano et al. [45] showed that 13, 28, and 44% of SIBO patients experience a relapse of their symptoms and breath test positivity at 3, 6, and 9 months.”
- There are 2 classes of prokinetics, which are considerations in preventing relapse of SIBO:
- “motilin receptor agonists (e.g., erythromycin and azithromycin) and
- 5-HT4 agonists (e.g., tegaserod, cisapride, and prucalopride).”
- Note: The one study looking at this found that tegaserod extended time in SIBO remission. However, erythromycin did not show a statistically significant benefit. This is important to bear in mind and suggests potentially we are overstating the effect of erythromycin. Which is why this study concluded, “Tegaserod significantly prevents the recurrence of IBS symptoms after antibiotic treatment compared to erythromycin or no prevention.”
- “In a systematic review, Rao et al. [55] found that a low FODMAP diet improved overall IBS symptoms in 6/6 trials”
Clinical Takeaways:
- Antibiotics, herbals, elemental diet, and low FODMAP diets are all efficacious treatments for SIBO and/or IBS.
- SIBO has been associated with many non-gut conditions/symptoms.
- Neomycin may not be needed just because someone has methane positivity, but may be best reserved for when methane is
- The SIBO relapse preventative effects of erythromycin may be overstated.
Dr. Ruscio’s, DC, Comments
Most of my comments on this study were provided in the clinical takeaways. However, one thing that was disappointing was the short and incomplete mention of probiotics. A handful of clinical trials have shown that probiotics can reduce SIBO gas levels. Several clinical trials have shown probiotics to benefit IBS. I fear there may be a bit of an anti-probiotic biased present here. Other than that, this was a great review of available SIBO treatment/prevention options.
Helicobacter pylori CagA antibodies and thyroid function in latent autoimmune diabetes in adults.
https://www.ncbi.nlm.nih.gov/pubmed/27775795
Study Purpose:
- “determine the association between H. pylori infection and its virulent strain CagA with antibodies against thyroperoxidase (TPO Ab) and thyrotropin (TSH) in a cohort of latent autoimmune diabetes in adult (LADA) patients.”
Intervention:
- “We included 234 LADA patients (53.8% women). Antibodies against H. pylori whole antigens and CagA, TPO Ab and TSH were assessed in all patients.”
Main Results:
- Prevalence of IgG against H. pylori and CagA was 52.1% and 20.9% respectively.
- Antibodies against H. pylori were not associated with TPO Ab and TSH.
- Antibodies against CagA showed a positive association with TSH and TPO Ab.
- Subjects with hypothyroidism (TSH ≥ 3.5 μU/ml) had an increased frequency of Ab anti CagA .
-
Additional Results:
- Other studies showing an association between HP and thyroid autoimmunity
- Studies showing treatment of HP can reduce thyroid AI
- **Meta-analysis showing association between H. Pylori and thyroid autoimmunity
Authors’ Conclusion:
- “We showed that titers of TPO Ab and CagA were related, suggesting that the presence of most virulent pylori could be a risk factor for the presence of thyroid autoimmunity and a functional impairment of the thyroid gland.”
Interesting Notes:
- “Latent autoimmune diabetes in adults (LADA) is a type of autoimmune diabetes characterized by the presence of antibodies against glutamic acid decarboxylase 65 (GAD65 Ab) with a clinical picture very similar to type 2 diabetes at diagnosis.”
Clinical Takeaways:
- CagA H. Pylori and HP in general are associated with thyroid autoimmunity. Treatment of HP may improve thyroid autoimmunity.
Dr. Ruscio’s, DC, Comments
This study provides some nice documentation for the gut-autoimmunity connection as it relates to HP. It appears that HP in general may be associated with thyroid autoimmunity and that CagA HP might be more strongly associated.
Does this mean all autoimmune thyroid patients should be screened for HP? Well, maybe. The data here are not complete in the sense that we don’t know that treating this finding will yield any clinical benefit. If one could perform a screening at a reasonable cost, I think this is much more justifiable. Most of the studies looked at HP stool antigen for serum antibodies.
Regarding treatment of HP: I don’t think we have strong enough data to suggest triple or quadruple therapy for HP is justified in non-symptomatic (digestively) autoimmune thyroid patients. However, natural treatment options may be a justifiable alternative for this group. Anti-microbial herbs, paired with probiotics and potentially NAC, carry extremely low adverse effects and even have secondary health benefits.
To state this simply: if someone has HP and the classic GI symptoms that it causes (ulcer, indigestion, reflux) – treat via any of the available options. If someone has no GI symptoms but has thyroid AI, consider a natural treatment option.
Solar radiation and the incidence and mortality of leading invasive cancers in the United States.
https://www.ncbi.nlm.nih.gov/pubmed/27195056
Study purpose
- To assess the relationship between level of ultraviolet light exposure and invasive cancers
Intervention:
- The North America Land Data Assimilation System (NLDAS) daily average sunlight for the continental United States from 1999–2011 was analyzed in relation to the US Cancer Statistics age-adjusted-incidence and mortality from the Centers for Disease Control and Prevention (CDC).
Main Results:
- Cancer incidence
- “We found associations between increasing solar energy and decreasing cancer incidence for: all invasive cancers, brain/nervous system cancer, breast cancer, colon/rectum cancer, corpus uteri cancer, esophageal cancer, larynx cancers, leukemias, non-Hodgkins lymphoma, ovarian cancer, prostate cancer, and urinary bladder cancer.”
- “We found associations between increasing solar energy and increasing cancer incidence for: cervix uteri cancer and liver cancer.”
- We found no associations between solar energy and melanoma.
- Cancer mortality
- “We found no association between increasing solar energy and decreasing cancer mortality for all invasive cancers.”
- “We found that increasing solar energy increased liver cancer mortality.”
- We found no associations between solar energy and melanoma.
Additional Results:
- N/A
Authors’ Conclusion:
- “In summary, the current study confirms other ecological studies relating solar radiation to the incidence and mortality of a variety of cancer types.”
Interesting Notes:
- The method used to assess solar radiation in this study is likely more accurate than latitude because it accounts for factors such as cloud cover, ozone levels, and altitude.
Clinical Takeaways:
- Reasonable sun exposure may promote health.
Dr. Ruscio’s, DC, Comments
This study essentially found that living in a location with increased UV exposure was correlated with a decreased incidence of most, but not all, invasive cancers. What is more interesting is that the invasive form of skin cancer, melanoma, did not increase in incidence nor mortality with increased UV exposure. This study supports a growing body of evidence that suggests reasonable sun exposure may improves one’s health and that strict sun avoidance may have unintended health consequences.
Greg Williams asks:
“I’m interested to know your views on multivitamins. Do you consider them to be worthwhile, almost as an insurance policy against nutrient deficiencies? And if you do, are there any particular brands you recommend? In particular, I’m interested in their use for people with digestive issues (I mainly work with Crohn’s and Ulcerative Colitis sufferers). Thanks.”
Good question, Greg. Patients with IBD do have an increased incidence of deficiencies, for example, anemias of iron and/or B12, so this question has much clinical relevance. I do use multivitamins. I will usually use a multivitamin if someone presents with general signs of malabsorption. The most notable signs are unintended weight loss, being underweight, and/or frank anemia. Of course, if a patient’s CBC/differential shows deficiency, we will offer whatever nutritional support is indicated, often in conjunction with a multivitamin just to cover our bases.
There are a few other thoughts that are important here also. A multivitamin will not address the cause of the malabsorption, so it’s essential to obtain a good outcome with whatever underlying GI condition is present: IBD, IBS, GERD, gastritis, ulcers…. If patients are highly reactive, then I usually will forgo a multi to reduce the potential of a reaction.
I usually only use a multi for a few months and then discontinue. Part of the reason for this is because some studies have shown harm from long-term vitamin supplementation. So to hedge against this, I prefer a shorter term usage to obtain benefit while mitigating any risk associated with long-term use.
Any reputable brand should be fine.
I ask my staff the following questions at least once per month:
“What are we doing that feels hard, broken, or inefficient?” or
“What is the least favorite part of your job?”
Every office has its strengths and its weakness. Oftentimes it’s the weakness that you can’t see that are the most problematic. For example, a weakness that never bothers you because you are not the one doing the work. But this weakness might be a huge headache for a staff member, causing them to perform inaccurate or inefficient work, either of which will cut into your clinics profitability, customer service, and moral.
When you ask, and make it OK to answer, your staff what is wrong, broken, or inefficient, you have the chance to see what is not working. In asking this question repeatedly for the past few years, the level of efficiency, customer/patient service, and office moral has increased dramatically.
For example, one time after asking this question it came to my attention that filling out the lab requisition form was tedious for one of the labs we used. I asked, “Why?” The staff commented that every time we order this test, the lab would send us a form with the patient information they had, then our office had to print this form out, fill in the missing information, scan it, and then email it back! So the answer was simple. We asked this lab if they could start sending us this form digitally, and they said yes. So now we receive the form, then fill it all in digitally, and send it right back. It has saved us 15 minutes per order. If you are doing 10+ of these labs a day, you just saved over 1.5 hours of staff time per day.
These little things add up. Your staff is done earlier, is happier because they weren’t spinning their wheels, and you saved money on payroll. It’s a win-win.
“Feedback is the breakfast of champions.”