Patient Summary:
- Overview Context:
- Patient is a 38 year old nurse practitioner and mother of 3 with primary symptoms of chronic diarrhea. Onset began around the time she had possible acute gastroenteritis two years ago. “I eat so clean. At this point I feel like it’s not food and there’s something else going on. I hate to go back on steroids, but I need a break.”
Initial Impression: 50/100
Symptoms and Concerns
- Chief Complaints:
- Diarrhea (Up to 16x/day)
- Fatigue
- Brain fog
- Bloating
- Dry eye/Episcleritis (burning pain, swelling, photosensitivity of eyes)
- Muscle aches
- Onset/Timeline
- 2019: Moved into renovated home; using well water with added filter and water softener. Water not tested for heavy metals.
- 2020: Reports GI infection at this time. Shortly after, she began experiencing diarrhea and bloating. Symptoms waxed and waned for the next 2 years.
- 2021: Officially diagnosed with microscopic colitis. Steroid treatment improved symptoms.
- 2022: GI infection, which led to a severe regression in symptoms. New onset of symptoms including fatigue, brain fog, and episcleritis.
Past Medical History
- Prior Diagnosis:
- Microscopic colitis (2021)
- Medications:
- NA
- Pertinent Labs:
- Stool test (2021)
- Negative for pathogens
- Normal calprotectin
- Stool test (2021)
Prior Testing and Treatment History
- Previous Treatments (major pertinent helpful or negative treatment):
- Helpful
- Gluten free
- Dairy free
- Budesonide (steroid medication for microscopic colitis)
- Non Responsive
- Paleo
- Low FODMAP (haphazard)
- Probiotics
- Herbal antimicrobials
- Digestive repair nutrients
- Helpful
Initial Impression
- Clinical Commentary:
- She has tried many different therapies, but they have been somewhat haphazard. We find it very helpful to get a better understanding when someone says “I tried treatment XYZ”. We want to find out if they gave a therapy a clinically useful trial. If not, it’s worth revisiting.
- My top differential is dysbiosis given the fact her symptoms began after an acute gastrointestinal infection.
- Initial Treatment Recommendations
- Diet:
- Paleo low FODMAP diet
- Intermittent fasting 14-18 hours, 1-2x/week
- Supplements:
- 2-4 day elemental diet reset to hybrid application (replacing 1-2 meals/day on most days if reset is helpful)
- Lacto/bifido probiotic blend. Soil-based probiotics. Saccharomyces boulardii probiotic.
- GI supportive nutrients
- Followup:
- 6 weeks
- Diet:
- Labs:
- Fecal calprotectin
- Clinical Commentary:
- Despite her trying a low FODMAP diet in the past, it wasn’t implemented effectively, so it is worth another trial. A 2-4 day reset on an elemental diet can be helpful for quickly getting someone out of a flare.
- We always want to make sure our testing will affect our treatment plan. If her calprotectin is elevated, we’ll want to be more aggressive with anti-inflammatory treatments and ensure she follows up with a gastroenterologist for a more thorough assessment.
- Subjective Assessment
- 80/100, 75% better.
- “Diarrhea is the most normal it’s been in over 2 years.” No episcleritis episodes.
- Current Symptoms:
- Improved:
- Diarrhea
- Bloating
- Fatigue
- Brain fog
- Dry eyes/episcleritis
- Muscle aches
- Same:
- NA
- Worse:
- NA
- Improved:
- Response to Treatment
- Diet:
- Paleo low FODMAP diet: Very helpful
- Supplements:
- Elemental diet 2-4 day reset: Huge improvement in energy
- GI support nutrients: Helpful
- Probiotics: Initial improvement, but worsened bloating. Stopped all 3 and bloating improved, but unsure which one caused it.
- Diet:
- Updated Treatment Recommendations
- New Treatment:
- Herbal antimicrobial protocol
- Add in 1 probiotic at a time. Stay on what you tolerate well.
- Expand Paleo low FODMAP diet
- Followup: 10 weeks
- New Treatment:
- Clinical Commentary:
- Given her great response to initial GI treatments, we want to pivot to adding in herbal antimicrobials to further move her in the right direction. Calprotectin was not performed by the patient.
- Subjective Assessment
- 60/100, 30% better/worse.
- “I was doing very well until I had another flare that started about 2 weeks ago. Since then, it has definitely gotten worse.”
- Current Symptoms:
- Improved:
- Dry eyes/episcleritis
- Brain fog
- Same:
- NA
- Worse:
- Diarrhea, 6-10 watery BM’s daily since flare
- Bloating/cramping, since flare
- Fatigue, since flare
- Improved:
- Response to Treatment
- Diet:
- Expand low FODMAP diet: Was tolerating foods well.
- Supplements:
- Herbal Antimicrobials: “Felt amazing on HABx for the first 3 weeks, but flared at week 4.”
- Diet:
- Updated Treatment Recommendations
- Note to patient:
- “I am sorry you’re in a flare! Let’s work on getting you back to feeling better. Please stop the herbal antimicrobials. We will also get you back on the elemental diet 2-4 day reset to quickly help get out of this flare. If you are still not doing well after about 2 weeks of this plan, you can start immunoglobulin therapy.”
- New Treatment:
- Stop herbal antimicrobials
- Start elemental diet 2-4 day reset
- Resume Paleo low FODMAP diet
- Start immunoglobulin therapy if flare doesn’t improve with the above therapies
- Followup: 4-6 weeks
- Note to patient:
- Clinical Commentary:
- This patient felt fantastic during the first few weeks of herbal antimicrobial therapy, but she flared around week 4. This indicates we were effectively addressing her dysbiosis, but 4 weeks was too long a period of therapy for her. This is why it’s very important to listen to the patient. Instead of continuing the herbs, we stopped them and revisited therapies that were initially helpful (e.g. elemental dieting and Paleo low FODMAP diet).
- We also gave her a backup plan of immunoglobulins to help get her out of the flare if the main recommendations didn’t accomplish this.
Closing Thoughts
- This case highlights the power of treating empirically instead of based on GI testing. Working through the treatment hierarchy led to a 75% improvement just after her first visit.
- This case also illustrates what to do if a patient initially feels great, but then regresses. Sometimes the best thing to do is revisit the therapies that were successful instead of moving immediately to novel therapies.
- The use of a low FODMAP diet, elemental dieting, GI support nutrients, probiotics, and herbal antimicrobials is a clinically impactful combination of therapies for improving microscopic colitis (as well as IBD, IBS, and SIBO).
PMID: 34532928
Study purpose
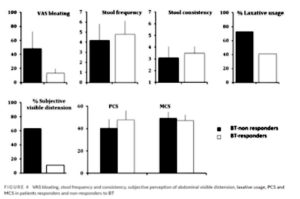
- This study aimed to answer two questions: 1) In patients with bloating, what is the prevalence of defecation disorders? 2) What effect does pelvic floor biofeedback therapy have on bloating that is non-responsive to dietary modifications?
- “We hypothesized that bloating and abdominal distension could be secondary to impaired gas or non-gas rectal emptying possibly due to disordered defecation.”
Intervention:
- 156 patients with severe bloating, all treated with the standard IBS diet x 2 weeks
- Patients who did not respond to dietary intervention were assessed for disordered defecations with electromyography (EMG) and balloon expulsion test
- Those with disordered defecation were treated with pelvic floor biofeedback
- Biofeedback intervention:
- First taught to strain more effectively and to coordinate expulsion efforts with their breathing
- Then taught to relax pelvic floor muscles during straining through EMG imaging
- Biofeedback intervention:
Main Results:
- Of the 156 patients with severe bloating treated with diet, 33% saw improvements in their bloating
- Of the patients who did NOT improve with diet, 64% of them failed the balloon expulsion test, indicative of disordered defecation
- “Patients who had higher bloating had a significant association with failed balloon expulsion test.”
- This indicates that those with more severe bloating were more likely to have disordered defecation
- After biofeedback, 54% of patients saw fair to major improvements in bloating, and they all saw at least a 50% reduction in bloating severity
- Biofeedback also led to improvements in:
- Abdominal distension
- Laxative usage
- Stool frequency and consistency
Authors Conclusion:
- “Our study shows that in patients with severe bloating, who did not respond to diet advice, bloating had a strong association with defecation disorders. The correction of disordered defecation was associated with significant relief of bloating.”
Clinician’s Comments
- This study found a significant proportion of patients with bloating who don’t respond to dietary interventions respond well to pelvic floor biofeedback therapy. We at the clinic have been incorporating a pelvic floor physical therapy referral as part of our treatment hierarchy, but it is typically more end-phase.
- We first focus on more conservative therapies such as diet, probiotics, antimicrobials, digestive enzyme support, immunoglobulins, exercise, and stress management.
- We use the patient’s history as well as response to treatment to determine if and when a pelvic floor therapy referral is indicated.
PMID: 34241973
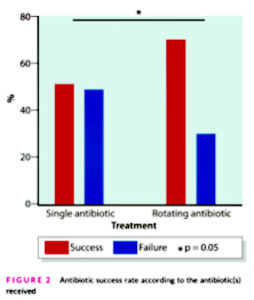
Study purpose
- This study aimed to assess the effectiveness of treating SIBO with single antibiotics or rotating antibiotics.
Intervention:
- Retrospective study, 223 patients with SIBO based on a glucose breath test using the Rome consensus criteria
- Patients were treated with the following for 10 consecutive days per month for 3 months:
- Single antibiotic (quinolone or azole) (N = 193)
- Rotating antibiotics (Azole and quinolone, one after the other) (N = 30)
- Note: This study took place in France over the course of 15 years. Rifaximin was not available in France for the treatment of SIBO until recently, which is why these patients were treated with other antibiotics.
Main Results:
- The overall eradication rate in all participants was 53%
- Compared to the single antibiotic group, the rotating antibiotic group experienced:
- Higher SIBO eradication rates (70% vs 50.8%)
- Improved bloating
- Improved quality of life
- “In this study,the treatment of small intestinal bacterial overgrowth using rotating antibiotics was more effective than treatment using a single course of antibiotic. Remission was associated with improvement in both quality of life and bloating.”
Authors Conclusion:
- “We observed remission more frequently in patients receiving rotating antibiotics than in patients receiving a single antibiotic (70.0% vs. 50.8%) even if the study was not designed to answer this question.”
- “Despite the limited power of the statistical analysis due to the small number of patients in the rotating antibiotics group, a difference was found, suggesting a real benefit of rotating antibiotics compared to a single antibiotic.”
Clinician’s Comments
- This study found rotating antibiotics was more effective than using a single antibiotic for the treatment of SIBO. The rotating antibiotic group led to a 70% eradication rate of SIBO, which is higher than the Rifaximin eradication rate of 59-63% as demonstrated by a recent meta-analysis. Of course, we can’t sufficiently compare the results of a meta-analysis to 30 patients; however, the results are still insightful.
- It’s also worth mentioning that probiotics have been shown to be as effective as Rifaxmin in eradicating SIBO, as demonstrated by a recent meta-analysis [1, 2].
- Lastly, we have data to support the use of herbal antimicrobial agents that are similarly effective as Rifaximin in the treatment of SIBO [3].
- All of this data supports our clinical approach to treating SIBO. We recommend patients start with probiotics, followed by a rotating course of herbal antimicrobials. We find this often leads to both eradication of SIBO and improvement in their symptoms. We encourage patients to take probiotics alongside antimicrobials, as we find this increases their efficacy.
PMID 33868611
Study purpose
- To determine the effect of walking after meals on bloating.
Intervention:
- 94 individuals with bloating, randomized to:
- Prokinetic medication alone (domperidone)
- Prokinetic medication + 10-15 minute walk after each meal
- Walking protocol included “walking with hand clasped together behind the body and flexed neck (around 45 degree) posture without talking meanwhile”
- Walking protocol included “walking with hand clasped together behind the body and flexed neck (around 45 degree) posture without talking meanwhile”
Main Results:
- After 1 month, the addition of walking to the prokinetic medication led to greater improvements in various bloating severities:
- Severe to very severe bloating
- Control group (30% before treatment → 16% after treatment)
- Intervention group (33.2% before treatment → 0% after treatment)
- Very mild to no bloating
- Control group (12.2% before treatment → 42.8% after treatment)
- Intervention group (4.4% before treatment → 62.2% after treatment)
- Severe to very severe bloating
Authors Conclusion:
- “This study shows that physical activity could be effective in relieving abdominal bloating symptoms. In contrast to other means of treatment proposed for abdominal bloating and its related symptoms, it needs no materials or equipment and can be easily performed by any individual.”
- “Several mechanisms could be attributed to physical activity in order to exhibit this anti-bloating effect”:
- “It has been shown that exercise could impose a prokinetic effect on the gut.”
- “The abdominal muscle contractions occurring during the physical activity induce somato-autonomic reflex by which the propulsive motor activities of the GI tract are boosted, hence leading to increased luminal contents including fluid and gas transit.”
- “This increased intra-abdominal pressure applies a passive force on luminal gas facilitating its transit and evacuation.”
Clinician’s Comments
- This study illustrates a very simple intervention that patients can implement. Aside from improved bloating, we have data that supports that walking can improve blood sugar regulation, weight, blood pressure, mood, and reduce the risk of all cause mortality [4, 5].
- Daily walking, especially after meals, is a simple and free therapy that can have profound benefits on bloating and other important aspects of health.