TREATING CLINICIAN: Robert Abbott, M.D.
Patient Summary: Ashley
- Overview/Context:
- Ashley is a 79-year-old, cognitively sharp, borderline overweight woman who desires to take a more conservative, functional medicine approach to address her primary complaints of insomnia, depression, and reflux.
- She endorses an overall low allostatic load, reports feeling loved and supported with adequate time for herself, but still experiences frequent feelings of anxiety, depression, and irritability.
- Concerns and Goals:
- The patient desires to improve her sleep, lessen the strain of her anxiety and would be additionally grateful for any benefits regarding her symptoms of reflux and longtime arthritis.
- Initial Symptoms:
- Insomnia – Severe and frequent
- Depression – Frequent, less severe
- Reflux – Frequent, less severe
- Arthritis – Frequent, less severe
- Gas and Bloating – Infrequent, very mild
- Prior Diagnosis:
- GERD, 2005
- Hypothyroidism?, 2005
- Arthritis, 2006
- Oral Lichen Planus, 2008
- Lichen Sclerosus, 2008
- Obstructive Sleep Apnea, 2015
- Glaucoma, 2016
- Oral Cancer (related to lichen planus), 2017
- Medications:
- Atorvastatin 20 mg
- Levothroid 50 mcg
- Latanoprost (eye drops)
- Prior Surgical History
- 2017
- Surgery to address cancer affecting oral cavity, tongue and salivary glands, some lymph nodes removed
- 2017
- Prior Testing Summary:
- The patient does not provide us with any baseline labs.
- She cannot recall the labs performed approximately 20 years ago with an integrative-minded physician surrounding the diagnosis of hypothyroidism.
- Treatment History Summary:
- She reports some benefit previously from a lower carb, “low yeast” diet.
- She reports the historical use of antidepressants at times with unclear benefit.
- She reports no long term use (or desire) to use medication for symptoms of reflux.
- She has used probiotics historically with benefit, but has not expanded into other GI treatments.
- She is not currently following any nutritional pattern and flags for multiple areas of poor sleep hygiene (late to bed, late blue light, etc.).
- Onset, Timeline, and History:
- ~2005
- Reports an initial evaluation by a more integrative minded physician in the setting of symptoms of fatigue, depression, and insomnia
- Began following a lower carb, whole foods elimination style diet with the use of probiotics and other nutritional supplements with some benefit
- Feels she began thyroid medication at this time
- 2015
- Diagnosed with sleep apnea, has sought to treat with modalities outside of non-tolerated CPAP
- Present
- Endorses worsening insomnia and daytime fatigue
- Describes nighttime awakening with sense of dread “world coming to an end, feeling of guilt and shame”
- Has also noticed some slight esophageal burning mostly at night
- Continues with stable, but somewhat bothersome arthritis as well as burning on the tongue post oral surgery in 2017
- ~2005
- Clinical Questions/Comments:
- Are there any serious medical concerns requiring more immediate attention?
- Do I need any initial testing to initiate my treatment recommendations?
- Can I develop a “minimally disruptive” testing and treatment plan for this woman who is desiring a more conservative approach overall?
- Prognosis:
- I expect her to do well with a focus on implementing a more nutrient dense diet, improving sleep hygiene and using supportive GI therapies. She may also be able to stop/decrease thyroid medication.
- Differential Dx
- Dietary & Lifestyle
- Dietary mismatch
- Poor sleep hygiene, timing, or duration
- Sedentarism
- Gastrointestinal
- Dysbiosis
- Laryngopharyngel reflux
- Gastritis vs. Hypochlorhydria
- Histamine intolerant
- Hormonal
- Incorrect thyroid dx and/or unnecessary thyroid medication vs. Hypothyroidism
- Nutritional
- Nutritional Deficiencies (tba)
- Metabolic
- Mild overweight
- Dyslipidemia – On Statin
- Sarcopenia
- Other Considerations
- Sleep
- Sleep disordered breathing, History of OSA
- Need for sleep CBT
- Infectious/Inflammatory
- Oral health Imbalance – History of oral lichen planus, oral cancer
- Toxic
- Heavy metal toxicity – Historical mercury amalgams and oral pathology
- Sleep
- Dietary & Lifestyle
- Recommended Testing
- I am NOT recommending any initial testing
- Clinical Decision Making
- Despite a relatively minimal GI symptom burden, I am speculating there is likely some underlying gut dysfunction connected to her neuropsychological symptoms of insomnia, anxiety, and depression.
- I am also curious given the relatively low dose of thyroid medication, her symptoms of insomnia, and the unclear circumstances of diagnosis with a more “natural” provider if she actually needs thyroid medication.
- At this present time, I do not see any medical urgencies requiring immediate evaluation. In addition, I feel that we can overall simplify our initial treatment approach by forgoing blood chemistry (or other testing) until a later date — It is important to note that I DO have interest in her thyroid levels and nutritional status.
- Treatment Hierarchy
- Relaxed Paleo Diet with optional intermittent fasting
- Sleep Hygiene vs. CBT-I
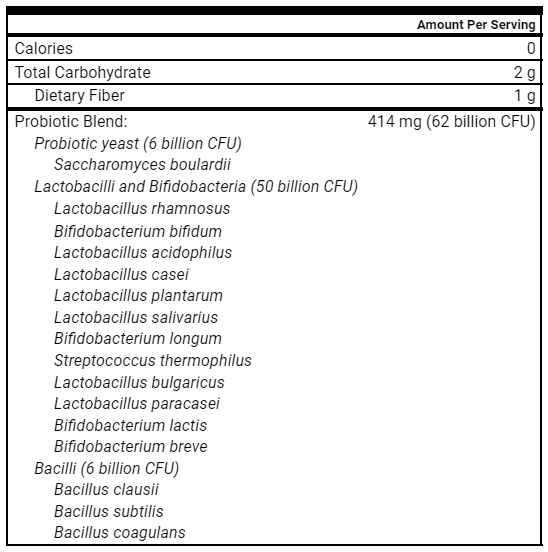
- Triple Probiotic Therapy
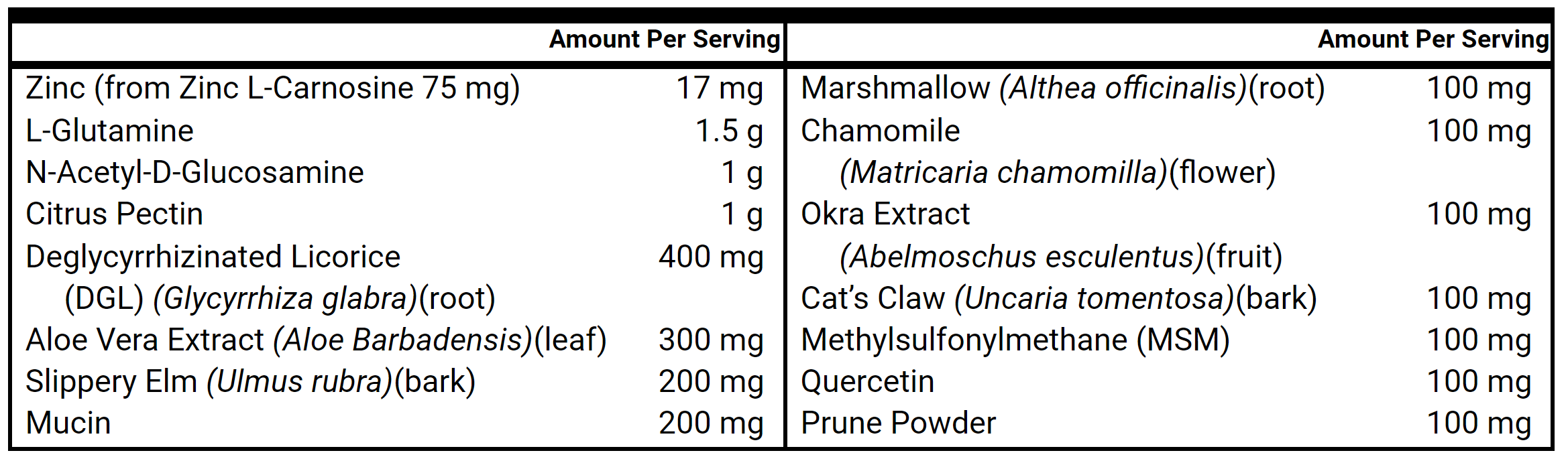
- Gut Healing Nutrients
- Adaptogens
- Melatonin
- Theanine
- Nutrient Replacement Therapy
- Elemental Diet (optional)
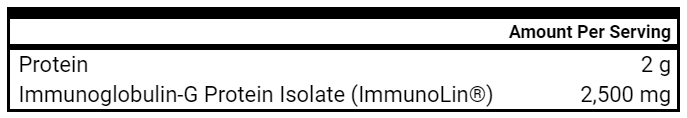
- Immunoglobulins
- MCAS and Histamine Intolerance Supports
- Thyroid Hormone Discontinuation Trial
- Myofunctional Therapy
- Ancestral Stressors (Cryotherapy)
- Herbal Antimicrobials
- Initial Treatment Recommendations
- Diet & Lifestyle
- Relaxed Paleo Diet, Encourage Carbs ~100 grams
- Can explore intermittent fasting as desired
- Can use Elemental Diet as optional AM meal replacement 2-3x weekly
- Sleep hygiene practices
- Future Considerations for CBT-I
- Walking in nature 2-3x/wk (preferably with a friend)
- Nutritional Replacement Therapy
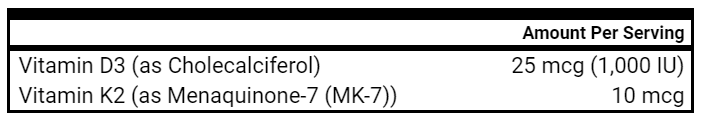
- Vit D/K
- Vit D/K
- GI phase 1
- Probiotic triple therapy
- Gut Healing Nutrients (powder)
- Melatonin 3 mg
- Probiotic triple therapy
- Adaptogens
- Theanine, Magnesium, GABA, Relora
- Medication
- Keep Levothroid at 50 mcg
- Follow-up Plan
- 5-6 weeks
- Diet & Lifestyle
- Clinician Treatment Summary
- Ashley is a pleasant older woman who primarily complains of insomnia, anxiety and depression in the setting of suboptimal sleep hygiene and dietary indiscretion. As she describes her diet, she consumes a high volume of carbohydrates with inadequate animal foods and protein. I see there is much room for progress if we focus first on some diet and lifestyle foundations.
- Given her more conservative treatment desires, I would like to build off her previous successes of following a lower carb type Paleo diet with the use of probiotics. It is usually more ideal to build treatment plans based on previous successes, or at the very least, within areas of knowledge and awareness for the patient as compared to brand new, intricate interventions.
- In addition to our lifestyle foundations, I feel that we can also see some progress with the utilization of triple probiotic therapy combined with gut healing nutrients. She also appears to be a candidate for melatonin which could both help her sleep and provide benefit for suspected LPR. I typically use doses between 3-6 mg. I have also included an additional adaptogenic product to explore that may help with some of her restlessness and insomnia.
- As we progress with treatment, we can consider additional interventions to address her sleep disordered breathing. I will also consider testing her thyroid function at a later date to inform a potential thyroid hormone discontinuation trial.
- Patient Self-Assessment
- Reported a 1-2 day intestinal infection shortly after our last visit (had not yet started any aspects of treatment)
- Used elemental diet during the early recovery period with benefit
- Does not feel she has any residual digestive distress
- Introduced probiotics and gut healing nutrients and feels this may have minimized symptom continuation/helped with the recovery period as well
- Reported that she experienced a negative reaction including fatigue and cognitive fatigue from carbohydrate restriction, but has now been doing well with a more moderate level of carbohydrates within the relaxed Paleo diet
- Insomnia
- Feels that her overall sleep and restlessness has improved
- Attributes some benefit to melatonin and changing her evening routine
- Has not used other adaptogens long enough to discern benefit, but no clear negative reactions at this point
- Reflux
- Feels that this may be better at night – attributes a potential effect with Melatonin
- Anxiety/Depression
- Reports no major changes in this area
- Reported a 1-2 day intestinal infection shortly after our last visit (had not yet started any aspects of treatment)
- Clinical Decision Making
- Ashley has responded well to the initial dietary recommendation, troubleshooting with our nutritionist to find a balanced intake of carbohydrates while prioritizing more whole foods from a relaxed Paleo diet template.
- There are some early signs of benefit from our supplemental interventions including triple therapy probiotics, gut healing nutrients, and melatonin.
- While she had what appeared to be a foodborne intestinal infection, she has recovered well and I do not see any need to further modify our treatment or explore testing with the recent GI illness.
- I expressed to the patient that I would like for her to stick with some of the dietary, lifestyle, and supplemental treatments, as I expect them to provide continued benefit and further synergy with more time. This being said, I offer suggestions on food reintroductions to consider based on her specific preferences. I suggest she focus on noticing if certain foods disrupt her digestion, sleep, or are connected with more notable anxiety/restlessness.
- I do not want perfection to be the enemy of good when it comes to diet and expect that perhaps she will gain further psychological benefit with some specific food reintroductions.
- Updated Treatment Recommendations
- Diet & Lifestyle
- Continue with moderate carb relaxed Paleo diet with the elemental shakes as a meal replacement as desired
- Supplementation and Medication
- Continue with the previous recommendations with no changes to Levothroid
- Follow-up Plan
- 5-6 weeks
- Diet & Lifestyle
- Patient Self-Assessment
- Reports her health as 80/100 and 30% better from when we began to work together
- Has continued to follow most of the relaxed Paleo diet with some food reintroductions (including dairy) without noticeable digestive distress or worsened neuropsychological symptoms
- Notes more normality to her stools, more formed/normal consistency, and regularity of timing
- Insomnia
- Feels that her sleep has continued to improve
- Reports activity during the day, sticking to an earlier bedtime and using melatonin has been helpful
- She notes a notable decrease in restlessness – “My body is just in a more relaxed state.”
- She has not used other adaptogens or L-Theanine in isolation as she has been feeling much better overall and with her sleep – does not feel she needs them
- Reflux
- Stable improvements, very infrequent to never
- Anxiety/Depression
- Reports no major changes in this area
- Clinical Decision Making
- It appears that Ashley has noted accumulated benefits from the continued use of the gut based supplementation, being more regimented with her sleep hygiene, following the broader guidelines of the relaxed Paleo diet and even being able to introduce some foods that have improved her overall well-being. This has encouraged her to stick to other key aspects of the dietary and lifestyle recommendations.
- She has likely reached a place where we can peel back some supplements into a more maintenance regimen and explore some “new” baseline labs to assess her thyroid function, metabolic health and nutritional status with this current way of living – perhaps in preparation for a discontinuation trial of her thyroid replacement medication.
- Updated Treatment Recommendations
- Diet & Lifestyle
- Continue with moderate carb relaxed Paleo diet with the elemental shakes as a meal replacement as desired
- Nutritional Replacement Therapy
- Vit D/K
- GI phase 1
- Probiotic triple therapy – decrease to 3x weekly
- Gut Healing Nutrients (powder) – decrease to 3x weekly
- Melatonin 3 mg
- Adaptogens
- Theanine PRN
- Medication
- Keep Levothroid at 50 mcg
- Lab Testing and Follow-up Plan
- CBC with differential, CMP, GGT
- TSH, Free T4, Free T3, TPO
- a1c, lipid panel, apoB
- Iron profile, Vitamin D, B12, homocysteine
- Follow-up in 6-8 weeks
- Diet & Lifestyle
Clinical Rule and Final Clinician Comments
1. Clinical Rule: Start with the least invasive treatments first – diet and lifestyle.
Consider less food restrictions in the pediatric and more elderly population to improve overall adherence to your treatment recommendations
2. Clinical Rule: Treat diet, lifestyle, and gut health before the thyroid.
Additionally, consider that treatment TSH targets for elderly patients may be higher than typical normal ranges. (Patients with normal Free T4 and no overt symptoms may be fine with a TSH between 4.5 and 7.0.)
3. Clinical Rule: Correcting diet, lifestyle, and GI health often improves nutrient imbalances.
Consider certain laboratory assessments and more rigorous nutritional replacement interventions after the implementation of initial therapies targeted at improving diet, lifestyle and gut health
Patient Summary: Steve
- Overview Context:
- Steve is a 24 year old male who has been experiencing rapidly worsening diarrhea, weight loss, fever, and fatigue.
- Steve’s sleep has been markedly disrupted given nighttime bowel movements and his overall levels of perceived stress are high given these health challenges.
- Concerns and Goals
- The patient desires to address the severe diarrhea and ongoing weight loss and clear diagnosis/understanding as to why.
- He desires guidance on a dietary pattern that can support him in achieving these ends.
- Initial Symptoms:
- Diarrhea – Severe and frequent
- Sudden Weight loss
- Fatigue – Severe and frequent
- Nausea – Frequent and moderate in intensity
- Fever – Infrequent, but severe
- Headaches – Frequent, less severe
- Prior Diagnosis:
- Ankylosing Spondylitis (AS), 2013
- Celiac Disease – recent diagnosis in connection with diarrhea and weight loss
- Medications:
- Enbrel, weekly injection (for AS)
- Prior Surgical History
- Root canal on tooth with long term infection (Age 8-16)
- No Hx of Abdominal or musculoskeletal surgeries
- Prior Testing Summary:
- Negative Stool O&P
- Negative PCR for cryptosporidium and giardia
- Markedly elevated serum IgA
- NEGATIVE Celiac Screen
- WBC: 14.9, Neutrophilic Predominance
- Platelets: 517
- Treatment History Summary:
- Reports Enbrel has been helpful for his AS symptoms (stable now)
- Followed a whole foods diet for most of adolescence
- Followed a more carnivore and ketogenic diet in the past directed at AS symptoms
- Recently followed a stricter gluten-free diet without significant change in symptoms
- Has not pursued supplemental or GI directed treatment as of yet
- Onset, Timeline and History:
- ~2008
- Noted symptoms of knee and hip pain related to playing baseball
- 2008-2012
- Noted worsening flares of joint pain
- Labs noted with elevated WBC
- Seen by Rheumatologist at age 16 who diagnosed with AS via X-rays, clinical history, and HLA B27 +
- Started Enbrel which was initially effective
- ~2018
- Started to notice Enbrel was less effective
- Connected eating more processed, inflammatory foods as main culprits
- Made some dietary modifications at this time towards more Paleo, keto, carnivore
- Early 2021 – Present
- Started to notice worsening fatigue, fevers and headaches
- Diarrhea increase to as many as 20 episodes daily, night time urgency and frequency
- Started to adopt a more strict gluten-free diet and noticed some slight improvements, such that stools are more typically 8-10x during day, 4x nightly
- Denies noticing a consistent pattern of blood in stools
- ~2008
- Clinical Questions/Comments:
- Does this patient actually have Celiac Disease? Or another GI pathology?
- Is his disease severe enough to warrant more urgent or emergent evaluation?
- What is the quickest, more reliable testing I can perform to better elucidate the reasons for his symptoms?
- Prognosis:
- Cautiously optimistic given his more severe symptoms currently
- Differential Dx
- Dietary & Lifestyle
- Disrupted sleep given urgent, frequent BM’s
- Sedentarism – Limited by fatigue
- Gastrointestinal
- IBD
- Dysbiosis
- GI Pathogen
- EPI
- Hormonal
- HPA Axis Dysregulation given weight loss, caloric insufficiency
- Nutritional
- Nutritional Deficiencies
- Likely multiple and possibly severe
- Nutritional Deficiencies
- Metabolic
- Sarcopenia – Loss of muscle mass
- Other Considerations
- Infectious/Inflammatory
- Oral health imbalance – History of root canal
- Known history of AS on Enbrel
- Toxic
- Heavy metal toxicity – possible autoimmune triggers
- Environmental toxicity – possible autoimmune triggers
- Infectious/Inflammatory
- Dietary & Lifestyle
- Recommended Testing
- GI MAP (Calprotectin)
- CBC with differential, CMP, GGT
- Iron Profile, Vitamin D, B12, Folate, Homocysteine, Magnesium
- hs-CRP
- Clinical Decision Making
- In looking at Steve’s clinical picture with the severe diarrhea, weight loss and fevers with a past history of AS, I am quite suspicious of a diagnosis of IBD and NOT Celiac. Interestingly, as I review his past labs, his Celiac testing was NEGATIVE. It appears in discussion with Steve that the clinician ordering the celiac screen must have misinterpreted or misread the test that showed markedly elevated serum IgA, but NOT evidence of celiac disease. Given the severity of his symptoms, I urge them to complete a GI MAP stool test as soon as possible, but consider a more urgent/emergent evaluation with a local provider to get an urgent GI referral. I also have recommended some baseline labs to evaluate the current activity of his immune system and his nutritional status given the severe diarrhea and weight loss.
- Treatment Hierarchy
- Elemental Diet
- Paleo vs. AIP vs. SCD
- Triple Probiotics
- L-Glutamine
- Additional Gut Healing Nutrients
- Boswellia, Curcumin
- Immunoglobulins
- MCAS Supports
- Initial Treatment Recommendations
- Diet & Lifestyle
- I discussed and shared handouts for Paleo, Autoimmune Protocol Diet (AIP) and Specific Carbohydrate Diet to give guidance on a dietary approach to implement at this time.
- I encouraged a 3 day reset of the Elemental Diet at eucaloric levels followed by a transition to a hybrid elemental diet with one of the dietary approaches discussed above.
- Nutritional Replacement Therapy
- None at this time
- GI phase 1
- Probiotic triple therapy, 1 packet, 2x daily
- L-Glutamine Powder, 1-2 tsps, 1-2x daily
- Immunoglobulins, 1-2 scoops, 2x daily
- Curcumin, 2 pills, 2x daily
- Probiotic triple therapy, 1 packet, 2x daily
- Follow-up Plan
- 3-4 weeks – upon receiving lab results
- Diet & Lifestyle
- Clinician Treatment Summary
- At this stage, I am strongly suspecting severe IBD (and NOT Celiac) and am initiating a comprehensive treatment based on this suspicion. I will obtain the GI MAP stool test for confirmatory purposes, expecting to see occult blood and markedly elevated calprotectin. While I have concerns about the patient’s weight loss, a short term Elemental Diet reset carries the potential benefit of beginning to calm the severe GI dysfunction. A therapeutic short reset could then combine – transition into a hybrid diet. I have advised the patient to follow-up sooner than typical given the severity of his symptoms.
- Patient Self-Assessment
- Reports his health as 70/100 and 40% better from just a few weeks ago
- Implemented a modified fast with the elemental diet for 3 days and then transitioned to a modified hybrid diet with AIP. This reset resulted in a notable shift in GI symptoms.
- Notes nuts are clearly problematic
- Higher volume of sugars, fruits seems to aggravate arthritis
- Reports a small volume of nightshades on the weekend without major symptom aggravation
- He introduced all of the GI supplements including:
- Triple Probiotics
- Immunoglobulins
- L-Glutamine
- Denies any noticeable adverse events or negative reactions to the supplements
- Diarrhea
- Significant decrease in frequency, more normalizing stool consistency
- Fatigue
- Markedly improved
- Fevers
- Resolved
- He reports with the more rapid change in symptoms that he has returned back to living on his own with plans to move in with his fiancée.
- Lab Results
- GI MAP
- Calprotectin: >3000
- Occult Blood >200
- Moderate Dysbiosis
- Elastase: 389
- Blood Chemistry
- WBC 8.3, Neutro 56%, Monocytes: 13%
- Hgb: 12.5, MCH: 25.6
- Platelets: 724
- Total Protein: 6.9
- Globulin: 4.1
- Albumin: 2.8
- Alk Phos: 155
- ALT: 27
- GGT: 77
- hs-CRP: 213.01
- Homocysteine: 11.9
- Folate 2.8
- B12: 1043
- Vitamin D: 42.3
- Copper: 165
- Zinc: 101
- TIBC: 219
- Ferritin: 684
- Iron Sat: 12%, Serum Fe: 27
- GI MAP
- Lab Interpretation and Diagnosis
- Steve’s GI MAP shows the expected markedly elevated calprotectin and occult blood amidst moderate dysbiosis. There are no indications for pathogens or potential pathogens. His stool test is consistent with inflammatory bowel disease.
- Steve’s bloodwork shows a markedly profound acute inflammatory response with multiple inflammatory mediators or acute phase reactants being elevated including WBC count, platelets, ferritin, hs-CRP and serum copper. His iron metabolism is disturbed secondary to active blood loss and inflammation resulting in low bioavailable iron and decreasing hemoglobin and RBC volume. Nutritionally, he is somewhat better than expected with the most prominent finding being markedly low folate and concurrently high homocysteine (this is a possible sequelae of his previous carnivore type diet amidst intestinal malabsorption). His albumin is also low secondary to GI losses.
- Refined Differential Dx
- Dietary & Lifestyle
- Disrupted sleep given urgent, frequent BM’s
- Sedentarism – Limited by fatigue
- Gastrointestinal
- IBD – elevated calprotectin with occult blood
- Dysbiosis – moderate on GI MAP
GI Pathogen – negative on GI MAPEPI – normal elastase
- Hormonal
- HPA Axis Dysregulation given weight loss, caloric insufficiency
- Nutritional
- Nutritional Deficiencies
- Iron
- Folate
- Protein
- Nutritional Deficiencies
- Metabolic
- Sarcopenia – Loss of muscle mass
- Other Considerations
- Infectious/Inflammatory
- Oral health imbalance – History of root canal
- Known history of AS on Enbrel
- Toxic
- Heavy metal toxicity – possible autoimmune triggers
- Environmental toxicity – possible autoimmune triggers
- Infectious/Inflammatory
- Dietary & Lifestyle
- Clinical Decision Making
- Steve has responded remarkably well to the initial recommendations of the elemental diet reset to hybrid with AIP combined with triple probiotics, L-Glutamine, immunoglobulins, and curcumin. His testing showed expectant results regarding the clinical diagnosis of IBD, acute inflammation and nutritional deficiencies. Given his positive response and healing gut, I feel he can now effectively utilize some targeted nutritional supplementation while we seek to continue the core components of our treatment plan. He appears out of the acute, most worrisome clinical state, but I will continue to encourage establishing a visit with a local GI to consider a colonoscopy in the near future.
- Updated Treatment Recommendations
- Diet & Lifestyle
- Continue hybrid elemental diet with Autoimmune Protocol Diet (AIP).
- Nutritional Replacement Therapy
- Electrolytes
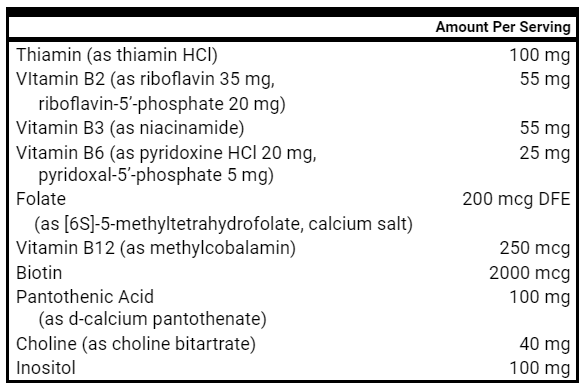
- B Complex
- Hydrolyzed Beef Protein
- Electrolytes
- GI phase 1
- Continue previous recommendations
- Lab Testing Follow-up Plan
- Blood Chemistry
- CBC with differential, CMP, GGT
- Iron Profile, Folate, Magnesium
- hs-CRP
- 8 weeks – after repeat lab results
- Blood Chemistry
- Diet & Lifestyle
Clinical Rule(s) and Final Clinician Comments
- Clinical Rule: Start with the least invasive treatments first – diet and lifestyle.
Even in settings of more acute and problematic symptom presentation, do not forget about the utility of a solid dietary foundation. In our patient with suspected IBD, evidence exists for the benefits of an elemental diet amidst other dietary protocols such as Paleo, AIP, and SCD.
- Clinical Rule: Correcting diet, lifestyle, and GI health often improves nutrient imbalances.
In this case, we have a patient with severe IBD and lab work indicating multiple nutritional deficiencies secondary to compromised intake, over-utilization in an inflamed state, and malabsorption. By beginning to heal his gut and move to a more nutrient-dense and compatible way of eating, we can correct nutritional deficiencies and be targeted in our additional nutritional supplementation.
- Clinical Rule: Give time for healing before adding multiple new or complex treatments.
Steve has begun to respond really well rather quickly which is very encouraging to see. While I provided him with a relatively robust set of initial recommendations given his more perilous clinical state, it is important to not overwhelm the patient and deviate from an initial core that is providing benefit and that should continue to provide benefit over time. Avoid treatment overwhelm and unnecessary novelty.
Clinical Question
- Is hormone replacement therapy (HRT) safe for women with a previous diagnosis of breast cancer?
Functional Medicine “Bias”
- Bioidentical hormone replacement is “natural” and safer than the equine estrogens and progestins (ex. medroxyprogesterone acetate) used in previous studies (observational and interventional) indicating potential harm (risk of primary or recurrent cancer).
What Does The Evidence Actually Suggest?
- HRT is associated with an INCREASED risk of breast cancer recurrence in those with previously hormone receptor POSITIVE cancer (progesterone and estrogen).
- HRT with synthetic progestogens is NOT associated with an increased risk of breast cancer recurrence in those with previously hormone receptor NEGATIVE cancer.
- Note: These conclusions are drawn from a meta-analysis of 4 randomized control trials using either:
- Estrogen alone
- Estrogen and Progestogens (Medroxyprogesterone acetate (MPA) or norethisterone)
- Tibolone (synthetic steroid)
- Note: These conclusions are drawn from a meta-analysis of 4 randomized control trials using either:
- We have identified insufficient evidence regarding the association of micronized progesterone and the risk of breast cancer recurrence.
What Should I Do In Clinical Practice?
- Using the conservative, precautionary principle, you should seek to implement a TERRAIN focused approach, exhausting diet, lifestyle, gut directed and other supportive therapies to minimize symptoms of hormonal deficiency in ALL patients with a history of breast cancer REGARDLESS of hormone receptor status or FORM (bioidentical or synthetic) of HRT.
- Consider, through shared decision making with each individual patient, the implementation of HRT amidst previously implemented low risk therapies in those with a history of hormone receptor NEGATIVE breast cancer.
- When choosing a form of progesterone-based HRT, micronized progesterone may be a safer alternative to utilize than progestins – MPA or norethisterone.
- In addition, treatment with micronized progesterone for <5 years (as compared to >5 years) appears safer with regards to primary (not recurrent) breast cancer risk.
Primary Study Title
- Safety of systemic hormone replacement therapy in breast cancer survivors: a systematic review and meta-analysis
Intervention Details
- 4 RCTs, 4,050 patients that investigated the risk of breast cancer (BC) recurrence with the use of HRT in BC survivors
- Overall, 2,022 patients were randomized to receive HRT (estrogen, estrogen/progestogen combination or tibolone) and 2,023 to the control group (placebo or no HRT)
- HRT significantly increased the risk of BC recurrence compared to placebo (HR 1.46, 95% CI 1.12-1.91)
- More effect if hormone-receptor positive BC
- But, NO effect if hormone-receptor negative BC
Study Author’s Primary Conclusion
- “Our meta-analysis reported that the use of systemic HRT cannot currently be recommended for BC patients experiencing symptoms related to estrogen deficiency, particularly in the case of hormone receptor-positive disease, calling for future research to draw up safe and effective alternatives for the physician’s armamentarium against these frequent side effects.”
Interesting Notes
- A study published in JAMA in 2020 by Chlebowski et. al showed that women who received conjugated equine estrogen ONLY following hysterectomy were significantly LESS likely to develop breast cancer or experience breast cancer related mortality than those receiving placebo.
- Additionally, those receiving conjugated equine estrogen AND medroxyprogesterone acetate with A UTERUS experienced an increased risk of breast cancer, but NO INCREASED RISK in breast cancer associated mortality.
- While data remains limited, a separate systematic review reviewing bioidentical or micronized progesterone suggests that micronized progesterone (oral or vaginal) DOES NOT INCREASE risk of breast cancer over a 5 year or less treatment period.
- Estrogen and micronized progesterone treatment for >5 years however, MAY BE associated with an INCREASED risk of developing breast cancer.
Secondary Study Titles
- Association of Menopausal Hormone Therapy with Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women’s Health Initative Randomized Clinical Trials
- The impact of micronized progesterone on breast cancer risk: a systematic review
Final Comments
HRT is a controversial topic in both traditional and functional medicine. Those in more “natural” medicine commonly suggest that bioidentical hormones are “better” than “synthetic” medications. However, almost all the data on HRT in large scale studies is taken from the “synthetic” medications. As the studies above highlighted, there is conflicting evidence for the benefit or harm of HRT in postmenopausal women with or without a history of breast cancer. Be careful in practice to not overstate claims or inadvertently tell patients there is supporting evidence that does not actually exist for a given therapy. Conversely, we must also recognize that even if a certain therapy does not have a large body of evidence supporting its use, it may still be an effective and practical treatment to consider. Please be conservative and conscientious in your approach to HRT, exhausting diet, lifestyle, gut and additional supplementation before considering this therapy in certain appropriate populations. When prescribing medications, seek to apply the principle of minimal effective dose for the minimal period of time necessary to achieve the desired therapeutic outcome.
Clinical Question
- How do I treat subclinical hypothyroidism?
Functional Medicine “Bias”
- We have observed multiple biases and ideas that seem to circulate in “natural” medicine that are worth highlighting:
- Tighter, more optimal thyroid hormone ranges should be used to ensure you do not “miss” thyroid dysfunction.
- Combination or desiccated replacement therapy is more “natural” and thus should be used preferentially.
- Since thyroid hormone is essential for all cellular functions, one must FIRST “balance” hormones before addressing other areas of diet, lifestyle of gut health for example.
What Does The Evidence Actually Suggest?
- An age-dependent “upper limit of normal” TSH should be implemented to better categorize those with subclinical hypothyroidism (SCH).
- The majority of RCTs have shown minimal to no benefit in quality of life, symptoms of fatigue, cognition or mood when individuals with SCH or mild thyroid hormone dysfunction are treated with hormone replacement.
- Observational data does highlight increased cardiovascular mortality and abnormal cardiometabolic parameters in patients with SCH or mild thyroid dysfunction.
- Of the interventional data available for cardiovascular and cardiometabolic outcomes, patients, depending on age, with TSH levels between 6.5-10 may receive benefit from replacement medication.
- Of the 2 studies available assessing the subject, the difference in weight between euthyroid and patients with mild thyroid dysfunction was clinically insignificant (difference of 1-2 kg).
What Should I Do In Clinical Practice?
- Categorize your patients with SCH by age-dependent upper limits of normal for TSH
- Identify the presence of historical or current thyroid dysfunction (TPO antibodies, abnormal thyroid ultrasound)
- Identify any previous labs suggesting the duration of the abnormal TSH findings
- Apply the non-pharmacological treatment approach to patients with thyroid dysfunction as outlined in the Thyroid Treatment Algorithm (FFMR May 2021)
- Consider thyroid hormone replacement for patients with SCH based on age-dependent upper limits of normal for TSH, current symptomatic complaints, and underlying risks for cardiovascular disease or cardiometabolic dysfunction
- T3 or desiccated, combination thyroid hormone replacement is NOT recommended in the elderly, pregnant or those with underlying cardiac disease (arrhythmias, heart failure and valvular disease).
Primary Study Title
- Treating hypothyroidism is not always easy: When to treat subclinical hypothyroidism, TSH goals in the elderly, and alternatives to levothyroxine monotherapy
Primary Study Graphics
Study Author’s Key Conclusions
- “Some of this dissatisfaction (with their treatment) is unintentionally caused by well-meaning practitioners who enthusiastically begin patients on levothyroxine for minimal hypothyroidism, with the promise that it will address their symptoms. Unfortunately, the evidence suggests that few such patients will experience long-term benefit in their symptoms.”
- Another study of 929,684 subjects demonstrated that in 2001 that approximately a quarter were treated due to TSH levels between 5 and 10 mIU/L, while by 2015 approximately half of the patients being treated had TSH values between 5 and 10 mIU/L [63]. It therefore seems likely that we are enriching the population of patients who carry a diagnosis of hypothyroidism with subjects who have symptoms and minimal TSH elevation, whose symptoms are unlikely to be responsive to treatment with levothyroxine.
Interesting Notes
- A study published in December 2021 followed a cohort of 431 healthy, (euthyroid) control patients and 225 patients with SCH WITHOUT providing any treatment.
- After 6 months
- 12.2% developed overt hypothyroidism (High TSH, Low Free T4)
- 13.4% remained with SCH
- 73.8% became euthyroid
- Risk factors for transition to overt hypothyroidism
- Female
- +TPO
- TSH > 6.9 mIU/L
- Free T4, Free 3 in lowest tertile of reference range
Secondary Study Title
- Transient high thyroid stimulating hormone and hypothyroidism incidence during follow-up of subclinical hypothyroidism
Additional References and Reviews
Final Comments
The appropriate diagnosis and treatment of hypothyroidism (and subclinical hypothyroidism) continues to be a controversial area within all circles of medicine. In general, we are observing overdiagnosis and overtreatment in patients seeing “natural” and functional medicine providers. However, research cited in the primary study analyzed in this review shows a marked increase in prescriptions for patients with TSH’s between 5-10, suggesting an even larger issue of overtreatment in patients seeing providers of all backgrounds. In seeking to bridge the divides between over and under diagnosis, as well as over and under treatment, we have developed and continue to refine the Thyroid Treatment Algorithm with additions noted here for SCH.
Assume Your Patient Knows Something You Don’t
I provide this reflection as a derivative of a “rule” discussed by Jordan Peterson in his book 12 Rules for Life. We have all certainly experienced the challenges when a suffering patient brings well-intentioned, but discombobulated ideas to our therapeutic encounters. While the therapeutic relationship with any patient is predicated on the understanding that you, the practitioner, have knowledge and insights that are of perceived value to the patient, we must not forget that the patient is also equipped with knowledge that may be of value to us. We can easily recognize that the patient is the “expert” of their personal experience, the only person capable of articulating important ideas about their health, but we can struggle to be receptive to new information and ideas that the patient may share as part of their own research efforts.
As clinicians, we must be both receptive and discerning, curious with openness, but precise with our actions and speech. I have found that amidst a remarkably “busy” clinical schedule, my most important “continuing medical education” comes from the observation of my patients (both before and during treatment) AND the exploration of ideas or even specific products shared by my patients.
Do not falsely assume that valuable insights and clinical information follows an unidirectional funnel towards the patient.
Assume Your Patient Knows Something You Don’t.