TREATING CLINICIAN: ROB ABBOTT, M.D.
Patient Info:
- Catie is a 34 y/o active and driven female experiencing chronic hives
- She has recently increased an increased allostatic load secondary to her (outdoor) work obligations and has noted some irregular (skipped) menstruation
- Chief Complaints:
- Hives – frequent and severe
- Heartburn – infrequent, but severe
- Lower abdominal discomfort – infrequent, but severe
- Nausea – infrequent, but severe
- Prior Diagnosis:
- Arnold Chiari Type 1/Scoliosis 1989 – Corrected via surgery at 2 years old
- Chronic Idiopathic Urticaria 12/2009
- Thyroid Nodule 06/28/2013
- Amenorrhea 06/28/2013
- Peripheral Neuropathy 06/28/2013
- GERD 06/28/2013
- Medications:
- Claritin 10 mg daily
- Benadryl 25-50 mg as needed when hives are severe
- Omeprazole 20 mg capsule daily
- Prior Surgical History:
- Arnold Chiari Type 1/Scoliosis 1989 – Corrected via surgery at 2 years old
- No History of abdominal surgeries
- Prior Testing Summary:
- March 2021 Labs
- WBC: 6.9, normal diff
- Hgb: 12.1
- RBC: 4.33
- MCV: 85.3
- TSH: 0.83
- a1c: 5.7
- TC: 190, Trigs: 67, HDL-C: 86, LDL-C: 91, VLDL-C: 13
- March 2021 Labs
*I am not convinced the a1c is truly reflective of her blood sugar and may be artificially high*
- Treatment History Summary:
- Recently followed Carnivore Diet with some further success beyond baseline lower carb Paleo
- Feels Claritin and Benadryl have been effective for hives when used
- Has not yet tried natural antihistamines or GI specific treatments
- Has not yet worked with an integrative/functional type provider
- Onset:
- December 2009 – Chronic hives began as a senior in high school
- Was working with horses and noted fairly severe seasonal allergies at the time
- Has reported daily hives since this time, caused/worsened by scratching, pressure from clothes, sometimes movement and heat
- Began mainly on back and have migrated to essentially all body parts at some point
- 2012-2013 – Experienced a multitude of symptoms including IBS, reflux, joint pain, chronic fatigue, brain fog, nausea and amenorrhea
- Was doing triathlons at the time, instructed to gain weight by endocrinologist
- Went gluten-free with some benefit of symptoms
- 2019 – Followed ketogenic diet that improved much of her GI symptoms, but hives were still very much present
- 2021 – Followed a carnivore type diet with resolution of residual GI symptoms – nausea and GERD, but still not noticeable improvements with the hives
- December 2009 – Chronic hives began as a senior in high school
- Clinical Questions/Comments:
- Is it reasonable to suspect that there is underlying GI dysfunction behind her chronic hives?
- Will the patient require a stool test to identify a possible GI source for her chronic hives?
- Catie has implemented a series of increasingly restrictive dietary patterns with some success for many GI-based symptoms. She has yet to obtain much significant testing and also has not yet done any natural antihistamine treatments or GI directed therapies
- Prognosis:
- Expect her to do well with a combination of natural antihistamine treatments alongside supportive GI interventions
- Differential Dx:
- Post Infectious-IBS, History of GI Infections
- Gastritis
- Hypochlorhydria – Iatrogenic
- Female hormone imbalance – amenorrhea
- Low normal, decreased oxygen-carrying capacity
- High allostatic load
- GI pathogen
- Histamine intolerant
- MCAS
- Recommended Testing:
- GI MAP
- Clinical Decision Making
- Catie is a very active and driven young female with a history of chronic idiopathic urticaria that I suspect is being driven by an underlying gut pathogen and/or gut dysbiosis. Because of the chronic nature of her hives, I would like to begin our exploration for potential parasites via a GI MAP.
- Treatment Hierarchy
- Low Carb Paleo Diet (Current)
- Probiotics (Soil-based, S. Boulardii)
- MCAS Support
- Immunoglobulins
- Gut Healing Nutrients
- Digestive Support
- Anti-parasitics, Herbal Antimicrobials
- Adaptogens
- Elemental Formula
- Nutritional Replacement Therapy
- Initial Treatment Recommendations
- Diet and Lifestyle
- Continue current Low Carb Paleo Diet
- Supplements
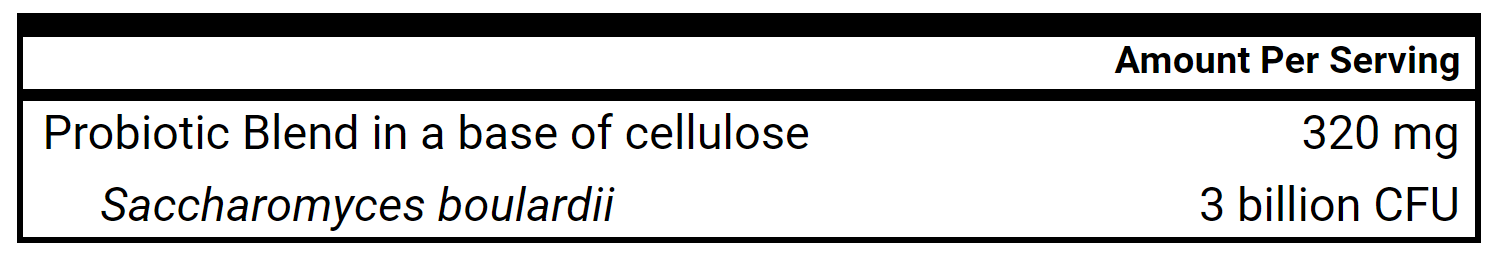
- S. Boulardii
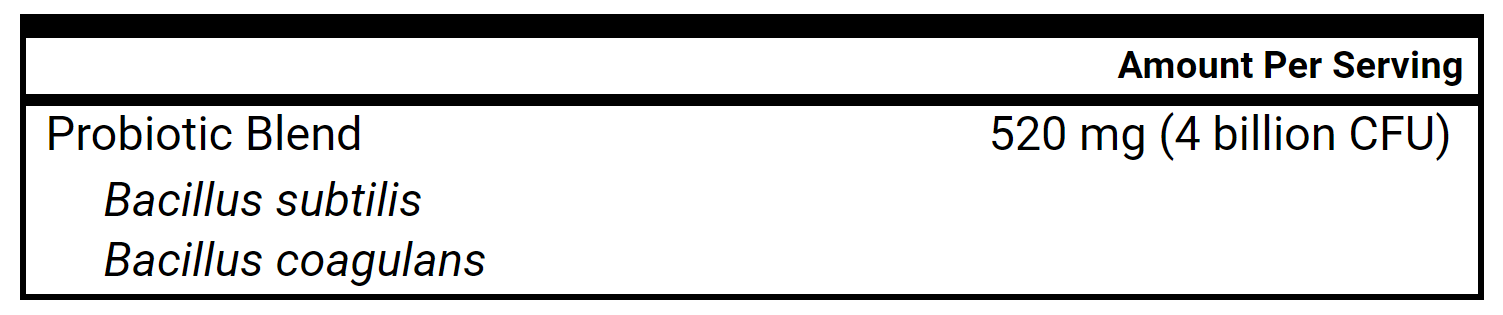
- Soil-based Probiotics
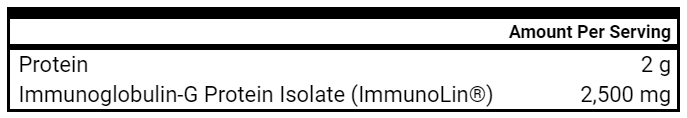
- Immunoglobulins
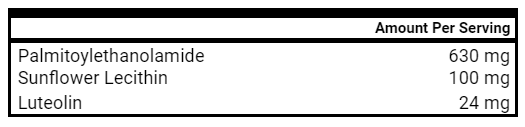
- PEA + Luteolin
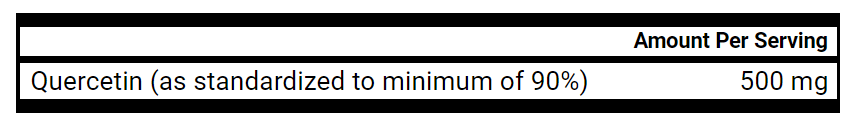
- Quercetin Ascorbate Powder
- S. Boulardii
- Medication
- Titration off Omeprazole over 2-3 weeks
- Other
- Meditate/Perform breathwork daily
- Follow-Up Plan
- 5-6 weeks
- Diet and Lifestyle
- Clinician Treatment Summary
- For treatment, I would like to begin utilizing 2 probiotics, a soil-based and beneficial yeast probiotic while also introducing immunoglobulins. I am choosing to do this earlier than gut repair nutrients and earlier than it is typical in our treatment sequence as I am suspecting it may have a more powerful anti-inflammatory effect on her GI tract. I will also have her incorporate 2 additional natural anti-histamine type supplements that include a combination of flavonoids that may help to decrease some of her hives. As we move forward with treatment, we will use her GI MAP testing and her response to the initial treatments to gauge whether or not to move more quickly to anti-microbial based treatments. Given her living situation, following a low histamine diet is not practical and thus was not recommended. I also shared that she could consider a titration off Omeprazole over 2-3 weeks (half her dose and then stop)
- Patient Self Assessment:
- Patient rates her health as a 75/100
- She states she is 10% better than when she started
- She feels she still experiences the hives daily, but that she has less extremely itchy episodes
- Reports she has a return of her menstrual cycle the month prior to our visit
- Denies any adverse reactions to treatments
- Has started all the supplements as previous recommended, feeling the probiotics have been some helpful to date
- Lab Results:
- GI MAP May 2021
- Elastase: 366
- Calprotectin: 34
- No overt pathogens
- No potential parasites
- Mild opportunistic dysbiosis
- GI MAP May 2021
- Lab Interpretation and Diagnosis:
- Her GI MAP did not reveal an overt or potential GI pathogen. The only major findings were some mild opportunistic dysbiosis.
- Post Infectious-IBS, History of GI Infections
- Gastritis (Tolerated titration off PPI without symptoms)
Hypochlorhydria – Iatrogenic(Off PPI now)- Female hormone imbalance – amenorrhea – (renormalizing cycle)
- Low normal, decreased oxygen-carrying capacity
- High allostatic load
GI pathogen(Negative Findings on GI MAP)- Histamine intolerant
- MCAS
- Clinical Decision Making:
- Catie has noted some mild improvements with less severe itching hives and has noted a return of her menstrual cycles which is encouraging. She has tolerated the supportive GI therapies well and titrated off the PPI without issue. The GI MAP did not show overt pathogens and only mild dysbiosis. We will move forward with more supportive treatments including digestive replacement and gut repair nutrients before moving on to herbal abx if deemed necessary.
- Treatment Hierarchy:
- Low Carb Paleo Diet (Current)
- Probiotics (SBO, S. Boulardii)
- MCAS Support
- Immunoglobulins
- Gut Healing Nutrients
- Digestive Support
- Anti-parasitics, Herbal Antimicrobials
- Adaptogens
- Elemental Formula
- Nutritional Replacement Therapy
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue with current lower carb Paleo diet
- Supplement
- Continue
- S. Boulardii
- Soil-based Probiotics
- PEA + Luteolin
- Quercetin Ascorbate Powder
- Stop Upon Completion
- Immunoglobulins
- Start
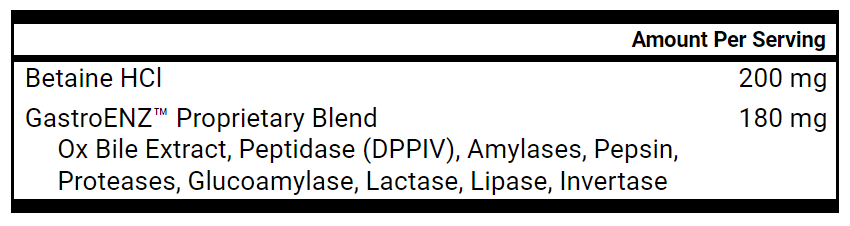
- Digestive Enzymes with HCl, 1-2 capsules with meals
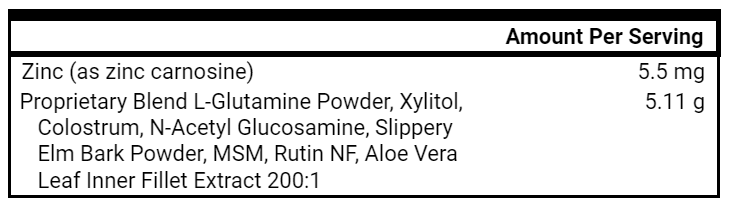
- Gut Healing Nutrients, 1 tsp, 2x daily
- Digestive Enzymes with HCl, 1-2 capsules with meals
- Continue
- Medication
- None
- Follow-up Plan
- 5-6 weeks
- Diet and Lifestyle
- Patient Self Assessment
- Feels 80-85/100
- Feels 10% better than last visit and 20% better since beginning work together and things are going well overall
- Reports despite even more stressful work period and less strict dietary intake, that she is not having constant itching and her hives are much milder overall
- Has continued with menstrual cycles, some mild PMS, but nothing like previous symptoms
- Has introduced the gut barrier supporting nutrients and enzymes without adverse event while continuing probiotics, quercetin and PEA + luteolin
- Reports no symptoms of GERD or gastritis
- Clinical Decision Making
- Catie feels that things are going really well. She has only had one bad flare-up with hives at the beginning of June during a period of significantly increased work stress. She is no longer constantly itching and has seen a return in her menstrual cycle that is starting to re-regulate.
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue with current lower carb Paleo diet
- Supplement
- Continue
- S. Boulardii
- Soil-based Probiotics
- PEA + Luteolin
- Quercetin Ascorbate Powder
- GI Healing Nutrients
- Digestive Enzymes with HCl
- Continue
- Follow-up Plan
- 8-12 weeks
- Diet and Lifestyle
Clinician’s Comments
Catie’s case is a great example of a simple stepwise approach through a supportive GI treatment hierarchy to treat chronic refractory extraintestinal symptoms. Research in the rapid review section highlights some of the connections between GI pathogens and chronic urticaria. While no evidence of a pathogen was found on her GI MAP, the extent of her symptoms warranted a stool test evaluation to help guide our treatment in that domain. I was pleased to see she was able to stop the PPI fairly quickly and did well with the addition of two MCAS supporting agents to her two histamine blocking medications. While we cannot 100% rule out a GI pathogen, even with a stool test, she has responded very nicely to supportive treatments and is unlikely to require antimicrobial treatments to maintain her symptomatic improvements
Clinical Rules Applied:
- Address underlying gut dysbiosis of pathogenic infections before digestive secretions
- Give time for healing before adding new treatments. Avoid “novelty bias” by continuing beneficial treatments in an iterative fashion for clinically appropriate periods of time before adding new treatments or significant treatment modification.
- Address underlying gut imbalances in cycling women prior to additional supplementation directed at female hormone support
Impact of the Swank and Wahls elimination dietary interventions on fatigue and quality of life in relapsing-remitting multiple sclerosis: The WAVES randomized parallel-arm clinical trial
https://journals.sagepub.com/doi/10.1177/20552173211035399
Study Purpose
- “To compare the effect of the modified Paleolithic elimination (Wahls) and low-saturated fat (Swank) diets in relapsing-remitting MS (RRMS)”
Intervention
- Parallel Clinical Interventions
- Randomized
- Individuals aged 18-70 followed either the low-saturated fat (Swank) diet or the modified Paleolithic elimination (Wahls) diet for a total of 24 weeks (this was following an initial 12 week run in period)
- Researchers sought to examine the effects of the dietary interventions on symptoms of fatigue, disease-specific mental and physical quality of life, and performance on a 6-minute walk test
- In addition to their respective dietary templates, participants followed a simplified supplementation regimen as follows
- 1 teaspoon cod liver oil
- 1,000 µg methyl-B12
- 1,000 µg methylfolate
- Multivitamin without iron
- 5,000 IU vitamin D3, the latter of which was adjusted based on serum levels with a target range of 40 to 80 ng/mL
Main Results
- 87 participants (44 Wahls) completed the initial run-in period
- 77 participants (39 Wahls) completed the initial 12 week study period and 72 total participants (35 Wahls) completed the full 24-week study
- Of the 72 total participants, adherence in both groups was fairly high (81.1% Swank, 74.3% Wahls)
- Both groups noted significant reductions in fatigue with the Wahls group noting an even greater reduction
- “Significant mean reductions from baseline were observed in the primary outcome of Fatigue Severity Scale (FSS) at both 12 and 24 weeks”
- The Wahls group experienced a 24-week Modified Fatigue Impact Scale (MFIS) mean reduction that was significantly greater than the Swank group (p = 0.02).
- The Wahls group noted an increased distance walked on the 6-meter walk test by 24 weeks which was not observed in the Swank group
- Neither group experienced significant improvements in distance walked during the 6-minute walk test (6MWT) at 12 weeks (Table 2). The 12-week mean differences were 3.7 ± 5.5 meters for the Swank group (p = 0.50) and 9.3 ± 7.8 meters for the Wahls group (p = 0.23). By 24 weeks, the mean difference from baseline for the Swank group did not change (10.0 ± 6.7 meters; p = 0.13), whereas the Wahls group walked 36.6 ± 13.5 meters further compared to baseline distance (p = 0.007) and achieved clinical significance defined as 6% change”
Authors Conclusion
- “The observation that both dietary approaches in this study are associated with significant reductions in fatigue and improvements in QoL greatly benefits the MS community in that it allows for patient preference for either diet and suggests that the benefits of dietary approaches are due to underlying mechanisms rather than unique characteristics of specific diets”
Interesting Notes
- While participants in both dietary arms appeared to have benefited from improved fatigue and quality of life, the slight edge objectively appears to favor the Paleo based Wahls diet over the plant based low-saturated fat Swank diet
Clinical Takeaways:
- Individuals with RRMS are likely to benefit from the adoption of a nutrient-dense way of eating such as the Swank or Wahls diet and can achieve this benefit from initial dietary counseling followed by less robust support to maintain adherence to the respective way of eating.
Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials
https://pubmed.ncbi.nlm.nih.gov/31004628/
Study Purpose
- To evaluate for the clinical effectiveness of prebiotics/probiotics for depression and anxiety
Intervention
- 34 human interventional studies that included 7 prebiotic and 29 probiotic studies were included in the final meta-analysis.
- Length of prebiotic administration across trials ranged from four hours to four weeks.
- Duration of probiotic administration across trials ranged from eight days to 45 weeks.
- The researchers included primarily non-clinical populations or studies – essentially studies that were not treating depressed or anxious populations, but “healthy populations” or those without these diagnosed medical conditions (important point to note).
Main Results
- There is insufficient data in clinical populations to comment strongly on the effects of probiotics to treat depression or anxiety
- “We did find general support, however, for an effect of probiotics on depression and anxiety, with small pooled effects in both cases. Although Lactobacillus received the most interest among probiotic trials, when considered alone, it did not have an effect on depression, with a significant difference in effect size existing between Lactobacillus-only trials and others.”
- “First, and perhaps most important, is the dearth of trials featuring samples with clinical depression and anxiety. Indeed, only four trials included samples with major depression.”
- The majority of studies were underpowered to detect significant effects, the median sample size of included studies being 46.5.
- The effect of the length of pre/probiotic administration was not analyzed.
- We should not rule out the therapeutic potential of probiotic level interventions for psychological disorders, but we should likely be more cautious in our suggestions of strong evidence supporting this therapy.
Authors Conclusion:
- “In summary, the current evidence base for prebiotics and probiotics in the treatment of internalizing disorders appears modest. Support for the efficacy of probiotics for depression and anxiety was observed, but with generally small pooled effects. These findings are qualified, however, by the relative rarity of trials with psychiatric samples and the prevalence of non-clinical samples in the literature, which together significantly reduced the observed effects.”
Interesting Notes:
- There were no pediatric or adolescent trials available for inclusion in the meta-analysis
Clinical Takeaways:
- While Lactobacillus based interventions appear to be the primary treatments utilized in the pooled analysis, one should likely consider a broader range of probiotic species/strains given the minimal adverse effects expected.
Clinician’s Comments
- Rather than use this meta-analysis as evidence against the use of Lactobacillus based probiotics for psychological symptoms such as depression, I feel it simply highlights the research gap for probiotics in clinically, psychologically suffering populations with the caveat that studies isolated to one intervention (such as probiotics) for complex conditions such as depression are unlikely to find remarkably large effect sizes given the complex and multifaceted nature of depressive illness.
Chronic spontaneous urticaria and internal parasites: A systematic review
https://pubmed.ncbi.nlm.nih.gov/26648083/
- 39 studies included in the SR
- Individuals with chronic spontaneous urticaria showed more frequency seropositive for several protozoan parasite including Blastocystis hominis
- Anti-parasitic medications were >50% efficacious in 9/21 studies examining treatment
- The authors propose various mechanism for the urticaria and gut connection
- “Pathogenic mechanisms in chronic spontaneous urticaria due to parasite infection may include specific IgE, Th2 cytokine skewing, eosinophils, activation of the complement, and the coagulation systems.”
Effects of Quercetin on Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
https://pubmed.ncbi.nlm.nih.gov/27405810/
- 7 trials with 9 treatment arms with ~600 patients
- Significant effects were noted with doses of at least 500 mg daily
- “The results of the meta-analysis showed significant reductions both in systolic BP (WMD: -3.04 mm Hg, 95% CI: -5.75, -0.33, P=0.028) and diastolic BP (WMD: -2.63 mm Hg, 95% CI: -3.26, -2.01, P<0.001) following supplementation with quercetin.”
- While these effects are not clinically astonishing, quercetin has a reasonable tolerance profile with many other potential benefits that make it an exciting nutraceutical for clinical practice.
The role of probiotic bacteria in managing periodontal disease: A systematic review
https://pubmed.ncbi.nlm.nih.gov/27224284/
- 12 RCT’s included
- Lactobacillus based probiotics appear to show benefit from address periodontitis
- “Analysis of 12 RCTs revealed that in general, oral administration of probiotics improved the recognized clinical signs of chronic and aggressive periodontitis such as probing pocket depth, bleeding on probing, and attachment loss, with a concomitant reduction in the levels of major periodontal pathogens.”
- To achieve full benefits, therapy may need to be continuous rather than temporary
Visit Time Management
Let’s face it, we as clinicians are always trying to be as time efficient and respectful to our patients as possible. We have multiple, sometimes competing interests during a patient encounter. While we desire for each patient to leave their therapeutic encounter feeling heard with an actionable and personalized plan, we also want to ensure we stay on time in an effort to treat subsequent patients with the same respect and fairness. While some providers may choose to provide themselves with significant margins between patient visits in order to minimize the likelihood of time stress, most operate with tighter margins out of financial necessity. Because of this, here are a few basic tips to help you with optimal time management during your visits.
1. State the goalposts at the beginning of the visit
As you may be running behind to start your patient visit, it is best to start with no hidden expectations of when the visit may end. I find it quite helpful in the beginning to state something like this,
“I appreciate your patience and am looking forward to talking with you today. We have until 10:30 AM for our session today and know there is a lot to cover. Would you like to tell me how things have been going since our last visit?”
2. Provide an update as the time is coming to a close
It can be really helpful to offer the patient an idea of where the visit has progressed in order to set up the closing. Depending on the length of your visits and the patient itself, you may opt for a 5 or 10 minute “warning”.
“I just wanted to let you know we will be wrapping up in about 5 minutes. Were there any particularly pressing concerns or questions you wanted to ask me? If not, I can provide us with a summary of today’s visit and the direction for our treatment. How does that sound?”’
3. Close and redirect to additional team services or the patient’s next visit
As you are visiting with patients, try to assess what needs they may have for additional support staff. While you can only offer them services or additional support that your clinic actually possesses, it is often a good idea at the end of visits to redirect them to the ways in which they can communicate questions with your support team or suggest the ways in which they can make visits with health coaches or nutritionists. You want to help minimize the likelihood for future lost time or bad outcomes from patients that do not feel they have the support they need. A little redirection/reminder can go a long way!