TREATING CLINICIAN: ROB ABBOTT, M.D.
Patient Summary:
- Sarah is a 68-year-old normal weight female with a kind and gentle attitude lost in the weeds of functional medicine who primarily complains of fatigue, insomnia, gastritis, and mixed IBS.
- She is currently utilizing a strange combination of thyroid replacement medications amidst other hormone replacement therapy.
- Chief Complaints:
- Fatigue – Severe
- Insomnia – Severe
- Multiple GI complaints – Frequent and Severe
- Diarrhea, constipation, abdominal pain, gas, painful defecation
- Excessive mucus, Paroxysmal nocturnal dyspnea, and cough – Frequent and Severe
- Brain Fog – Frequent, Not Severe
- Prior Diagnosis:
- Hypothyroidism, 2002
- Depression, 2018
- Collagenous Colitis, 2019
- Medications:
- Estradiol (pellets)
- Testosterone (pellets)
- Armour 45 mg AM AND 45 mg early afternoon
- Liothyronine 5 mcg AM AND 5 mcg early afternoon
- Naltrexone 4.5 mg
- Bupropion 300 mg
- Budesonide – nasal nebulizer, as needed
- Prior Surgical History:
- No previous abdominal surgeries
- Prior Testing Summary:
- Colonoscopy 2019
- Identified collagenous colitis
- Endoscopy 2019
- Identified mild gastritis, negative H. pylori
- October 2019 Blood Chemistry
- NEGATIVE anti-thyroglobulin antibodies
- May 2021 Blood Chemistry
- TSH: 0.086
- Free T3: 5.2
- DHEA: 154
- TPO <1
- hs-CRP: 9.3
- ANA: 1:
- June 2021 Blood Chemistry
- Testosterone: 142
- Estradiol: 50
- ANA, speckled pattern
- Sodium: 131
- Total Cholesterol: 210
- Colonoscopy 2019
- Treatment History Summary:
- Helpful Diets
- Gluten Free, Dairy Free, Low Carb Paleo
- Reactive Foods
- Caffeine and/or coffee
- Helpful Supplements
- Probiotics
- Digestive repair nutrients (glutamine, aloe, etc..)
- Hydrochloric acid (betaine HCl)
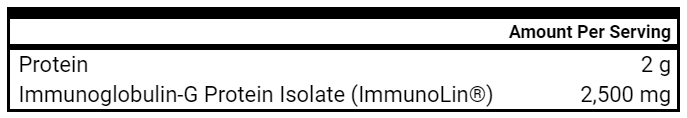
- Immunoglobulins
- Fiber PREbiotics
- Magnesium
- Concerning Treatments
- Inappropriate Hormone Replacement Therapy
- Markedly elevated testosterone
- Inappropriate Thyroid Hormone Replacement
- Multiple times daily dosing
- Markedly suppressed TSH and elevated Free T3
- Inappropriate Hormone Replacement Therapy
- Helpful Diets
- Onset:
- 2002
- Saw Functional MD who diagnosed with hypothyroidism and provided medication
- Recalls that this didn’t seem like something she needed
- 2019
- Diagnosed with collagenous colitis in setting of mixed IBS symptomatology
- Also noted with elevated ANA and CRP
- Reports utilizing many dietary patterns with some benefit, but continues with abnormal GI function and no changes in her CRP.
- Present
- Continues to utilize multiple different regimens of thyroid hormone replacement
- Reports confusion on what she needs and what is actually helpful
- Continues to use hormone replacement therapy that was started around age 40
- Feels this has helped her libido, sexual health
- Reports some allergic type symptoms in Austin
- Paroxysmal nocturnal dyspnea, nasal congestion, mild coughing
- Utilizing steroid nebulizer with some benefit
- Continues to utilize multiple different regimens of thyroid hormone replacement
- 2002
- Clinical Questions/Comments:
- Is the patient’s hypothyroidism diagnosis correct?
- Does she actually require thyroid replacement medication?
- Are some of her medications, most notably the hormone replacement and thyroid medication causing some of her symptoms including insomnia and fatigue?
- How can I best use testing to alleviate some of the patient’s anxiety and steer treatment in a more appropriate direction?
- How can I build a therapeutic alliance to keep the patient from working with other providers recommending inappropriate therapies?
- Prognosis:
- This is somewhat challenging to discern given her scattered care with other misleading providers, but I expect she will improve with thyroid hormone titration/discontinuation and a refocusing on GI therapies.
- Differential Dx:
- Dietary & Lifestyle
- Personality – slight neuroticism
- Affective Disorder – depression, not active
- Gastrointestinal
- Collagenous Colitis, IBD (Elevated Calprotectin)
- SIBO
- Dysbiosis
- Gastritis
- Gut Pathogen
- Digestive Insufficiency
- Hormonal
- Female hormone imbalance – on excessive/inappropriate HRT
- Incorrect thyroid dx and/or unnecessary thyroid medication
- Nutritional
- Nutritional Deficiencies (tba)
- Autoimmune Phenomena
- Positive ANA, elevated hs-CRP
- Other/2nd level
- Oral health Imbalance – root canals
- Heavy metal toxicity, historical mercury amalgams
- Sleep disordered breathing
- MCAS
- Mold exposure/illness
- Metabolic
- Dyslipidemia
- Underlying CVD?
- Dietary & Lifestyle
- Recommended Testing:
- Exagen AVISE-CTD – Autoimmune Profile (Serum)
- GI MAP
- Blood Chemistry
- CBC with Differential, CMP
- Lipid Panel, apoB, Fasting Insulin, a1c
- TSH, Free T4, Free T3 (after stopping Liothyronine)
- Zinc, Copper, Magnesium, Homocysteine, Iron Profile, Folate, B12, Vitamin D
- Cardiac CT for Calcium Scoring
- Clinical Decision Making:
- I desire to be more comprehensive in my initial testing to ask several important clinical questions and questions of the patient.
- She is quite concerned about her elevated ANA and hs-CRP that have not been explained and she feels she may have heart disease and is concerned about her cholesterol.
- She is a good candidate for serum testing with an autoimmune profile called AVIST-CTD through a company called Exagen as well as Cardiac CT with Calcium scoring to assess for coronary artery calcification.
- I feel that stool testing with a GI MAP can provide some helpful information about the active state of inflammation of her GI tract and the degree of dysbiosis or pathogenic infections that could change treatment.
- For blood chemistry, given my concerns for nutritional deficiencies from possible maldigestion/malabsorption, her previous thyroid hormone testing and our overall concerns for cardiovascular disease, I would like to better understand the current state of her metabolic health, her thyroid function with the cessation of T3 medication and her overall nutritional status.
- Treatment Hierarchy:
- Paleo Template
- Partial Elemental Diet
- Triple Probiotics – Higher Dose
- Gut Healing Nutrients
- Cessation of T3
- Intranasal Xylitol Rinses
- Decrease testosterone pellets (outside provider)
- Nutritional Replacement Therapy
- Immunoglobulins
- Adaptogens
- Anti-inflammatory phytonutrients vs. MCAS Supports
- Digestive Enzymes, HCl
- Herbal Antimicrobials
- Initial Treatment Recommendations:
- Diet and Lifestyle
- Paleo Template
- Partial Elemental Diet – 1 meal Daily
- Supplements
- Triple Probiotic Packs, 1 pack, 2x daily
- Gut Healing Nutrients
- Triple Probiotic Packs, 1 pack, 2x daily
- Medication
- Stop Liothyronine
- Other
- Consult outside provider to decrease/stop testosterone pellets
- Follow-up Plan
- Obtain labs 4 weeks after stopping Liothyronine
- Visit in 6-7 weeks
- Diet and Lifestyle
- Clinician Treatment Summary:
- Sarah has used HRT and NDT extensively since 2002. I feel her hypothyroidism diagnosis is inappropriate and she is using unnecessary medication. She is also being misled into excessive HRT without addressing underlying gut imbalances and perhaps some underlying autoimmune – connective tissue concerns. My initial focus will be to obtain baseline testing to better assess her GI health and overall metabolic/immune functioning. My treatment will focus on supportive GI elements while I encourage her to begin titrating down her current thyroid medication and decreasing HRT.
- Patient Self Assessment:
- Rates health at 75/100
- Reports overall 50-60% improvement since our first visit
- Reports sleep 50% better, her GI symptoms are 60% better
- Improved
- Fatigue
- Diarrhea, abdominal pain
- Insomnia, Night time awakening
- Mucus, PND, cough – with 2 week course of Prilosec, symptoms improved
- Worse
- None
- Reports that she is now only taking 90 mg Armour in the AM
- She has much less diarrhea and minimal abdominal pain with more normal bowel pattern
- She as implemented the semi elemental diet, probiotics at a higher dose (2 packets daily) and gut healing nutrients
- She denies any adverse reactions to the supplement
- Lab Results:
- GI MAP (08/31/21)
- Moderate Dysbiosis
- No pathogens
- No parasites
- Elastase: 761
- Calprotectin: 219
- AVISE-CTD (September 2021)
- 1:160, ANA
- Negative TPO/TGA
- + Anti-cardiolipin IgG
- Blood Chemistry (10/04/21)
- Ferritin: 138
- WBC: 6.8, Monocytes: 11%
- K+: 5.3
- TC: 217, LDL-C: 139
- apoB: 109
- Insulin: 5, a1c: 5.3
- TSH: 0.407, Free T3: 6.2
- Free T4: 1.13
- Zinc: 85
- Cu: 136
- Mg: 2.2
- Homocysteine: 16.2
- Vit D: 35.1
- B12: 818
- Folate: 4.5
- Cardiac CT with Calcium Scoring
- 0 Agatston units
- Mild bibasilar bronchiectasis
- GI MAP (08/31/21)
- Lab Interpretation and Diagnosis:
- Sarah’s Cardiac CT with calcium scoring was 0 which was greatly encouraging and helped her to be less concerning about some of her lab markers.
- Her blood chemistry showed continued suppressed TSH even without the previous 10 mcg of Liothyronine, increasing the likelihood of inappropriate hypothyroidism diagnosis.
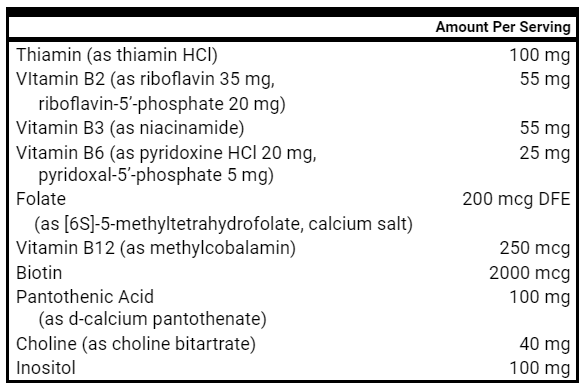
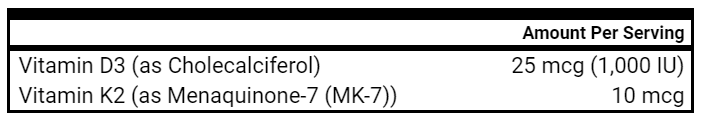
- Nutritionally she appears with a significant folate deficiency and possible B6 deficiency with elevated homocysteine. Her Vitamin D could likely be higher.
- Her AVISE-CTD corroborated her previous ANA and negative thyroid antibody testing without other concerning findings.
- Her stool testing revealed moderate dysbiosis without a pathogen and a calprotectin of 219 which is consistent with her moderately active collagenous colitis.
- Updated Differential Dx:
- Dietary & Lifestyle
- Personality – slight neuroticism
- Affective Disorder – depression, not active
- Gastrointestinal
- Collagenous Colitis, IBD (Elevated Calprotectin)
- SIBO
- Dysbiosis (Moderate on GI MAP)
- Gastritis – previous endoscopy and PPI response
Gut Pathogen(Negative on GI MAP)- Digestive Insufficiency – Possible HC given PPI response
- Hormonal
- Female hormone imbalance – on excessive/inappropriate HRT
- Incorrect thyroid dx and/or unnecessary thyroid medication
- Nutritional
- Nutritional Deficiencies (tba)
- Folate
- Nutritional Deficiencies (tba)
- Autoimmune Phenomena
- Positive ANA, elevated hs-CRP
- Other/2nd level
- Oral health Imbalance – root canals
- Heavy metal toxicity, historical mercury amalgams
- Sleep disordered breathing
- MCAS
- Mold exposure/illness
- Metabolic
- Dyslipidemia – (apoB: 109)
Underlying CVD? (Negative CAC)
- Dietary & Lifestyle
- Clinical Decision Making:
- Sarah has responded well to our initial thyroid down titration and supportive GI treatments.
- Given the suppressed TSH and elevated Free T3, we discussed continuing to decrease her Armour to 60 mg.
- While her stool testing revealed moderate dysbiosis and inflammation, I was encouraged by her initial response to the GI treatments, so I suggested continuing supportive GI treatments with options for an immunoglobulins trial.
- Her mucus and cough could indeed be coming from the GI tract given her response to the PPI, however, we will seek to avoid this medication and see if symptoms respond to continued GI supports.
- Her insomnia and fatigue have likely improved given the decrease in unnecessary thyroid medication and improving GI health.
- Updated Treatment Hierarchy:
- Paleo Template
- Partial Elemental Diet
- Triple Probiotics – Higher Dose
- Gut Healing Nutrients
- Cessation of T3/Decrease Armour
- Intranasal Xylitol Rinses
- Decrease testosterone pellets (outside provider)
- Nutritional Replacement Therapy
- Immunoglobulins
- Adaptogens
- Anti-inflammatory phytonutrients vs. MCAS Supports
- Digestive Enzymes, HCl
- Herbal Antimicrobials
- Updated Treatment Recommendations
- Diet and Lifestyle
- Continue Paleo Template
- Continue Partial Elemental Diet – 1 meal Daily
- Supplements
- Continue Triple Probiotic Packs, 1 pack, 2x daily
- Continue Gut Healing Nutrients
- Start Immunoglobulins, 2 scoops daily
- Start B Complex, 1 pill daily
- Start Vit D/K2, 4 drops daily
- Medication
- Start Armour 60 mg
- Follow-up Plan
- Obtain TSH, Free T4, Free T3 and CMP 4 weeks after starting Armour 60 mg
- Visit in 6 weeks
- Diet and Lifestyle
Clinical Rules Applied and Final Clinician Comments
- Functional Medicine is foundationally a diet and lifestyle based approach and should leverage and prioritize such low risk interventions initially and throughout treatment.
- Exhaust low risk, empirically informed treatments prior to the consideration of testing to guide/modify treatment recommendations.
- Give time for healing before adding new treatments. Avoid “novelty bias” by continuing beneficial treatments in an iterative fashion for clinically appropriate periods of time before adding new treatments or significant treatment modification.
- Appropriately apply the thyroid treatment algorithm to patients who may be inappropriately diagnosed and can benefit from discontinuation or decreased medication.
In this case, we see yet again an excessively and inappropriately treated patient in functional medicine primarily through the indiscriminate use of hormone replacement therapy as well as a complicated and likely unnecessary thyroid treatment regimen. The patient received significant benefit through the iterative application of low-risk, empirically-formulated dietary, lifestyle, and GI directed treatments. For this patient, I performed a greater degree of clinically-informed testing initially that was utilized primarily for diagnostic purposes and supporting the patient’s anxiety/increasing treatment adherence rather than providing concrete direction for treatment. While the patient’s GI MAP testing came back with concerns that could be possibly treated with antimicrobial regimens, I chose to continue the supportive regimens that were providing benefit. The negative CAC scan provided some reassurance around her concerns for cardiovascular disease and calcification. The AVISE-CTD autoimmune profile also provided reassurance of no other specific connective autoimmune phenomenon and again confirmed the negative thyroid auto-antibodies, increasing the likelihood of successful thyroid medication discontinuation. The blood chemistry testing provided valuable insights regarding the effect of decreased, excessive thyroid medication use and highlighted general nutrient sufficiency with the exception of a likely clinically-relevant folate deficiency. The blood chemistry testing also suggested that the patient was generally metabolically healthy with a reasonable apoB. As a field, we must continue to highlight inappropriate care, moving to reformed, evidence-informed practices, and document how patients can actually receive safe and effective care.
Effect of synbiotics and probiotics supplementation on autoimmune diseases: A systematic review and meta-analysis of clinical trials
https://pubmed.ncbi.nlm.nih.gov/33642142/
Study Purpose
- To examine the effects of probiotics or combination prebiotics/probiotics (synbiotics) as positively modulating agents in autoimmune disease
Intervention:
- Meta-analysis of 10 randomized controlled trials
- 440 subjects (N= 216 intervention)
- Modulation of three domains
- Blood sugar control (HOMA-IR)
- Inflammation (hs-CRP, ESR, IL-6, IL-10, TNF-ɑ)
- Oxidative Stress (Glutathione, Malondialdehyde, Total Antioxidant capacity)
Main Results:
- Most studies are international – many out of Iran
- 7/10 studies involving Rheumatoid Arthritis
- 2/10 studies involving Relapsing Remitting Multiple Sclerosis
- 1 study on Systemic Lupus Erythematosus
- Age from 16-61 years old, female predominance, mostly overweight, but non-obese
- Disease duration from 3.2 – 16.3 years (not early onset)
- Most studies used probiotics only (instead of synbiotics)
- “Lactobacillus casei [ 13 , 22 ], Lactobacillus reuteri [ 17 ], Lactobacillus rhamnosus [ 27 ] and more than one type of probiotics”
- “Daily dose of probiotics ranged from 10 8 to 112.5 × 10 9 CFU.”
- Inflammatory Markers
- hs-CRP – clinically and statistically significant decrease in most patients – the most pronounced effects were in younger patients, with shorter disease duration using lacto/bifido combination probiotics
- “Furthermore, in patients with disease duration ≤6 years, the impacts of synbiotics and probiotics on hs-CRP reduction was greater (SMD = −0.67, P < 0.001 ) than those with >6 years (SMD = −0.45, P < 0.019 ).”
- “The largest decrease in hs-CRP levels was observed in patients who received Lactobacillus plus Bifidobacterium strains (SMD = −0.71; 95% CI = −0.96, −0.45, P < 0.001 ).”
- IL-6 – clinically and statistically significant decrease – most pronounced in studies lasting > 3 months duration
- “Studies that administered synbiotics and probiotics for more than 12 weeks could make a significant reduction in serum IL-6 concentrations (WMD = −0.28 pg/ml; 95% CI = −0.55, −0.01, P = 0.042 ).”
- hs-CRP – clinically and statistically significant decrease in most patients – the most pronounced effects were in younger patients, with shorter disease duration using lacto/bifido combination probiotics
- Oxidative Stress
- There were minimal to no effects of synbiotics or probiotics on any of the three oxidative stress markers including glutathione and total antioxidant capacity.
- “Overall, no significant correlation was observed between probiotic treatment and GSH”
- There were minimal to no effects of synbiotics or probiotics on any of the three oxidative stress markers including glutathione and total antioxidant capacity.
- Blood Sugar Control
- HOMA-IR – clinically and statistically significant decrease in patients. A mean difference (WMD) of 0.71 is quite clinically meaningful and arguably the most clinically relevant finding outside of hs-CRP decrease in this entire meta-analysis
- “a significant reduction in HOMA-IR was seen following supplementation (WMD = −0.71; 95% CI = −1.05, −0.37, P <0.001 )”
- HOMA-IR – clinically and statistically significant decrease in patients. A mean difference (WMD) of 0.71 is quite clinically meaningful and arguably the most clinically relevant finding outside of hs-CRP decrease in this entire meta-analysis
Authors Conclusion:
- “Our findings revealed that synbiotics and probiotics supplementation has significant effect on some inflammatory and oxidative stress markers; although, the number of trials was too small to make powerful conclusions and further investigations may be needed.”
- “Synbiotics and probiotics seem to be less effective in changing serum levels of oxidative stress markers e.g. TAC, GSH.”
Clinical Takeaways:
- Probiotics or synbiotics may provide some benefit to patients with autoimmune disease (RA the main disease studied) by improving blood sugar control and decreasing inflammation.
Clinician’s Comments
- While this meta-analysis was quite small and we must be quite hesitant to make any wide ranging conclusions, it does provide further support for gut directed interventions for those with autoimmune disease even if overt GI symptoms are not present.
- Given the low risk of lacto/bifido probiotics, such treatments should be considered in the treatment of patients with autoimmune disease with or without overt GI symptoms.
Igg Food Antibody Guided Elimination-Rotation Diet Was More Effective than FODMAP Diet and Control Diet in the Treatment of Women with Mixed IBS—Results from an Open Label Study
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8509634/
Study Purpose
- To investigate the effectiveness of a personalized IgG antibody based dietary intervention to a standardized low FODMAP dietary intervention for women with mixed IBS
Intervention:
- OPEN LABEL study for 3 dietary interventions taking place over 8 weeks
- Low FODMAP
- IgG antibody elimination diet
- Control – Dietary advice from their attending GI physician
- 90 Participants – 30 allocated (not randomized) to each group
- Symptoms assessed via YES and NO answers – no standardized questionnaire or visual analog scale
- Key Point
- The participants KNEW precisely what advice or care they were getting. The low FODMAP diet folks knew they were getting likely helpful, but generic advice. The IgG folks knew they were getting “very personalized” dietary advice while the control group received recommendations from a GI specialist for a diet consisting of easily digestible elements that could be modified based on their stool consistency or pattern.
- Red Flags
- Open Label
- Yes or No answers to study questions
- Variable/no standard control
- Patients were allowed to vary their diet to some degree throughout the study based on symptoms they were experiencing
Main Results:
- Baseline Demographics and Completion Rates
- A per protocol analysis was performed (only people completing the study included in the final data analysis)
- 26/30 patients in control and low fodmap finished the study
- Only 21/30 patients in IgG group finished
- Borderline overweight women ~ 40 years of age (premenopausal)
- Majority of patients with IBS-M <5 years
- Intervention Results
- The Control group saw ZERO change in ANY marker – not even a whiff of a placebo effect
- The Low FODMAP group saw significant changes in bloating, gurgling sensations, gastric fullness, nausea, mucus and blood in the stool. There were trends for decreasing abdominal pain, however, complaints of incomplete defecation and constipation were unchanged.
- The IgG antibody elimination group appears to have found the grand elixir of life with near symptom evaporation in all domains.
Authors Conclusion:
- “This study shows that a personalized dietary approach is more effective in treating IBS-M than generalized diet recommendations.”
- “Only the IgG elimination-rotation diet could demonstrate significant improvements in all of the monitored IBS-M symptoms as well as extra-intestinal symptoms.”
- “Claims that IgG food antibodies only reveal exposure to food and not intolerance should be reinvestigated in larger double-blinded studies.”
Interesting Notes:
- Okay – before I throw this study in the dumpster, let me at least provide some helpful criticisms.
- Reiterating again – the IgG group got personalized care and KNEW it. They essentially got the combination of a well formulated elimination diet that removed some of the most commonly immunogenic food including gluten, grains, dairy, soy and nuts, the effect of caregivers and any further placebo enhancements from the personalized care.
- A control group having zero effect as a placebo is a big red flag for a IBS study – again likely because the participants knew they were getting suboptimal advice from a doctor and not getting extra attention. Something of a nocebo is likely happening here.
- The researchers used a silly YES and NO score for symptoms. How did each participant decide Yes or No? Was it one day? They had to be internally gauging some degree of severity and frequency. It is not like things just magically evaporated. Trying to simplify something to a dichotomous variable that should be continuous (on a spectrum) may simplify things for researchers, but it’s BAD data collection for symptoms experienced on a spectrum over time.
- 5 more participants dropped out of the IgG study as compared to either the control or low fodmap groups. A 66% completion rate for a supported dietary study isn’t great. Given the small size of the intervention, if all those folks did not get better (a reasonable assumption) the IgG intervention would suddenly not look so magical.
- There was no randomization, simply standardized allocation – every 3rd person in a certain group.
- The researchers DID NOT perform UNPAIRED statistical analysis – despite having 3 groups, they only performed PAIRED or WITHIN group analysis instead of UNPAIRED or BETWEEN group analysis. The best way to make an intervention look better than it is, is to not compare it to another intervention that showed some improvement.
Clinical Takeaways:
- A Low FODMAP diet (as supported by larger meta-analysis) appears helpful in alleviating GI symptoms in middle aged women with IBS-M
- IgG based elimination diets must be studied in a rigorous manner to determine their potential usefulness in clinical practice.
- Don’t get nutritional advice from a GI doctor
A Low-FODMAP Diet Improves the Global Symptoms and Bowel Habits of Adult IBS Patients: A Systematic Review and Meta-Analysis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8417072/
- 10 studies involving 511 participants
- All were randomized controlled trials with at least single blinding
- Some compared Low FODMAP to a standard or habitual diet while others compared to sham or even high FODMAP diet (heterogeneity in control diet)
- Improvement in stool consistency and reduction in stool frequency
- IBS-QOL and other measures of psychological/mental health minimally affected
- “There was no statistically significant change in IBS-QOL (n = 484; MD = 2.77; 95% CI −2 to 7.55; I2 = 62%), anxiety score (n = 150; MD = −0.45; 95% CI −3.38 to 2.49; I2 = 86%), depression score (n = 150; MD = −0.05; 95% CI −2.5 to 2.4; I2 = 88%)”
- Potentially greater benefits for IBS-D versus other subtypes
- “A ‘Low FODMAP diet’ is effective in reducing the global symptoms and improving the bowel habits of adult IBS patients. The efficacy for IBS-D patients can also be more pronounced.”
- Take Home:
- A moderately sized meta-analysis of randomized controlled trials with “moderate” overall quality of the data according to GRADE criteria comparing a low FODMAP diet to various control diets suggested benefit for improving stool consistency and frequency with signals for improved overall IBS symptoms with the most pronounced effects occurring in the group with IBS-D.
Excretion of Heavy Metals and Glyphosate in Urine and Hair Before and After Long-Term Fasting in Humans
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8505741/
- Aim
- To study the effects of an extended period of fasting (10 days) on the excretion of various heavy metals and glyphosate.
- 109 healthy subjects between age 18-70 (Avg: 56.7) (Women: 68)
- Urinary Assessments: As, Cr, Co, Pb, Ni, Hg and glyphosate
- Hair Assessments (22 subjects): Similar parameters were assessed
- Self Assessment – Symptoms – Before fasting, daily during 10 day fast, 4 weeks after fast
- Fasting Regimen
- 20 g honey
- 250 mL vegetable broth
- 250 mL organic juice
- Additional H20 or non-caloric, organic herbal teas
- Results
- Arsenic (As) found in ALL subjects at baseline
- 71.5% decrease in As AFTER the fasting period
- Nickel (Ni) found in 50 or ~50% of subjects at baseline
- Ni found (above detection limit) in only 28 subject AFTER the fasting period
- Mercury (Hg) found in 40/109 patients at baseline
- Hg found in 29 subjects AFTER the fasting period (not statistically significant)
- Glyphosate found in only 9 patients BEFORE and in 0/9 AFTER
- Self reported benefits included decreased fatigue, sleep disorders, headache and hunger
Diagnostic yield of endoscopy in irritable bowel syndrome: A nationwide prevalence study 1987-2016
https://pubmed.ncbi.nlm.nih.gov/34420846/
- Aim
- To determine the clinical utility of endoscopy and colonoscopy in patients with IBS
- Clinical Concern
- Are endoscopy and colonoscopy overused in IBS patients?
- Is there excessive risk in undergoing the procedure because of a low pre-test/procedure probability of finding something of pathological significance?
- Summary of Clinical Concern
- Do the benefits of performing colonoscopy and endoscopy in patients with IBS outweigh the risks (direct and indirect damage from the procedure, misdiagnosis, and overdiagnosis)
- Location – Sweden
- Participants – ~22,000 IBS, ~81,000 controls
- Results
- IBS patients had a clinically and statistically significant decreased risk for IBD, colon cancer, precancerous polyps and celiac disease
- “Biopsy-proven IBD was seen in 1.6% of IBS and in 5.9% of controls”
- “The prevalence of precancerous polyps was 4.1% vs. 13.0%”
- “The prevalence of colorectal cancer 0.8% vs. 6.3%”
- “The prevalence celiac disease 1.9% vs. 3.4%”
- “The prevalence of microscopic colitis was 2.9% vs. 1.7%”
- IBS patients had a clinically and statistically significant decreased risk for IBD, colon cancer, precancerous polyps and celiac disease
- Conclusions
- “The diagnostic yield of upper endoscopy and colonoscopy for organic disease is low in patients with a first-time diagnosis of IBS, though increases with age.”
- Clinician Thoughts
- I suspect the lower rates of the examined conditions stems from the appropriate diagnostic evaluations for such conditions prior to the diagnosis of IBS. Such evaluations could include serum testing of celiac antibodies, stool testing for occult blood, calprotectin or other inflammatory mediators and risk stratification based on age, family history and other aspects of the person’s medical history.
- With a thorough work-up using non-invasive diagnostics, it appears that individuals can be appropriately classified as having IBS with low risks for other organic GI conditions. Taken a step beyond, functional medicine practitioners can utilize GI directed therapies to help improve symptoms in patients with IBS, decrease the utilization of low yield invasive diagnostics like endoscopy and colonoscopy, and provide reassurance to the patient (based on this research) regarding the low prevalence of other more concerning GI conditions when an appropriate diagnosis of IBS is given.
The Better Nutrition Program
At the Ruscio Institute for Functional Medicine (RIFM), dietary guidance is a foundation for every set of therapeutic recommendations. From low FODMAP and low histamine diets to the utilization of Elemental Heal in combination with a paleo diet, we recognize the importance and power of personalized nutrition. Many of our patients come in extremely confused about what to eat and how they can use nutrition to help alleviate GI and non-GI symptoms. While they recognize we are not strictly nutritional professionals, they desire to be provided evidence informed nutritional recommendations that will help alleviate their symptoms. It can be challenging as functional medicine providers to feel competent in providing patients with supportive and personalized nutrition recommendations. It is much easier to simply order labs, recommend supplements and prescribe medications and never give the essential nutritional guidance and support they need.
Don’t be one of those practitioners.
There are numerous programs geared at training and supporting professionals engaged in nutritional and lifestyle medicine and it can certainly be overwhelming to choose a training/program to advance your practice and clinical skills.
At RIFM we have been quite impressed with The Better Nutrition Program (BNP) that offers comprehensive tools for personalizing nutrition including cutting-edge evaluations that help you get all patient data – food, supplement, medications, health and lifestyle information that are beautiful & easy to fill out. The BNP Toolkit™ also includes guides, protocols and menus, as well as business and marketing tools to help ensure you operate a financially viable and vibrant business. They offer 2 tiers of engagement for those desiring even more community and support from their BNP community of practitioners.
If you feel like you are falling into the trap of relying too heavily on labs, supplements and medications, you should strongly consider investing in a program or toolkit like BNP that will give you actionable documents and education to provide your patients with informed and personalized nutritional advice. Perhaps you will find with this investment, you get patients better faster for less money. Your patients will certainly let you know.
You can check out the program and sign-up for a free demo here: https://thebetternutritionprogram.com/free-resources-from-the-better-nutrition-program/