Practitioner Research Review – May 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- Effects of Prebiotics vs a Diet Low in FODMAPs in Patients With Functional Gut Disorders
- Treatment of hypothyroidism with levothyroxine plus liothyronine: a randomized, double-blind, crossover study
- Mediterranean Diet and Other Dietary Patterns in Primary Prevention of Heart Failure and Changes in Cardiac Function Markers: A Systematic Review
- Rapid-Fire Research – Ultra-concise summaries of noteworthy studies
- The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls.
- Serum Ferritin as a Marker of Thyroid Hormone Action on Peripheral Tissues.
- Association between serum ferritin and thyroid hormone profile in hypothyroidism.
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however, the research studies are a collection of the most clinically meaningful research that has been published recently.
Effects of Prebiotics vs a Diet Low in FODMAPs in Patients With Functional Gut Disorders.
https://www.ncbi.nlm.nih.gov/pubmed/29964041
Study Purpose
- Determine what is more helpful for IBS patients; low FODMAP dieting or prebiotic supplementation
- As summarized by this diagram
Intervention:
- A randomized, parallel, double-blind study of patients with functional gastrointestinal disorders with flatulence
- In 44 IBS patients and 13 with abdominal distention
- Forty-four patients (31 with irritable bowel syndrome and 13 with functional abdominal distension)
- Compared the effects of a
- prebiotic + Mediterranean diet
- 2.8 g/d Bimuno containing 1.37 g beta-galactooligosaccharide plus a Mediterranean-type diet, prebiotic group, n = 19
- vs placebo + Low FODMAP
- 2.8 g/d xylose plus a diet low in FODMAP, LFD group, n = 21
- Patients were treated for 4 weeks, then followed for 2 weeks post-treatment
- prebiotic + Mediterranean diet
Main Results:
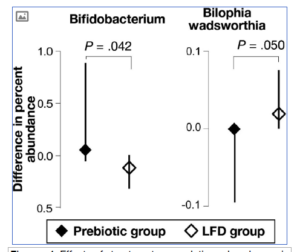
- Microbiota effects were opposite in the prebiotic compared to low FODMAP group. Note: exactly what this difference means clinically is still debatable, so this is more of an academic observation, in my opinion. Some bacteria increased on prebiotics BUT others increased on low FODMAP. Be careful not to assume Bifidobacterium is the ultimate proxy for a healthy microbiota.
- After 4 weeks, we observed opposite effects on microbiota in each group, particularly in relation to the abundance of Bifidobacterium sequences (increase in the prebiotic group and decrease in the low-FODMAP group; P = .042), and Bilophila wadsworthia (decrease in the prebiotic group and increase in the low-FODMAP group; P = .050).
- After 4 weeks, we observed opposite effects on microbiota in each group, particularly in relation to the abundance of Bifidobacterium sequences (increase in the prebiotic group and decrease in the low-FODMAP group; P = .042), and Bilophila wadsworthia (decrease in the prebiotic group and increase in the low-FODMAP group; P = .050).
- Both groups experienced significant improvement symptomatically. Note: but might have favored the low FODMAP (because the prebiotic group did not see improved flatulence or turbulence aka borborygmi aka bowel sounds).
- After 4 weeks, both groups had statistically significant reductions in all symptom scores, except reductions in flatulence and borborygmi were not significant in the prebiotic group.
- The low FODMAP group saw their symptoms return once stopping, whereas the prebiotic group did not. *Important note below on this*
- Although the decrease in symptoms persisted for 2 weeks after patients discontinued prebiotic supplementation, symptoms reappeared immediately after patients discontinued the low-FODMAP diet.
- Here is an important detail that is somewhat overlooked by this study, and will invariably be mis-referenced by those with a prebiotic bias.
- The changes in symptoms post-intervention were not significant! Meaning the overall edge here might go to the low FODMAP diet.
- Recap:
- both diets lead to improvements, but the low FODMAP group may have improved more (more symptoms responded in the LFD group)
- Post-intervention the low FODMAP group regressed, but not in a significant manner and were still better than the baseline.
- Post-intervention there was no significant difference between groups
- However, both strategies had different consequences after treatment discontinuation. Although the improvement of symptoms persisted 2 weeks after prebiotic administration, symptoms tended to relapse after discontinuing the LFD (still lower than pre-treatment), although the change (from treatment values to post-treatment values) was not significantly different between groups (P = .093 by multivariate analysis of variance).
- This could have been an honest oversight, or it could indicate clear biased of the researchers. I say this because their abstract conclusion leaves this out and paints a picture of the prebiotic group clearly responding better.
Additional Results:
- Upon using a prebiotic, patients may experience symptomatic flaring (increased gas production as one example) that should abate after 7-10 days.
Limitations:
- “The study is small, did not estimate long-term efficacy and did not determine whether the prebiotic effect is product-specific or generic.”
Authors Conclusion:
- “Intermittent prebiotic administration might, therefore, be an alternative to dietary restrictions for patients with functional gut symptoms.”
- Thankfully these authors pull back from their initial conclusion, which appears biased, to a more reasonable afterthought in their discussion. Essentially saying, both interventions appear equal, but perhaps we should favor prebiotics since they are easier to administer as compared to dietary restrictions.
- From a practical perspective, our study indicated that, in the short run, daily administration of B-GOS prebiotic was equally effective as an LFD. Because dietary restrictions, particularly the LFD, are cumbersome to follow, these results present an alternative patient management strategy
Clinical Takeaways:
- Here is the clinical hierarchy I lay out in Healthy Gut Health You. It is what I feel to be the best way to incorporate these findings.
- Because those with severe cases may be more prone to have a negative reaction to prebiotics, in these cases, I use them end-stage.
- Since less symptomatic patients appear less reactive, I use prebiotics early on in mild-moderate cases.
- I am not married to this approach, but it appears the most tenable one at the moment.
- Patients may experience symptomatic flaring (increased gas production as one example) that should abate after 7-10 days
Severe cases
- Elimination-type diet (example: Paleo)
- Low FODMAP
- Probiotics
- Habx or Abx
- Prebiotic and fiber trial
Mild-moderate cases
- Elimination-type diet (example: Paleo)
- Prebiotics, fiber and/or probiotics
- Low FODMAP
- Probiotics
- Habx or Abx
What to tell your patients:
- There is excitement regarding prebiotics. Some of this is warranted, however, there is also a significant bias that must be filtered out. In short, the more symptomatic you are (digestively) the more careful we should be with pre The less symptomatic you are the more likely you are to benefit.
Dr. Ruscio Comments
This study provides a great example of why reading only an abstract can get you into trouble. The details can matter. Prebiotics can be used and can be helpful. However, they should also be used cautiously in highly symptomatic individuals.
Treatment of hypothyroidism with levothyroxine plus liothyronine: A randomized, double-blind, crossover study
https://www.ncbi.nlm.nih.gov/pubmed/27982198
Study Purpose
- To compare T4 to T4+T3 for hypothyroidism
Intervention:
- Adults with primary hypothyroidism (n = 32) on stable doses of LT4 for ≥ 6 months (125 or 150 μg/day) were randomized. Note: stable dose means they were doing OK.
- to continue LT4 treatment (G1)
- or to start LT4/LT3 therapy (75/15 μg/day; G2)
- After 8 weeks, participants switched treatments for 8 more weeks.
- Thyroid function, lipid profile, plasma glucose, body weight, electrocardiogram, vital signs, and quality of life (QoL) were evaluated at weeks 0, 8, and 16.
- A randomized, double-blinded, cross-over study
Main Results:
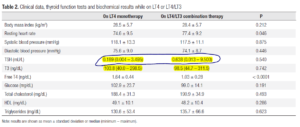
- Free T4 levels were significantly lower while on T4/T3
- TSH and T3 levels were not affected by the type of therapy.
- More patients on T4+T3 had T3 levels above the upper limit (15% vs. 3%).
- The combination therapy led to an increase in heart rate, with no significant changes in electrocardiogram or arterial blood pressure.
- Lipid profile, body weight, and QoL remained unchanged.
- Patients appeared to feel better symptomatically on T4 alone, than on combination therapy.
Limitations:
- This group was not a group of non-responders to T4 therapy. If this group had been, perhaps a positive result would have been seen as we discussed in this recent study.
- You could also make the criticism that the dosage of T4+T3 was insufficient as evidenced by this table wherein those on combination therapy experienced a decline in their T4 and T3 levels when on combination therapy
- HOWEVER, the researchers did a subanalysis to assess if those on combination therapy and with the highest T3 levels might have felt better. They did not. So higher T3 did not equal feeling better.
- We also performed a subanalysis for the group with high T3 levels (T3 > 180 ng/dL), which showed no significant differences regarding QoL scores (global and subgroup scores), VAS scores, body mass index, arterial blood pressure or resting heart rate.
- The researchers also recruited patients on a specific dose of T4 at study entry and then used combination therapy dosages in alignment with previous research which found it improved patients symptoms.
- Instead of using a substitution approach to calculate the dose of LT4/LT3, we recruited participants who were within a very limited LT4 daily dose range (125 or 150 μg/day) and used a fixed combination approach.
- We administered LT4/LT3 at a fixed dose of 75 μg of LT4 plus 15 μg of LT3, regardless of their initial LT4 dose, in the same 5:1 weight ratio as previously evaluated in other studies (12,22,23,24).
- Doses were not adjusted during the study period, as was done by Nygaard and cols. (12)
- It is also possible that the testing showed low T3 due to waiting 24 hours after dosing to collect blood samples
- Although we could not identify increases in T3 levels caused by the combination therapy, it is possible that these results are falsely low due to the short half-life of liothyronine, as well as the fact that blood samples were collected 24 hours after administration of the LT4/LT3 tablets.
Authors Conclusion:
- “The combination therapy yielded significantly lower free T4 levels, with no changes in TSH or T3 levels.”
- “More patients on LT4/T3 had elevated T3 levels, with no significant alterations in the evaluated outcomes.”
- “No clear clinical benefit of the studied formulation could be observed.”
Interesting Notes:
- There is some evidence showing combination therapy can be helpful, but the majority of the data does not support this.
- To date, 15 clinical trials have evaluated the combination therapy of LT4 plus synthetic liothyronine in patients with hypothyroidism [reviewed by Escobar-Morreale and cols. (15)], and one study evaluated desiccated thyroid extract containing both T3 and T4 (20). Clear benefits of the combination therapy were only observed among two groups from Lithuania and Denmark, which reported improvements in mood, well-being and psychometric functionality (11,21), along with better scores of QoL, depression, and anxiety (12).
- Two meta-analyses have not found combination therapy to be effective, as we have previously covered.
- However, a subset of patients exists for which combination therapy seems to help. Likely poor converters.
- However, in the clinical setting, some patients who complain of hypothyroid symptoms (despite having normal TSH and fT4 levels) have mentioned improvements when empirically treated with LT4/LT3 and preferred that type of therapy (15)
- Note: The ratios in all reviewed studies were between 3.4:1 (4:1 by weight) to 17:1 (20:1 by weight). Patients preferences between studies also varied.
- It is possible that a subgroup of patients with deiodinase 2 (DIO2) polymorphisms can benefit from a combination
- Some evidence suggests for the 5-10% of patients T4 alone might not be enough due to poor conversion of T4 to T3.
- Approximately 5-10% of patients continue to report symptoms of hypothyroidism, despite their TSH levels being within the normal reference range (7). Mounting evidence suggests that LT4 monotherapy cannot assure a euthyroid state in the blood and in all tissues simultaneously, and that normal serum thyroid-stimulating hormone (TSH) levels in patients receiving LT4 reflect only pituitary euthyroidism this could be attributed to the fact that the peripheral conversion from T4 to triiodothyronine (T3) is not sufficient to restore normal T3 level
- The authors feel current combination medication offerings are sub-optimal
- Currently available oral liothyronine preparations have an inadequate pharmacokinetic profile. Similarly, commercial preparations that contain levothyroxine and liothyronine contain an excess of the latter and do not mimic the proportion of levothyroxine to triiodothyronine present in normal human thyroidal secretion
Clinical Takeaways:
- Combination (T4+T3) therapy should not be used in all patients
- Combination therapy can be helpful, but only for a minority of patients
- The dosage of T3 might require a high degree of personalization
- Start with T4 therapy and proceed through my algorithm
What to tell your patients:
- Despite what you may read on the internet, the overwhelming majority of data do not support using combination therapy. In fact, using this therapy when not needed may make you feel worse. However, there is a small subset of people who may benefit from combination therapy, so it is an option.
- Problems in the gut will often cause what looks like a thyroid problem. We will work you through an algorithm to sort all this out and make sure you get the therapies that treat the underlying cause of your symptoms, instead of erroneously following internet trends.
Dr. Ruscio Comments
A great paper here. You can tell they did not set up this study in a biased way. However, there are two reasons why we should be cautious with this study’s results.
- The dose could have been inadequate in the combination group.
- The group selected was seemingly healthy and may not have needed to make the switch to combination therapy.
The major issue here is not rushing to combination therapy just because ‘functional medicine guru’s say it’s better’. Follow my thyroid algorithm and you will navigate this efficiently.
Mediterranean Diet and Other Dietary Patterns in Primary Prevention of Heart Failure and Changes in Cardiac Function Markers: A Systematic Review.
https://www.ncbi.nlm.nih.gov/pubmed/29320401
Study Purpose
- Review the data regarding diet, heart failure, and cardiac function
Intervention:
- “A total of 1119 studies were identified, 14 met the inclusion criteria. Studies regarding the Mediterranean, DASH, vegetarian, and Paleolithic diets were found.”
Main Results:
- The Mediterranean and Dash diets might be best for heart health, however, the data here are limited and this conclusion requires further research.
- The effect of the investigated dietary patterns in the primary prevention of HF in adult individuals is not totally clear. It is possible that both DASH and Mediterranean diets may contribute to reduced incidence of HF and a decreased morbidity and mortality in adult patients, but these results need to be analyzed with caution due to the quality of evidence found. There is a need for further investigation on different dietary patterns to elucidate their relationship to primary prevention of HF.
- The Mediterranean and Dash diets dominated the data set here, so this should be considered relative to the conclusion; Paleo and vegetarian were underrepresented. There were also no studies on low fat or low carb.
- A total of 188.470 participants were included in this review.
- Four RCTs [22,23,24,25] and four cohort studies [26,27,28,29] investigated the effects of adherence to the Mediterranean diet and
- Regarding the DASH diet, three cohort studies [30,31,32] and one cross-sectional study [33] were included,
- Finally, a Swedish RCT investigated the Paleolithic diet [34], and a US cross-sectional study investigated the relationship of vegetarian diet and heart failure [35].
- A total of 188.470 participants were included in this review.
Limitations:
- The quality and quantity of the data here are limited.
Authors Conclusion:
- “It is observed that the adoption of the Mediterranean or DASH-type dietary patterns may contribute to the prevention of HF, but these results need to be analyzed with caution due to the low quality of evidence.”
Interesting Notes:
- Many of the Mediterranean diets limited processed grains (good) but also tended to lump in ‘avoid red meat’ along with recommendations to avoid sugar and processed foods (bad, this confounds the signal).
- For the favorable food groups (fruits, vegetables, whole grains, nuts and legumes, and low-fat dairy products) the highest quintile gets 5 points and the lowest quintile gets 1 point. For unfavorable food groups (red and processed meats, sugary drinks, and sodium), the reverse quintile score is applied.
- Another study, which was mentioned in the discussion section of this study, pointed out finding in which the greater the salt restriction the larger the improvement in blood pressure. This might be a select reference, but is interesting none-the-less.
- The DASH-sodium trial conducted by Sacks et al. [12] strengthens the need to reduce sodium intake to prevent CVD. In this study, the DASH dietary pattern was evaluated combined with three different levels of sodium: low (1500 mg/day), intermediate (2400 mg/day), and high (3300 mg/day). The greatest reductions in blood pressure occurred when the DASH diet was associated with sodium reduction (1500 mg/day)
Clinical Takeaways:
- Mediterranean or Dash diets have shown benefit for heart health, however other diets (like Paleo or Low Carb) might also be helpful.
- What to tell your patients:
- The jury is still out regarding if any one diet is the best for heart health. Food quality is likely more important than your specific macronutrients or other refining points (Mediterranean, Paleo, Low Carb, etc…). This point was tacitly reinforced by Dr. Christopher Gardner in our recent podcast.
Dr. Ruscio Comments
I wanted to include this study mainly to arm you with the nuance that while one could easily proclaim “look, Mediterranean and Dash are best for heart health!” that would be a misrepresentation of the data. So, if you have a patient on a Paleo or lower-carb diet, there is no cause for concern from a heart-health perspective.
Rapid-Fire Research: Ultra-Concise Summaries of Noteworthy Studies
The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls.
https://www.ncbi.nlm.nih.gov/pubmed/16500878/
- Low ferritin can cause increased reverse T3
- Subjects with low serum ferritin had a higher ratio of T3/T4 (r = -0.42, P < 0.01). Using stepwise regression analysis, only ferritin contributed significantly to the rT3 concentration (r = -0.35, P < 0.01). The results indicate that the degree of iron deficiency may affect thyroid hormone status in iron-deficient adolescent girls.
Serum Ferritin as a Marker of Thyroid Hormone Action on Peripheral Tissues
https://academic.oup.com/jcem/article-abstract/61/4/672/2675004?redirectedFrom=fulltext
- The relationship between ferritin and thyroid hormones is bi-directional; thyroid hormone administration can increase ferritin levels
- Administration of 75 μg T3 daily for 1 week to 11 euthyroid subjects resulted in a 23–243% (mean ± SD, 117 ± 70%) increase in serum ferritin above basal values. In contrast, in 3 patients with thyroid hormone resistance, the same treatment produced rises in serum ferritin concentrations of only 2%, 5%, and 15%.
Association between serum ferritin and thyroid hormone profile in hypothyroidism
https://www.scopemed.org/?mno=178386
- More data are showing low ferritin is associated with hypothyroidism
- Results: Serum ferritin levels were found to be significantly reduced in patients with hypothyroidism compared to normal subjects (p < 0.001).
What to tell your patients:
- Ferritin can be an overlooked factor leading to non-responsiveness to thyroid hormone replacement. It is important to evaluate this as this may be the cause of your problems rather than other commonly suspected issues: the need for different thyroid Rx, ‘adrenal fatigue’, mold, Lyme, etc…
Thanks to Nick Hedberg for making me aware of these references
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!