Practitioner Case Study – November 2018
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Re-Challenge Studies in Non-Celiac Gluten Sensitivity: A Systematic Review and Meta-Analysis
- To Treat or Not To Treat H. pylori – Dr. Ruscio’s Review of H. pylori Treatment Consensus Data
- Clinical experience with the use of anti-CdtB and anti-vinculin antibodies in patients with diarrhea in Mexico
- Rapid-Fire Research – Ultra-concise summaries of noteworthy studies.
- Update on dietary therapy for eosinophilic esophagitis in children and adults
- Prucalopride succinate for the treatment of constipation: An update
- Parity and 11-Year Serum Thyrotropin and Thyroid Autoantibody Change: A Longitudinal Population-Based Study
- Effects of probiotics consumption on lowering lipids and CVD risk factors: A systematic review and meta-analysis of randomized controlled trials
- Meta-Analysis: Effects of Probiotic Supplementation on Lipid Profiles in Normal to Mildly Hypercholesterolemic Individuals
Practitioner Question of the Month
Practice Tip
Case Study
Patient Info:
- Megan, 33yo female
- Previous Dx
- Celiac, Hypothyroid, PTSD
- Rx
- Birth control (Necon), Levothyroid 125 mcg, Phentermine, Rogaine and Clobetasone – for hair loss
- Chief Complaints
- Anxiety, 5-Int
- Fatigue, 8-Co
- Obesity, 8-Co
- Hair Loss, 7-Co
- Migraines, 5-Int
- Insomnia, 5-Int
Visit 1 (Day 1) – History and Exam:
Initial Impression
Megan presents as a 33yo female on a healthy diet and with a good lifestyle, demeanor, and outlook on her health.
- Previous testing:
- Testosterone high normal
- Onset:
- Gradual onset with no known cause.
- Family history
- Mom: obese, addictions Dad: obese, sleep apnea possibly
- Prior treatments:
- Megan has done well with diet, determining she was celiac and changing diet accordingly help resolve some lifelong complaints. However, she still seems to be suffering from hormonal and autoimmune problems.
- Thyroid Rx – responded well Phentermine – no help
- Notes/DDX
- She has responded well to diet but this has been all she has done so standard GI care and female hormone support may be very helpful.
- Her SS are likely being driven by GI and by female hormones, however, if GI in NR she may have other ddx like adhesions due to previous surgery.
- Prognosis
- I anticipate with the combined hormonal/immune support she should respond moderately.
- Previous Diets
- AIP very helpful for energy, migraines, GI issues, but had cravings. Egg intolerant.
- Previous Treatments
- Thyroid Rx – responded well. Phentermine – no help
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Aerodiagnostics Lactulose SIBO breath test
- Doctors Data Comp. Stool and Parasitology 3x
- LabCorp #2 blood & urine
- LabCorp #1 blood, urine, stool & breath
- Rationale
- We will evaluate SIBO and for GI dysbiosis and/or infection.
- We will also check thyroid function, screen for anemias and look at foundation markers; CMP, CBC w diff, vitamin D
Recommendations
- Dietary
- Please start on the paleo low FODMAP diet
- Treatment
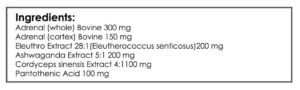
- NRT: vit. D/K, omega 3,6,9 blend
- Adrenal: Adrenal Support formula
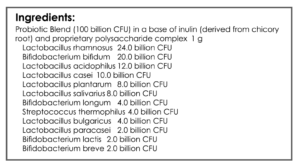
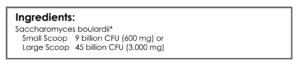
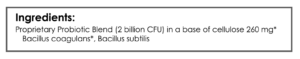
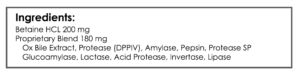
- GI: Lact & bifido probios blend, enzyme with HCl formula, S. boulardii probiotic, soil-based probiotic
- Rationale
- We will evaluate the addition of low FODMAP into her previous paleo-like elimination diet
- Pair this with basic nutritional, GI and adrenal support – remember probiotics are all that is needed to resolve some cases of dysbiosis
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Has not started on diet/program b/c of holiday.
- Improved:
- anxiety – from life calming down.
- Same:
- fatigue, migraines, insomnia
- Worse:
- weight – holidays
Lab Interpretation:
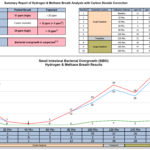
- Aerodiagnostics Lactulose SIBO breath test
- H2 20/32, CH4 5, combo 23/36. classic double peak
- H2 20/32, CH4 5, combo 23/36. classic double peak
- Doctors Data Comp. Stool and Parasitology 3x
- 4 commensals imbalanced. Many yeasts.
- 3x Blastocystis hominis
- 3x Endolimax nana cysts
- 3x Endolimax nana trophs
- 3x Yeast
- LabCorp #2 blood & urine
- Ova and Parasites 3x Examination w/o Giardia
- Abnormal – B. hominis present, Endolimax nana cysts seen
- Indicans, urine qualitative
- Positive Abnormal
- Positive Abnormal
- Ova and Parasites 3x Examination w/o Giardia
- LabCorp #1 blood, urine, stool & breath
- Cholesterol 226-H, LDL 137-H, CRP 4.19-H, T3 Uptake 23-L, Vit D 18.8-L
- Dx
- 1/20/17: mild mixed SIBO. Definite (found LC and DD); Blasto, yeast, E. nana. Low vitamin D, high CRP.
Impression:
- 1/20/17 – Today’s GI finding are likely major driver of sequelae. Has done little other than diet so I expect she should respond well to Habx. Bear in mind other ddx if non-responsive.
Recommendations:
- Continue
- Dietary
- Please start on the paleo low FODMAP diet
- Treatment
- NRT: vit. D/K, omega 3,6,9 blend
- Adrenal: Adrenal Support formula
- GI: Lact & bifido probios blend, enzyme with HCl formula, S. boulardii probiotic, soil-based probiotic
- Dietary
- Starting
- give the diet 1.5 weeks before starting the initial program, then
- start on the initial program 1.5 weeks, then
- start on the antimicrobials
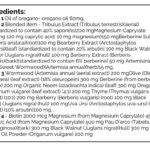
- GI: Habx, base protocol – oregano, antimicrobial blend 1
- FU: 6-8 weeks, midway through the antimicrobial program
- Rationale
- Remember, we don’t need to jump right to antimicrobials. If I were seeing this patient today I would have had her start on diet, then on initial program, then fu. At the fu we could consider Habx if indicated.
Visit 4
Subjective Assessment:
- Paleo Low FODMAP diet – clearly helpful
- Initial program – helpful
- + Oregano, antimicrobial blend – more helpful.
- Needs less Levothyroxine now 🙂 – took a flare of overdosing to determine this
- Improved:
- brain fog, fatigue, anxiety, obesity (20lbs), hair loss, migraines
- Same:
- insomnia
- Worse:
- the feeling of yeast infection
Impression:
- 8/30/17 – Megan has improved vastly, as expected, from initial program plus Habx. She even had a bout of hyperthyroid likely from increase absorption of thyroid Rx, which was alleviated by decreased dose. Will transition to low dose antimicrobials since it seems particularly helpful, in addition to maintaining the previous plan. Option to start vaginally applied hormone cream if vaginal symptoms persist. Fu in 3 months to reintroduce diet, curtail program and consider any retesting.
Recommendations:
- Same a prior, however, we had her start using ¼- ½ dose of antimicrobials.
Dr. Ruscio’s Comments
A few important points from this case.
- A decrease of thyroid medication is possible when you heal the gut. Is this because you have ‘fixed’ the thyroid? Not likely. It’s likely concomitant to increased absorption of their medication.
- Note, sometimes a flare of yeast infection can occur when on antimicrobials. This has appeared to be self-limiting and short lived in most cases in my experience. If an antibiotic is needed, I am not worried about it since it fits in with the theme of the previous antimicrobial treatment anyways.
- We did not jump to retesting. I am sure her tests would have looked better. But this is not the point. The goal is to assess and support/treat her but until she has achieved and maintained the clinical outcome. If you achieve this, the labs usually support what the patient presentation has found. Megan, who wasn’t great with compliance, followed up 14 months later. She had been doing great other than recently when she started noticing some of her symptoms returning. She had been under quit a bit more stress and had been quite lax with her diet. She was also off everything in her program. I anticipate a gentle push with probiotics, combined with being a bit more careful with her diet (but not going to the point of dietary zealotry), will get her back to her previous optimal. Consider this, what a waste the retesting at this point would have been. What would it show us? At most, we would have seen a less severe variation of her original labs. OK, and then we would do what? Exactly the treatments that had worked for her before. Great, so we spent several hundred dollars to do the same treatment again. This is exactly where functional medicine trips over its own feet. Yes, some testing can be helpful, but serial retesting needs serious reconsideration.
- This is one of the more rare cases where there is a high agreement between different stool/GI evaluation (LabCorp and Doctor’s Data).
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine



Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!