Practitioner Research Review – October 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
- Ileocecal Valve & SIBO: Dr. Ruscio’s Mini-review
- Lead and cadmium exposure, higher thyroid antibodies and thyroid dysfunction in Chinese women
- Mast cells at the crossroads of microbiota and IBD
- Rapid-fire Research – ultra concise summaries of noteworthy studies
- Perspective: Fundamental Limitations of the Randomized Controlled Trial Method in Nutritional Research: The Example of Probiotics
- Serum Thyroglobulin-A Sensitive Biomarker of Iodine Nutrition Status and Affected by Thyroid Abnormalities and Disease in Adult Populations
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Ileocecal Valve & SIBO: Dr. Ruscio’s Mini-review
Background:
The ileocecal (IC) valve regulates movement of luminal contents from the small to the larger intestine. One theory states that IC valve dysfunction is a significant factor contributing to SIBO. I have been open to this theory, but admittedly skeptical. So, I decided to review the data to see if there is anything to this hypothesis.
Conclusion:
The majority of the data suggests IC valve dysfunction is associated with SIBO. The data here come from smaller sample size studies, so larger studies are needed to more definitively establish this conclusion.
It appears likely that IC dysfunction occurs as part of a larger syndrome of dysmotility. Thus, it might be most accurate to say dysmotility is associated with IC dysfunction & concomitantly with SIBO.
Surprisingly, post-surgical patients (bowel resection) wherein the IC valve is altered or removed and recreated, do not experience an increased prevalence of SIBO. This is important to note as sometimes this data is cited to refute the impact IC function has on SIBO.
“Even those who have had their IC removed or surgically altered don’t experience higher rates of SIBO, so the IC can’t be that impactful.”
Evidence:
IC dysfunction associated with SIBO, in non-surgically altered subjects. Dysmotility statements in red font.
- Patients with SIBO have significantly lower ICJP, prolonged SBTT, and a higher gastrointestinal pH as compared to those without SIBO. [1]
- Ileocecal junction pressures were significantly higher in LBT(-) negative vs. LBT(+) (79.9 vs. 45.1). [2]
- Low IJP is significantly associated with SIBO.
- Small bowel transit time was significantly longer in LBT(+) versus LBT(-) (5.82 vs. 3.81 h, p = 0.05).
- Compared to normal, subjects with a positive lactulose breath test have a defective ICV cecal distension reflex. [3]
- And only one study refuting the associated between IC function and SIBO [4]
Data regarding post-surgical patients not listed.
Clinical Takeaways:
- IC valve dysfunction is associated with SIBO, but is likely part of a larger syndrome of dysmotility. Thus, the clinical aim might be towards a more global aim (motility) rather than a localized focus (the IC valve).
- The exception here could be any type of adhesion in the IC region.
- What to tell your patients:
- Working to improve your motility should improve your IC function, as the IC valve is likely a reflection of your overall motility function.
- You may also be a candidate for manual therapies to remove restrictions and or scar tissue in your abdomen (only if history, signs and symptoms support).
Dr. Ruscio Comments
It appears that yes, IC dysfunction is associated with SIBO. Good to know. Now, the next question is how do we treat this? Likely through improving motility. How do we do this? In my opinion much of what we already do for IBS appears to improve motility; diet (including low FODMAP, speculatively), fasting, reducing inflammation, probios, SIBO treatments, prokinetic therapy…
Also, keep in mind some patients may require more manual/visceral therapies to address a structural issue.
Lead and cadmium exposure, higher thyroid antibodies and thyroid dysfunction in Chinese women.
Environ Pollut. 2017 Nov;230:320-328. doi: 10.1016/j.envpol.2017.06.052. Epub 2017 Jun 28.
Study Purpose
- To determine whether the blood levels of lead(BPb) or cadmium(BCd) related to the levels of sera antibodies to thyroid proteins and thyroid dysfunction in the general population.
Intervention:
- 5628 Chinese adults
- Thyroid dysfunction and subclinical thyroid dysfunction were defined by
- Total T3, T4, and TSH.
- TPO and TG antibodies.
- BPb and BCd levels were tested by atomic absorption spectrometry.
Main Results:
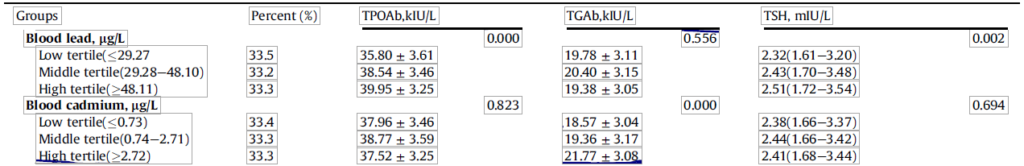
- Summary: Lead and cadmium were associated with either increased autoimmunity and/or hypothyroidism, even after adjusting for age, BMI, smoking, and drinking.
- After adjustment for age, body mass index, smoking status (men only) and drinking status, the Pb was positively related TPOAb and to TSH in women.
- The Cd in women was positively related to the TGAb
- In the adjusted logistic regression models, the Cd of women was positively related to their hypothyroid status and TG Abs.
- The ORs of women in the middle and higher TPO Ab tertiles were 1.38 (P < 0.001) and 1.35 (P < 0.001) times greater for every unit increase in Pb, respectively.
- In men, no continuous correlation was found among variables.
- However, these findings and conclusions by the authors could be very easily misinterpreted and misrepresented by the natural/functional medicine community.
- The researchers defined normal for TPO and TG antibodies as below 60
- The upper limits of the normal range for TGAb and TPOAb were both 60 kIU/L.
- The changes in thyroid antibodies when going from low, medium to high levels of lead/cadmium were statistically significant but were not clinically meaningful. In fact, they never even reached the positive range.
- In women, TPOAb levels in the low BPb tertile, the middle BPb tertile and the high BPb tertile were 35.80, 38.54, and 39.95, respectively.
- In women, TGAb levels in the low BCd tertile, the middle BCd tertile and the high tertile were 18.57, 19.36 and 21.77 with significant difference among groups
- The researchers defined normal for TPO and TG antibodies as below 60
Limitations:
- This was a Chinese population, which to my understanding, will have higher levels of exposure to lead and mercury.
Authors Conclusion:
- “In women, BPb and BCd levels were related to higher TSH and hypothyroid status, respectively, suggesting a Pb and Cd induction of sex-biased thyroid autoimmunity.”
- “In women, blood Pb and Cd levels were related to higher TSH and hypothyroid status, respectively. Toxic metal induction of thyroid autoimmunity may be one pathogenic mechanism behind this. Further prospective studies and animal studies are needed to clarify the causality and underlying mechanisms.”
Interesting Notes:
- The majority (73%) of thyroid autoimmunity may be genetic. So, yes we want to improve the environment, but as I have said before we should not obsess over ‘normal’ antibodies as it may not be modifiable.
- “In the 1980s, when people finally became aware of the serious neurotoxicity of Pb in both adults and children, Pb was banned from use in gasoline by most countries. Despite this, Pb exposure still occurs through contaminated water, lead-laced toys, and cosmetics, etc.”
Clinical Takeaways:
- Some data have found as lead and cadmium blood levels increase, this correlated with thyroid autoimmunity and TSH. However, the effect size appears negligible and not clinically meaningful.
- The environment may only affect 20-30% of thyroid autoimmunity.
- What to tell your patients:
- Repeat above and mention this is something to potentially explore but only end phase and if symptoms persist after exhausting all other options.
- The environment may only affect 20-30% of your thyroid antibodies, so we will act but not obsess over antibody levels.
Dr. Ruscio Comments
The main point here is that there is a vast difference with two conclusions one could make from reading the ABSTRACT of this study.
- Incorrect: Heavy metals have shown to worsen your thyroid autoimmunity and function and must be addressed.
- Correct: Heavy metals may play a role but generally, appear insignificant unless you are allergic to a given metal or have an unusually high industrial exposure.
Mast cells at the crossroads of microbiota and IBD.
Eur J Immunol. 2018 Dec;48(12):1929-1937. doi: 10.1002/eji.201847504. Epub 2018 Nov 19.
Study Purpose
- Outline impact of mast cells in IBD
Innervation:
- Review, non-systematic.
Interesting Notes:
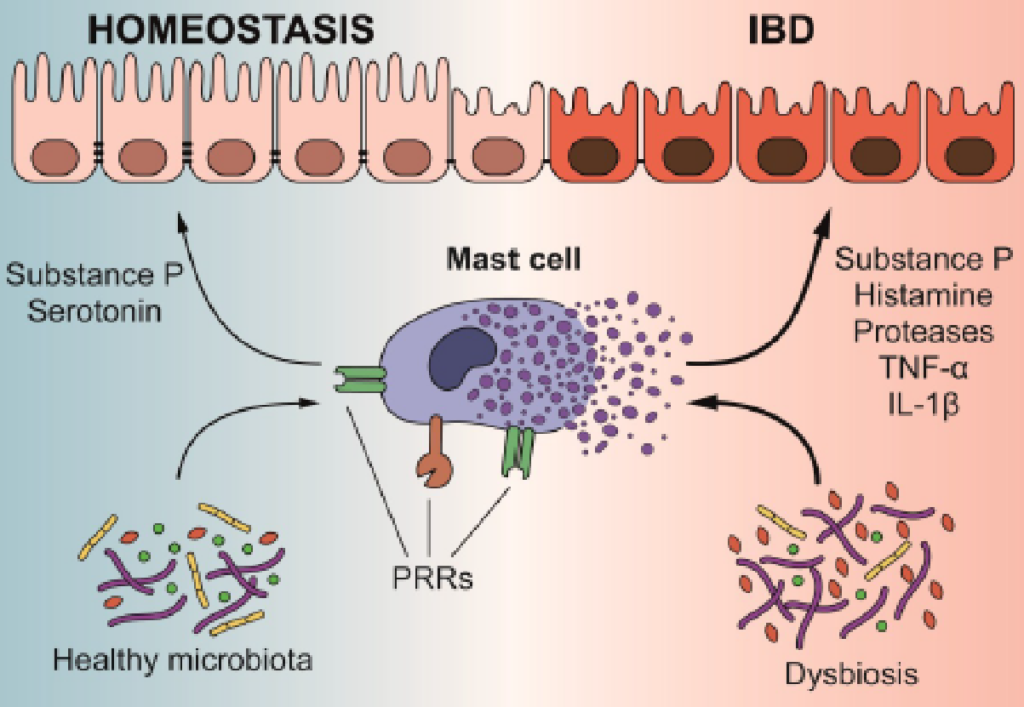
- Microbiota does impact mast cells, this is why improving GI health is crucial with IBD patients
- The ability of some bacteria to specifically affect MC functions and activation has been extensively studied
- Great diagram (PRRs, pattern recognition receptors) illustrating how the microbiota impacts the immune system. My note: This is the hot burning causal core of many patient’s sequelae
- Reminder, the microbiota impacts the immune system but also the nervous system (hence motility)
- The gut is a complex universe in which the intestinal mucosa co-exists with the nervous system, the commensal microbiota, and the immune system
- There is a bi-directional relationship between the microbiota and the immune system, this includes fungus
- Over the last two decades several reports were able to demonstrate that bacteria and fungi induce MCs activation.
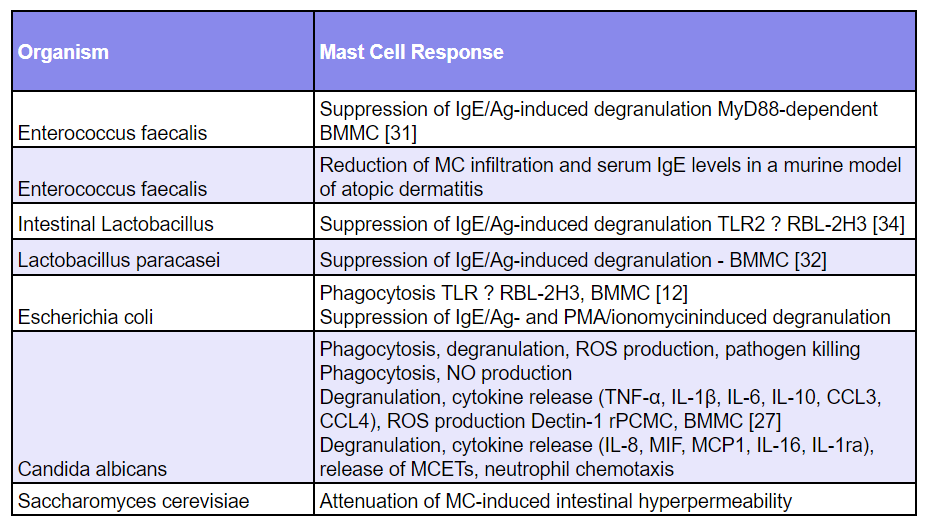
- Interestingly, although some microorganisms can elicit a proinflammatory response of MCs, other microorganisms are able to reduce their activation, thus limiting inflammation and promoting homeostatic conditions, highlighting the key role of these neglected cells in the control of tissue inflammation and homeostasis
- Post-infectious IBS patients have increased immune activation aka increased mast cell activation. IBD patients also show signs of increased mast cell activation.
- In recent years, a growing body of publications clearly showed that patients with post-infectious IBS have increased MC activation [53,54,55].
- Patients affected by IBD in remission frequently show functional gastrointestinal symptoms similar to those developed by patients suffering gastroenteritis [56]. Supporting the hypothesis of an involvement of MCs in IBD, an increased secretion of histamine and tryptase has been documented in biopsies from the duodenum, colon, and rectum of IBD patients
- Probiotics can attenuate an overzealous immune response via mast cell regulation
- In line with the growing body of evidence highlighting the effectiveness of the use of probiotics in the treatment of patients affected by IBS and IBD, it has been recently demonstrated that dietary administration of S. cerevisiae-derived β-glucan was able to attenuate MC-induced intestinal hyperpermeability in patients affected by Crohn’s disease ileitis as well as in non-inflammatory IBD subjects, highlighting again the key role of these cells in bridging pathology and dysbiosis [75,76,77].
- There are still gaps in the published data, but preliminary research show probiotics and/or dysbiosis can influence mast cell activation. My note: an astute GI clinician has likely figured much out much of what works already through empiricism (diet, probiotics, dysbiosis treatments…).
- Most of the data obtained thus far and discussed here, derived from in vitro or in vivo animal studies because studies on humans are still scarce
- Most of the data obtained thus far and discussed here, derived from in vitro or in vivo animal studies because studies on humans are still scarce
Authors Conclusion:
- “The data discussed here provide evidence that the alteration of gut functions in the context of IBD can be the consequence of MC hyper-reactivity caused, in turn, by microbiota dysbiosis.”
Clinical Takeaways:
- The microbiota influence mast cells and this influence is only beginning to be appreciated
- Probiotics and dysbiosis influence mast cells and thus GI immune activation
- What to tell your patients:
- Overzealous immune reactivity and inflammation play a major role in IBD and IBD.
- Probiotics and dysbiosis are two modifiable factors that can improve your immune system ie mast cell activation.
Dr. Ruscio Comments
While mast cell activation can sometimes appear as a clinical challenge requiring its own, unique treatment approach, foundationally mast cell activation follows the same treatment algorithm as IBS and IBD. MCAS can require unique treatments, but it is important not to overlook the foundation.
Rapid-Fire Research: Ultra-Concise Summaries of Noteworthy Studies
Perspective: Fundamental Limitations of the Randomized Controlled Trial Method in Nutritional Research: The Example of Probiotics.
Adv Nutr. 2018 Sep 1;9(5):561-571. doi: 10.1093/advances/nmy046.
Study Purpose
- Discuss the limitations of randomized control trials in the study of nutrition, mainly in probiotics.
Findings and Notes
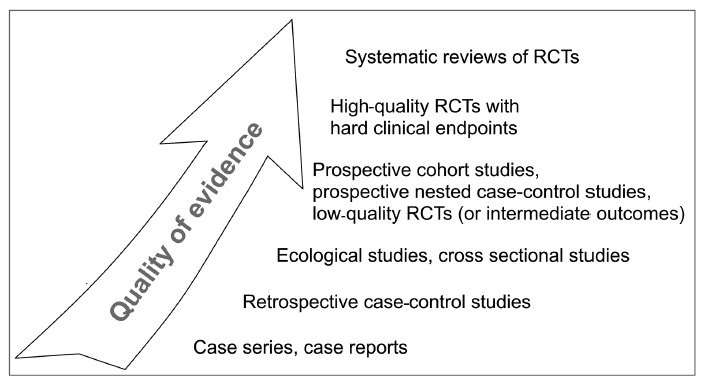
- Just a reminder of what the quality of evidence tiers looks like
- I agree with the authors that conventional medicine/research can be quick to dismiss therapies when there are either limitations or inconsistencies in the research. Probiotics are a good example of this. Despite a substantial body of evidence showing that probiotics can improve IBS, and do so without adverse events, some researchers state probiotics can’t be recommended because of heterogeneity in the strains or dosages used. This is especially irritating when considering that the other therapies mentioned (let’s say tricyclic antidepressants) have notable adverse events.
- However, if an appreciable effect is achieved from therapy, it appears this effect is usually able to be detected in the trend in the RCTs. While single studies may vary, with additional studies a trend will develop and the trend line is usually fairly accurate, in my observation.
Serum Thyroglobulin-A Sensitive Biomarker of Iodine Nutrition Status and Affected by Thyroid Abnormalities and Disease in Adult Populations.
Biomed Environ Sci. 2017 Jul;30(7):508-516. doi: 10.3967/bes2017.067.
Study purpose:
- Assess if serum thyroglobulin (not thyroglobulin antibodies) track with iodine status or thyroid function.
- Key question: can serum TG be used to assess iodine insufficiency and excess?
Findings and Notes:
- Excess or deficient iodine intake was associated with higher thyroglobulin (TG) levels (between 15-22 µg/L).
- A total of 573 adults were recruited for this study.
- The serum Tg levels differed significantly among the three groups (27 μg/L, 9.73 μg/L and 15.77 μg/L in the excess, more-than-adequate, and deficient groups, respectively).
- The results of multivariate linear regression analysis indicate that excess and deficient iodine intake, goiter, thyroid nodule, hypothyroidism are significantly related with higher Tg level
- While this is interesting, it is challenging because the TG levels were within the normal range (3.5-77 µg/L). However, this test is normally used for tumor tracking post thyroidectomy assessment – so the use in this study (iodine status) is different.
- We could perhaps pose a suggested range for TG in iodine assessment.
- Caution of excess or deficient intake >10 µg/L
- Excess or deficient intake > 15 µg/L
- normal range of the Tg reference is 3.5-77 μg/L.
- The TG differences between excess or deficient intake, compared to normal controls, was statistically significant.
- Specifically, compared with that of the more than adequate iodine group, the median serum Tg levels of both iodine excessive and deficient groups were significantly higher (P < 0.01)
- Hypothyroid also correlated with TG, however, since we already have easy/accurate testing for hypothyroid it isn’t advisable to use TG. The same also applies for thyroid nodules.
- While this is a preliminary finding, and thus should be applied very conservatively, it is not the only of its kind
- LabCorp and Quest offer thyroglobulin [16,17]
Dr. Ruscio’s Comments:
I am considering tracking this marker in some cases to assess iodine status.
I’d like to hear what you have to say regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what you’re reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!