Practitioner Case Study – May 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case Study
Research
- Effects of Prebiotics vs a Diet Low in FODMAPs in Patients With Functional Gut Disorders.
- Treatment of hypothyroidism with levothyroxine plus liothyronine: A randomized, double-blind, crossover study
- Mediterranean Diet and Other Dietary Patterns in Primary Prevention of Heart Failure and Changes in Cardiac Function Markers: A Systematic Review
- Rapid-Fire Research – Ultra-concise summaries of noteworthy studies.
- The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls.
- Serum Ferritin as a Marker of Thyroid Hormone Action on Peripheral Tissues.
- Association between serum ferritin and thyroid hormone profile in hypothyroidism.
Practitioner Question of the Month
Practice Tip
Case Study
Dr. Ruscio’s Comments:
This is a case study from our audience, Dr. Robert Abbott. I have highlighted a few points below that I feel are of importance.
Thank you, Robert. This was a poignant case study illustrating how impactful the concepts we embody in the Future of Functional Medicine Review (FFMR). You helped this patient find her way through the wasteful landscape in functional medicine and delivered her results, quickly and cost-effectively.
Specifically, you undiagnosed her previous, erroneous ‘hypothyroid diagnosis’. As I have been saying, this problem is becoming endemic in functional medicine. This patient, as with many others, felt worse when on unneeded thyroid medication.
You also pieced together that GI treatment was the most effective line of therapy she had tried prior, but for some reason was quickly abandoned by her former providers for other therapies.
Summary: Master what we cover in the FFMR and you WILL help people who others have been unable to, in less time and at less cost.
Bravo Robert!
Patient Info:
Susan is a 31 y/o female with PMHx of multiple AI diseases including hypothyroidism and celiac disease as well as multiple psychiatric disorders including GAD, PTSD and panic attacks. She is seeking to address the following symptoms and health concerns:
- Hormone fluctuations/PCOS
- Anxiety and panic attacks
- Metabolic dysregulation and insulin resistance
- Poor sleep
- Digestive issues: constipation, nausea, bloating
- Weight loss resistance
Previous Treatments and Therapies
- Follows an AIP dietary template – now in reintroductions
- Worked with a health coach and NTC to address nutrition for autoimmune disease
- Worked with various integrative health providers
- Addressed clinically diagnosed SIBO in 2017 with prescription anti-microbials
Current short and long-term health goals
- Conceive off of anxiety medications
- Address digestive complaints
- Investigate and address hormonal concerns – previous Dx of PCOS
- Weight loss
- Optimize nutrition for conception
- Improve anxiety, eliminate panic attacks
Visit 1 – Initial History and Exam:
SUBJECTIVE
Susan presents as a 31 y/o F who has been diagnosed with three different autoimmune conditions over the past 3 years and continues to be bothered by continued psychological concerns included anxiety and panic attacks as well as GI symptoms including constipation, nausea and bloating. She has worked extensively with a health coach to implement dietary changes following an AIP template to address multiple AI diseases. She has performed numerous reintroductions with the protocol and feels at a stable place nutritionally. She is seeking support primarily to eventually conceive and desires to titrate off and stop current psychiatric medications given this goal.
Past Medical History/Timeline
- PMHx is significant for generalized anxiety disorder, PTSD and panic attacks beginning around 2011 during a period of growth and processing of early life trauma. She did not begin any psychotropic medications at this time.
- She struggled with multiple health complaints through 2011 into 2012 and was finally diagnosed with Celiac Disease in 2012 via antibody testing. States she did not pursue diagnostic endoscopy. Is unable to provide the laboratory results confirming this diagnosis.
- Reported some improvement with the removal of gluten, however, she struggled with extreme anxiety, more fatigue and GI complaints into 2014. She began seeing multiple integrative health practitioners and was eventually diagnosed with adrenal fatigue, candida, and hypothyroidism. She was put on compounded combination thyroid hormone replacement.
- Following this diagnosis she improved only marginally, still suffering from fatigue and joint pains mainly in her upper extremities. She was diagnosed in 2015 with RA, PCOS and a variation in the MTHFR gene.
- She eventually moved from California to Maryland in 2016 and began suffering flares of anxiety, fatigue and GI symptoms prompting her to begin work with the previously mentioned health coach who guided her into following the autoimmune protocol. She reported treatment for clinically diagnosed SIBO in 2017 and did one round of prescription antimicrobials with significant improvement.
- She began psychotropic medications in late 2017 as she deepened her work with the nutritionist. She was prescribed Clonazepam 0.5 mg twice daily and escitalopram 20 mg daily.
- She reported significant improvements in 2018 with most symptoms resolving and now in late 2018 is desiring to continue exploration into previously outlined areas with the main central goal of optimizing the environment for conception.
- She reports being given numerous supplement recommendations previously with the most recent recommendations noted below. She stated this was a burden and that she was not taking nearly any of these recommended products.
Medical Symptoms Questionnaire
- GI Tract: constipation, bloating, belching
- Ears: itchy ears, tinnitus
- Emotions: anxiety, mood swings
- Energy: fatigue, lethargy, restlessness
- Eyes: itchy eyes, swollen eyelids
- Nose: hay fever, stuffy nose
- Head: insomnia, headaches, and dizziness
- M/S: arthritis
- Skin: hives
- Weight: excessive weight and food cravings
- GU: genital itch
OBJECTIVE
Supplements
- MTHF 1 mg daily
- B-12 1 mg daily
- Rhodiola Rosea, 100 mg twice daily
- Nanoemulsified DIM, 20 mg, 4 pumps twice daily
- Nanoemulsified D3K2, 5000 IU, 2 pumps daily
- Spore-based broad-spectrum probiotic & prebiotic, 620 mg, 1 capsule daily
- Fish Oil 445 mg, 4 capsules twice daily
- Colostrum, 1000 mg, 2 capsules daily
- Magnesium glycinate, 120 mg, 6 capsules at night before bed
- Digestive Enzymes, 1 capsule before meals
- Digestive Bitters, 1 dropper full after meals
- Zinc, 30 mg, 1 capsule daily
- Beef Liver, 4 capsules daily
- Restorative Gut Nutrients product, 150 mg, 1 tsp three times daily
Prescription Medications
- Compounded T4/T3 75/7.5 mcg 1 capsule daily since 2014
- Naltrexone, 3 mg, 1 capsule daily since 2016
- Escitalopram, 20 mg, 1 tablet daily, since December 2017
- Clonazepam, 0.5 mg, 1 tablet twice daily, since December 2017
Allergies
- Gluten- reactions range from severe headaches to hives, digestive issues, severe bloating
- Cow Dairy- stomach pains, diarrhea, constipation, flatulence, bloating
- Soy- bloating, constipation
- Peanuts -bloating, constipation
- Nightshades- makes joint symptoms worse
Lifestyle & Diet Review
Non-smoker, non-drinker who enjoys her work as a freelance writer. She has recently significantly increased her physical activity including more formal workouts. She follows an AIP dietary template. Main stressors appear to be around health and life in general. Sleep seems to be problematic even with good sleep hygiene. Positive eustress is noted with recent engagement and planning of a wedding.
Laboratory Assessment
2015 Comprehensive Stool Analysis
- Pancreatic insufficiency – low fecal elastase
- Dysbiosis
- Candida overgrowth
- Elevated EPX and sIgA
August 2017 Comprehensive Stool Analysis
- No signs of fat malabsorption or insufficiency
- No candida
- Normal fecal elastase
2017 Bloodwork
- Elevated monocytes, eosinophils, normal WBC
- Glucose 99, HgbA1c 5.2
- ALT at 112, AST at 49
- TSH 3.4 with normal range Free T4 (1.48 ng/dL)
- TPO Ab and TGA normal
- Vit D 25: 57.2, Vit D 1,25: 74.0, Concordant
- Negative ANA and Anti-CCP, normal ESR
- Iron Profile – normal
- DHEA- S – elevated
- Testosterone- high normal
- Negative candida Ab’s
Additional Previous Bloodwork
- Negative Western Bloat for Lyme, Negative Babesia Ab’s
- Negative EBV, appears to have had no exposure previously based on titers
Genetics Overview
- 1298C MTHFR Homozygote
- COMT V158M -/- (GG) (Lowest Dopamine- Warrior Phenotype)
- Celiac Genetics- one allele for DQ2.5
Clinician Summary
Since 2014, Susan has had significant laboratory testing, the majority of which has been excessive, wasteful and clinically unimportant. I am appalled at the course of laboratory testing that was pursued by multiple providers.
Not listed above included a homeopathic sensitivity test for multiple food and environmental antigens, multiple cortisol and hormonal panels that proved entirely useless, repetitive and excessive bloodwork including workups for chronic Lyme, chronic EBV, and other chronic infections. Upon further discussion, she was diagnosed with hypothyroidism despite normal TSH and Free T4, but was started on medication because “other markers pointed to her thyroid needing support.” She has never at any point showed elevated thyroid antibodies, had a negative Rheumatoid Factor as well as a negative anti-CCP Ab – a specific test for rheumatoid arthritis (RA) that can sometimes be elevated prior to the onset of clinical symptoms, but was still told her joint symptoms were related to RA. While she could not provide the celiac antibody testing results, genetic testing confirmed she did at least have one risk allele for the DQ2.5 risk haplotype.
It is notable that she showed clear GI dysfunction in 2015 with improvement in a repeat stool sample in 2017 (the same year she pursued antimicrobial treatment for SIBO), however, testing and treatment throughout and following was pursued in other domains rather than GI health.
It is disheartening to see that she had been on thyroid medication that she likely did not need, was diagnosed with RA, which she does not have, was tested for every chronic thing under the sun without clinical reason, placed on numerous supplements despite a persistence with overt GI dysfunction and symptoms pointing to imbalances in energy production and the GI tract.
What is perhaps even more troubling is the worsening of anxiety and panic following the use of thyroid hormone replacement. She additionally noted that there was a period of time where the doctor did not refill her thyroid medication and she went several weeks without it and began to actually feel a little better, but dismissed this as she felt it was simply getting back to baseline after having a slight worsening acutely after stopping the thyroid replacement.
ASSESSMENT
Working Differential of Concerns
- HPA Axis Dysregulation
- Female Hormone Imbalance- Elevated Androgens, DHEA, PCOS
- Dysbiosis with potentially pathogenic organisms
- Methane Predominant SIBO
- SIFO
- Maldigestion/Malabsorption
- Immune Dysregulation
- Iatrogenic thyroid suppression
- Nutrient deficiencies secondary to maldigestion/malabsorption and SIBO
- Mast cell activation, coming from GI tract?
Global Assessment
Susan is a young overweight female with an extensive past medical history most notable for celiac disease, hypothyroidism, rheumatoid arthritis, panic disorder, PCOS, anxiety, and PTSD who presents for her initial intake visit seeking to make progress regarding her hormonal imbalances/PCOS, neuropsychological symptoms, and digestive issues including constipation and bloating. She has already made significant progress in working with Angie Alt to implement AIP, reintroductions and other positive lifestyle changes. She persists with excessive weight, hormonal imbalances, controlled anxiety, and less frequent panic attacks, but has remained on medication with the desire to discontinue medications prior to conception.
She has had extensive previous testing include functional nutritional and stool testing, but none since 2017. A review of these findings can be seen above in the note. Most concerning, however, is clinically observed fat malabsorption as noted by the patient’s self-report of the pale stool as well as previously noted 2015 stool studies showing pancreatic insufficiency.
She is very motivated with external sources of support and accountability. She has additionally suffered some fairly significant trauma with subsequent therapy and mourning assisting in her progress positively forward. Her faith and relationships appear to be her strengths and anchors in life in addition to pursuing her passions in writing.
Given her symptoms, the patient will likely benefit from updating current blood work, performing a stool test with a potential SIBO breath test if stool testing is inconclusive and GI symptoms persist. Longer term we can potentially assess hormones given previously elevated DHEA-S and androgens via blood testing and urinary hormone testing. Organic acid testing including fatty acid composition, toxic element screen, repeat assessment of thyroid function, vitamin D, and an iron profile will all be helpful to optimize the environment for conception, however, current concerns must focus on gut health and its assessment.
I expect the patient to make positive improvements by supporting digestion, examining gut and hormonal health with a trajectory for optimal improvement over 6-9 months. I suspect she does not need thyroid hormone replacement and does not appear to have clinical indicators of RA. We will need to pursue titration off and stopping thyroid hormone as well as exploring dietary modifications to support weight loss.
PLAN
Core Treatment Pathways
- Digestive Support and Supportive Gut
- Core Nutritional Support
- AIP Reintroductions with an exploration of the ketogenic diet
Lifestyle Treatment
Nutrition
- AIP with Reintroductions, explore fodmap and keto if needed
Movement/Exercise
- Has increased this and will encourage continuing current structured workouts
Sleep
- Will review hygiene and explore needs for additional supplementation
Stress Management
- Appears motivated to combine spiritual practice with contemplative stress management
Community/Relationships
- Strong and nourishing
Wisdom
- Strong faith as evangelical Christian, appears motivated to combine spiritual practice with contemplative stress management
Play
- Enjoys her work and has several hobbies
Nature/Environment
- Will encourage time in nature even more despite the winter as we move into the spring months
Initial Supplementation
Noted to not be taking many of previously recommended supplements (by other providers). We will advise that she should discontinue these and optionally can continue using essential oil products as desired.
- Betaine HCl
- Digestive Enzymes
- Vit D/K2
- Saccharomyces boulardii
- Cod Liver Oil
Additional Testing Considerations
- GI-MAP stool testing
- Blood chemistry panel: CBC CMP, Vit D, Lipids, Homocysteine, HgbA1c, DHEA-S, SHBG/Free Androgen Index, repeat thyroid after stopping the medication
Future Pre-Conception Testing
- DUTCH urinary hormone testing
- Genova Diagnostics NutrEval organic acid testing
- Blood chemistry: iron panel, repeat thyroid, defer B12 and folate as will be doing organic acid methylmalonic acid and FIGlu
Visit 2: 2 weeks later
Visit Summary
During this visit, we discussed Susan’s most recent visit with her nutritionist and health coach, our interpretation of previous laboratory testing as well as initial recommendations for supplementation and testing. Susan very much appreciated the small amount of initial supplementation and also agreed to pursue stool testing first, followed by breath testing if it was inconclusive and she still persisted with GI symptoms. She liked the idea of pursuing further dietary re-introductions as well as intermittent fasting, extended fasting, and a ketogenic macronutrient template. She expressed that she had had negative reactions to GABA supplements in the past and this would not be a good alternative as she sought to titrate off psychotropic medications.
She agreed and was willing to stop thyroid hormone replacement and pursue blood chemistry testing including thyroid function in 6-8 weeks after stopping the medication. We discussed given her longer-term vision of conceiving, non-pharmacologic and supplement therapies that would be aligned with this goal. She agreed to pursue urinary hormone testing at a later date as well as nutritional organic acid testing closer to the desired date of conception.
Clinician Commentary
In functional medicine, we cannot get caught up with fancy testing and supplementation or get dragged into the weeds of things that are not foundational. We must also do our due diligence to construct a pathway of healing and exploration that is logical, iterative and affordable. We must start with foundational lifestyle therapies, explore areas that appear clinically impacted with specific testing that will actually change or dictate treatment, and only use supplementation for very specific needs. As Dr. Ruscio has pointed out in previous newsletters, we must not become cynical, but rightly inquire about previous medical history as we may discover an erroneous diagnosis and perhaps even medications that are unnecessary and harmful. Performing significant testing while potentially enlightening is almost always practically and clinically unhelpful as certain areas will improve with other foundational therapies and it is impractical to try to address identified heavy metal toxicity, gut dysfunction, methylation issues, female hormone imbalance, and impaired detoxification all at once- hence the need to outline an iterative approach for you and the patient. You may not get the person better overnight and you may recommend things that don’t work along the way, but the process must be methodical and iterative as well as doable for the patient.
Visit 3: 4 weeks later
Visit Summary
Implementation visit with nutritionist focused on dietary reintroductions, the use of Cronometer to track macro and micronutrients given desire to follow a ketogenic template and mitochondria. She expresses improvements in bloating and bowel movements with the enzymes. She reports stopping her thyroid medication.
Visit 4: 2 weeks later
Visit Summary
Implementation visit with nutritionist focused on new dietary recommendations amidst other lifestyle changes. She is preparing for a trip to California. Has completed the stool test and it will result in the next 2 weeks. Has maintained previous gains with regards to GI symptoms and improving energy. She is not noticing any major negative effects of stopping thyroid medication.
Visit 5: 4 weeks later
SUBJECTIVE
Visit Summary
The patient meets with me once again to review stool testing and recent blood chemistry. She has continued with previous gains, rating her health as an 8/10 with continued improvement since the previous visit. She is following a ketogenic dietary template and intermittent fasting closely.
In exploring symptoms it appears she still is bothered a little with intermittent constipation described as both infrequent stools and hard stools: Bristol 1-2. It does seem that these symptoms are worsened during the second half her menstrual cycle after ovulation and subside with menstruation.
She has begun tapering Clonazepam with her psychiatrist and plans to be off completely in 2 weeks with subsequent titration in escitalopram. She states she stopped her thyroid medication at the end of January and feels completely normal. She reports finishing planning for her wedding in 2 months, which is stress relief. She has not had any new acute concerns.
OBJECTIVE
Laboratory Findings and Review
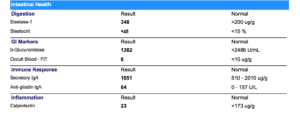
GI MAP 3/5/2019
Blood Chemistry 3/15/2019
- Blood sugar well balanced – HgbA1c 5.1
- High DHEA-S with normal bioavailable testosterone, still higher androgens
- Balanced kidney, liver function, electrolytes
- Low normal protein, low creatinine – low muscle mass?
- Slightly elevated WBC count, elevated eosinophils could be a sign of an allergic-type response
- Ideal Vitamin D
- Ideal blood fats- cholesterol, triglycerides
- Normal thyroid function
ASSESSMENT
Susan reports continued improvements in her health and is very happy overall with her progress. GI MAP testing showed no imbalances with no pathogenic overgrowth or even the remote presence of a potential pathogen. Additionally, sIgA, calprotectin, steatocrit, and fecal elastase are all normal. Susan’s stool test does not seem to indicate any primary gut pathology and it would be unlikely that she would have small intestinal bacterial overgrowth with an entirely normal stool test. Additionally, she still seems to have issues with elevated DHEA-S and other female hormones with progesterone changes after ovulation likely impacting gut motility. Fiber intake, hydration, magnesium supplementation all appear optimal at this time, although she could benefit with the targeted inclusion of certain fibers, changing to magnesium citrate and using DIM or female adaptogens around the second half of her cycle to prevent worsening constipation.
Thyroid function now 7 weeks post stopping medication shows normal free T4 and free T3 with TSH within range and near the previous baseline noted while on thyroid hormone replacement. She does appear to have some immune dysregulation and potential mast cell phenomenon as she has noted some isolated hives and her bloodwork continues to show slightly elevated eosinophils and monocytes. Our next step of action should be to explore female hormone testing to corroborate elevated DHEA-S, assessing estrogen and progesterone metabolism to fine tune and better support female hormones and detoxification.
Additionally, she may benefit from a trial of anti-histamines and quercetin to see if this has any effect with infrequent hives and skin rashes. I do not feel given her overall improvements and the current state of health that further extensive testing is necessary. We can continue with the current plan including the titration off of psychotropic medication, reassessing thyroid function as well as a performing an iron panel in 2 months alongside organic acid testing to optimize nutrition and fetal environment for conception. We will also monitor her during the titration off SSRI, given recent stoppage of thyroid hormone to ensure continued motility. Short term pro-kinetic support with 5-HTP and Vitamin B6 may be explored.
PLAN
New Supplementation
- Explore DIM 300 mg
- Quercetin 3x daily before meals
- Change magnesium glycinate to magnesium citrate
- Explore the use of 5-HTP and Vitamin B6 – pro-kinetic if necessary given titration off SSRI
New Medications
- Can explore the use of anti-histamine as desired.
New Testing
- DUTCH urinary hormone testing
- Repeat targeted blood chemistry in 8-12 weeks
Clinical Commentary
Given the patient’s clinical trajectory, concerns for hormonal imbalances contributing to symptoms and the overall goal of desiring conception in the near future, I feel it is prudent to utilize hormonal and organic acid testing given the importance of optimizing pre-conception environment and her previous health concerns. I do not usually perform such testing in patients at her stage of health and improvement, but I have been using these tests specifically for soon to be mothers with the focus on optimizing essential fatty acid status, assessing for folate or B12 needs, assessing iron status, thyroid function, heavy metal toxic burden, and mineral status, and in this patient’s case, looking for possible low progesterone given the elevated androgens that could make early miscarriage more likely. Despite utilizing more testing than normal in this case, I am still remaining targeted asking very specific questions that have large implications and would change/dictate my medical recommendations.
Final Summary
This is the active substance, name of the drug is Lexapro.
Dr. Ruscio’s Comments:
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!