Practitioner Case Study – January 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Dr. Ruscio’s Review of Zonulin Testing for Leaky Gut
- Re-challenging FODMAPs: The low FODMAP diet phase two
- Rapid-Fire Research – ultra-concise summaries of noteworthy studies.
- Autologous stem-cell transplantation in treatment-refractory Crohn’s disease: An analysis of pooled data from the ASTIC trial
- Selective expression of histamine receptors H1R, H2R, and H4R, but not H3R, in the human intestinal tract.
- Using Hashimoto thyroiditis as the gold standard to determine the upper limit value of thyroid stimulating hormone in a Chinese cohort.
- Blocking nocturnal blue light for insomnia: A randomized controlled trial
Practitioner Question of the Month
Practice Tip
Case Study
Questionable Diagnosis of Hypothyroid by “Famous Thyroid Doctor” Results in Harming Patient Only to Later See Great Results by… Starting With The Gut.
Patient Info:
- Brittany, 33yo female
- Previous Dx
- Hypothyroidism, Epstein–Barr virus, Irregular heartbeat
- Rx
- NA
- Chief Complaints
- Gas, 6-IN
- Bloating, 5-IN
- Fatigue, 4-OC
- Constipation/diarrhea, 8-IN
- Other Symptoms
- Allostatic, mod – fatigue, insomnia
- Female, mod – digestion, cramps
- I am now making a rough tally of how high a patient’s allostatic load and female hormone symptoms appear (mild, mod, severe).
Visit 1 (Day 1) – History and Exam:
Initial Impression
- Intro: Brittany presents as a 33yo female, on a very healthy diet, with a good lifestyle, demeanor, and outlook on her health.
- Dx/Rx: Likely incorrectly Dx with hypothyroid and EBV
- Testing: NA
- Onset/History: Healthy child. IBS 2002-4 until went Paleo. 2015 got very sick with what she thinks was mono, fatigue lasted 1.5 years post.
- Family: AFib, thyroid conditions, anemia
- Tx: See below. Fairly naïve but has responded to what she has done. Other than thyroid Rx, all of which had caused reactions, even after multiple formula and dose changes
- Notes/DDX: Should be a simple case where GI is the main driver, classic IBS/dysbiosis.
- Other: Might also require antiviral/immune support, but not likely.
- Prognosis: Good to excellent.
Previous Diets
- Mg Citrate – helps constipation. Armour – felt worse, levels NR. Thyroid meds (any kind) – negative reactions. Probio – some help, some flare. Habx – up/down. EBV treatment – up/down. Vitamins B, C, and D – very helpful.
Previous Treatments
- Lower Carb, FODMAP and Paleo-like -helps. Low lectin – NR. Low histamine – slight help. AIP – NR. Female hormones best on low carb.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing
- Please send me the labs from before you went on thyroid medication. The labs that diagnosed you as hypothyroid.
- Optional – Aero Lactulose SIBO breath test
- Optional – BioHealth 401H stool test
- PCO testing at LabCorp
- CBC w diff, CMP, lipid panel, iron panel, Hemoglobin A1c, vitamin D
- TSH, free T4
- TPO and TG antibodies
- Rationale
- Prior labs- I now (unfortunately) ask all patients to send me the labs that diagnosed them as hypothyroid if they were diagnosed by any type of integrative or functional provider. You’ll be shocked by what follows in this case.
- GI testing as optional – because she was treatment naïve, she had performed some treatment but it was mostly haphazard, so chances are high by starting with my GI algorithm she won’t need to test.
- PCO testing – I’d like to see her current thyroid hormone and antibody status, and basic blood work
Recommendations
- Diet
- Please continue with your previous Keto, Paleo, low FODMAP
- See handouts at www.drruscio.com/patients
- Lifestyle
- NA
- Treatment
- Sequence: testing, diet & supplement program, follow up.
- NRT: B Complex, C+Biofizz, vitamin D/K
- GI: Lacto-Biff, S. boulardii, Soil-Based, Mg Citrate
- FU: 4 weeks
- Rationale
- Brittany seemed to respond well to therapies she had done in the past but just needed some structure and monitoring. So, we start simple.
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- B Complex, C+Biofizz, Vitamin D/K – helping.
- Lacto-Biff, S. boulardii, Soil-Based, Mg Citrate – helping.
- Improved:
- Bloating, gas (much less). Food Intolerances. Constipation. Insomnia.
- Same:
- Worse:
- Diarrhea (vitamin C).
Lab interpretation:
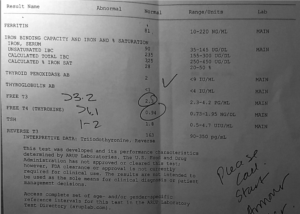
- Labs from time of ‘hypothyroid’ diagnosis (file below)
- WNL – not hypothyroid
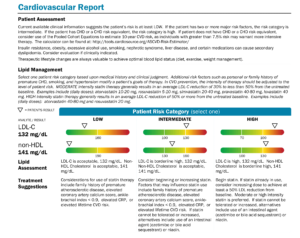
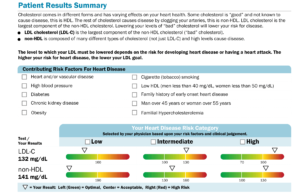
- LabCorp PCO file: Labcorp 11.21.18
- Lipid Panel Cholesterol 220-H, LDL 132-H
- Iron Panel Ferritin 151-H
- Vit D 2-H
- Dx:
- NOT hypothyroid. High ferritin due to inflammation
Impression:
- Today Brittany has improved in almost all CCs. Labs are UR AND prior labs with well-known thyroid doctor showed she was NOT hypothyroid… likely why she felt terrible on Rx. Will continue current plan then fu.
- My rant:
- I try to give every provider the benefit of the doubt. Hopefully, this patient misunderstood her diagnosis, which hopefully was ‘you’re not hypothyroid but your levels are not optimal and might benefit from support’. However, the fact that 1) this patient thought she was true hypothyroid and moreover, 2) was subjected to what I believe was roughly 7 months on different Rxs and felt worse the entire time – make me suspect this was terribly executed functional medicine care.
- What is appalling about this is that a well-known thyroid doctor who has literally written books on the issue and speaks at conferences, etc… Again, hopefully, this was just an isolated incidence, but…. I have seen this erroneous thyroid Dx enough times to think it’s Some of these thyroid gurus might be where all the misdiagnosis is coming from (they are teaching this to other clinicians).
- Finally, if you’re going to perform a trial of thyroid Rx in a case like this, you should look to symptomatic improvement to ensure this was the right choice. Pair this with a recent meta-analysis showing no benefit when treating subclinical hypothyroid with thyroid hormone (SCH is worse than Brittany’s normal labs) and you can help but ask yourself ‘what the heck is going on here?’. This display both ignorance to the literature and a poor ability to leave your dogma at the door and know when someone might not fit into your thyroid-centric model.
Recommendations:
- New
- Discontinue the vitamin D for 6 months, then retest and only use a maintenance dose of 2-6,000 IU/day
- Continue current plan
- FU: 6-8 weeks
Dr. Ruscio’s Comments
Brittany is not done with her care, but I wanted to point out that in only 2 months she has seen better results than she has seen in years. She is also no longer burdened with the thinking she is hypothyroid. You’ve likely heard me say that overdiagnosis/incorrect diagnosis of hypothyroid is a problem and that often times it’s a problem in the gut leading to the symptoms attributed to the thyroid. These cases are why. Don’t make this mistake. I expect her loose stools to improve with a reduction in her vitamin C and that her fatigue will follow the trend of all her other symptoms and improve with time.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine

Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!