Practitioner Case Study – April 2019
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Case study
Research
- Dr. Rusico’s Comparison of Two Popular DNA-based Stool Tests
- Secretome of Intestinal Bacilli: A Natural Guard against Pathologies
- Why Is Working Memory Performance Unstable? A Review of 21 Factors
- Rapid-Fire Research – ultra-concise summaries of noteworthy studies
- Guidelines for the investigation of chronic diarrhea in adults: British Society of Gastroenterology, 3rd edition
Practitioner Question of the Month & Practice Tip
Case Study
From Diarrhea, Gas, Rashes, and Amenorrhea to Symptom-Free and Pregnant In Just Over 6 Months. The Power of Gut & Female Hormone Support and No Need to Directly Treat Low T3.
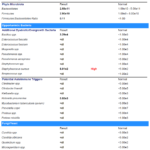
Patient info:
- Kaitlyn, 29yo, Female
- Previous Dx
- IBS, PCOS
- Rx
- N/A
- Chief complaints
- Daily diarrhea (5 years, constant), 9-CO
- Gas, 5-INT
- Skin rash (upper arms), 4-INT
- Amenorrhea (since stopping birth control 7 years ago), 10-CO
Visit 1 (day 1) – History and Exam:
Initial impression:
- Kaitlyn presents as a 29yo female with good diet, lifestyle and outlook on her health.
- She had been on BC for many years and now is not cycling after being off for 7mo. Kaitlyn likely has dysbiosis and very likely is irritated by high FODMAP and insoluble fiber/cellulose intake. She may also have histamine intolerance, or less likely, oxalate or lectin sensitivity, or bile acid malabsorption or IBD.
- Dx/Rx:
- IBS and PCOS and is on no Rx.
- Previous testing:
- Colonoscopy and endoscopy – normal.
- Onset:
- Her female symptoms have been present since puberty and her GI symptoms for several years. Occurring with no known cause.
- Notes/DDX:
- Kaitlyn likely has dysbiosis and very likely is irritated by high FODMAP and insoluble fiber/cellulose intake. She may also have histamine intolerance, or less likely, oxalate or lectin sensitivity, or bile acid malabsorption or IBD.
- Prognosis:
- I anticipate she will respond very well to standard therapies. Prognosis good to excellent.
- Previous Diets:
- Dairy free and paleo seemed to help but is still having GI symptoms. Low FODMAP helps diarrhea but then get constipated. Does better on fewer vegetables and more grain. NR to probio and to Paleo.
- Previous Treatment:
- Test lowering protocol – only 2 weeks. Probios – NR. Aloe – NR.
Visit 2 (a few days later) – Testing and Initial Recommendations
Testing:
- Tests ordered
- Aerodiagnostics Lactulose SIBO breath test
- GI-MAP Stool Test
- Quest #1 – blood, urine, stool, breath – full GI
- Quest #2 – blood, urine – basics + additions
- Rationale
- Her GI symptoms warrant SIBO and stool testing
- Will will also screen via standard blood work for anemia, hypothyroid, high blood sugar, etc…
Recommendations:
- Diet + Lifestyle
- Start on the Standard Low FODMAP Diet. Also, continue to avoid dairy and other foods you know don’t agree with you.
- Make sure to eat more gluten free grains, and less vegetables. Also, eat slightly less fat.
- Give this two weeks, if it has not provided adequate resolution then also try following the Low Histamine Diet for 1 week.
- Please be on the diet for 3 weeks before adding in the supplements, but continue diet until our follow up. Then be on the supplements for 3 weeks before following up. Please make a note of the change you noticed from each one of these.
- Until our follow up, only perform weight training. No high intensity cardio or circuits.
- Treatment
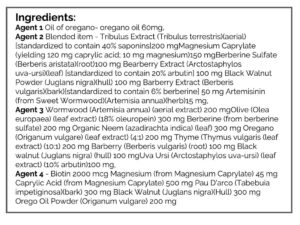
- NRT: Vitamin D/K, DHA/EPA
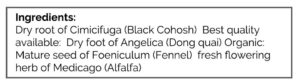
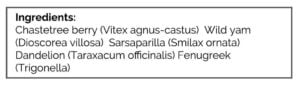
- Cycling Female: Female hormone support herbs
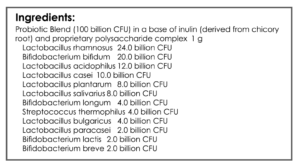
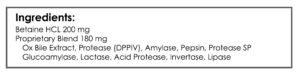
- GI: Lactobacillus & Bifidobacterium probiotic blend, Saccharomyces boulardii probiotic, digestive enzyme
- *Before starting any supplements, perform a 4 day trial on peppermint oil*
- Rationale
- Fairly straight forward choice of diet for IBS-like symptoms
- Same applies for probiotics.
- Her female hormones likely need a push for initiating regular menstruation
Visit 3 – Lab Interpretation and Treatment Evaluation
Subjective Assessment:
- Broth fast (3 days) – helpful
- Standard Low FODMAP diet, less veggies, more carbs – helpful
- Peppermint oil – caused constipation
- Initial program – Has only been doing a few days
- Less exercise – seems helpful
- Improved:
- Diarrhea, gas
- Female – is cycling again
- Same:
- Skin
- Worse:
- Fatigue
Lab interpretation:
- Aerodiagnostics Lactulose SIBO breath test
- H2: 68, rise 62, CH4: 10
- H2: 68, rise 62, CH4: 10
- GI-Map Stool test
- Quest #1 blood, urine, stool & breath
Diagnosis:
- Moderate (68/10) H2 predominant SIBO. GI-MAP: bacterial dysbiosis. Quest: Low Total T3, L vit. D, ASCA antibodies.
Impression:
- 1/31/18
- Today’s labs show SIBO and bacterial dysbiosis, low WBC, total T3 and IBS abs. Kaitlyn has improved nicely from increasing CHO/GF grains via standard LF diet. This combined with less exercise may have lead to cycle returning. Initial program – too early to tell. Today we will continue with current plan and give initial program a few weeks to take effect. Then f/u and decide on maintenance or to use Habx.
Recommendations:
- Diet + Lifestyle
- Continue to focus on weight training. Limit high intensity cardio or circuits.
- Continue on current plan
- Follow up: 4-6 weeks
Visit 4
Subjective Assessment:
- Isn’t feeling as well as she was last time we spoke, partially because she has been less compliant with diet, mainly has more bowels, missed a cycle and rash has reappeared.
- Improved:
- Gas
- Same:
- Better than baseline, but not as good last visit.
- Skin rashes.
- Period has not come back; had one in Nov. and Jan. but not March.
Impression:
- 3/16/18
- Isn’t feeling as well as she was last time we spoke, partially because she has been less compliant with diet, mainly having more bowels movements, missed a cycle, and rash has reappeared. Cycle could require time, diarrhea, rash, and cycles may improve after treating SIBO/dysbiosis. Today starting Habx. Monitor her cycles and if not responsive, retest T3.
Recommendations:
- Continue current plan
- Starting:
- HAbx base protocol
- Follow up: 5 weeks
Visit 5
Subjective Assessment:
- Is about the same, better than baseline, but improvements have plateaued.
- Bad days are much better than baseline, but are not as good as she’d like them to be.
- Habx (1st month base) – NR.
- Improved:
- Gas
- Cycles: had period in March
- Same:
- Bowels – better than baseline, but not as good as last visit
- Skin
Impression:
- 4/25/18
- Better than baseline, but still not optimal. Time might be required, but will finish Habx today, tweak diet, and stop enzymes. Next consider a low histamine diet.
Recommendations:
- Continue:
- Habx base protocol
- Starting
- Consider rotation diet, look at foods restricted on the AIP to be cautious with.
- Or try full trial for 2 weeks on AIP, Autoimmune Paleo Diet
- Discontinue Digestive Enzyme
- Follow up: 3 weeks after finishing antimicrobials
Visit 6
Subjective Assessment:
- Just finished Habx. 2nd month antimicrobials – likely helpful
- AIP, low FODMAP (2 week trial) – very helpful.
- Was able to reintroduce nuts, grains but might have a problem with nightshades, coffee – still experimenting.
- When follows AIP+LF at home = 100% improved, when AIP+LF out = 80%.
- Improved:
- All GI complaints markedly improved
- Skin
- Cycles: is now getting cycles (though they are long around 55 days)
Impression:
- 6/27/18
- Today Kaitlyn has improved to a point where she peaks at 100% improvement, but only when eating home cooked AIP+LF diet, which she recently started. 2nd month of Habx may have helped also. Reports she does not eat much dietary histamine, so low HI not advised. Today, decided to maintain current course (including AIP+LF) and start on trial of Immunoglobulins. Next consider: low sulfur, Elemental Diet, Low Dose Naltrexone, Helminth Therapy, Bile Acid Malabsorption.
Recommendations:
- Ending:
- Habx base protocol
- Continue:
- Continue on the AIP + Low FODMAP diet
- Starting:
- Begin trial of Immunoglobulins for 3-4 weeks
- GI (Diarrhea, IBS-D): Immunoglobulins
- Follow up: 4-6 weeks.
Visit 7
Subjective Assessment:
- Currently pregnant. Stopped taking everything and started on prenatal.
- Before that, everything was going very well.
- SBI (one bottle, 3-4 weeks) – thinks it helped, hard to say.
Impression:
- 8/15/18
- Today Kaitlyn is pregnant and very pleased about this given she had been amenorrheic before we started our work together. AIP+LF diet continues to keep her asymptomatic, Immunoglobulins may have helped. Today will continue only with vitamin D/K, DHA/EPA, and probiotics. Also, recommending to continue monitoring with OB, consider also finding midwife and being diligent about iodine intake given she is on paleo diet. Will also start dietary reintro. Will f/u as needed or if any thyroid (SCH) questions arise.
Recommendations:
- Stop the following until you are done nursing: Female hormone support herbs, DHA/EPA, Immunoglobulins.
- A low FODMAP diet can help reduce colic when nursing.
- Make sure you are getting in adequate dietary iodine (Anywhere 220-290 mcg per day.)
- Start on dietary reintroductions
- Follow up as needed
Testing
- TSH, free T4, free T3, TPO and TG antibodies
Dr. Ruscio’s Comments
This is case beautifully illustrates the powerful effect you can have on fertility via improving gut health combined with herbal female hormone support.
We could have rushed into a month long female hormone profile – not needed.
We could have said ‘you must be on thyroid hormone if you want to get pregnant’ – not needed. But, we should make sure her OB is aware of this finding and monitoring thyroid function.
We focused on her diet, GI health and used some gentle herbal female hormone supports and Kaitlyn did great. She wasn’t perfect from a GI perspective, but thankfully she hit her goal of becoming fertile, we will later return to our process of GI optimization. I also suspect she was 90% of the way there after the Habx, and just needed a little time for her GI to heal and thus for further symptomatic improvements to be realized.
Also, if I were starting with Kaitlyn today I likely would have ordered less GI testing. With the clinically hierarchy I use for GI, most findings become irrelevant thus making the need for copious documentation of dysbiosis or infection moot. My care becomes less expensive, patients like this, they tell friends, my practice grows. This is cost-effective functional medicine!
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine


Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!