Practitioner Research Review – March 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Effective vitamin B12 treatment can reduce serum antigastric parietal cell antibody titer in patients with oral mucosal disease.
https://www.ncbi.nlm.nih.gov/pubmed/27474730
Study Purpose:
- To assess the impact of B12 administration on stomach autoimmunity (anti-parietal cell antibodies). This was a follow up to a previous study by this same group, http://www.ncbi.nlm.nih.gov/pubmed/20659263 . These cells are responsible for producing stomach acid and for absorption of B12, so the clinical implications are significant.
Intervention:
- 210 patients were given either
- One B12 injections per week as 1,000 mcg hydroxocobalamin.
- Oral B12/vitamin blend. 1 capsule twice per day. Each capsule contained:
- 10 mg of vitamin B1, 5 mg of vitamin B2, 5 mg of vitamin B6, 5 mcg of vitamin B12, 20 mg of calcium pantothenate, 50 mg of nicotinamide, 150 mg of vitamin C, and 60 mg of calcium.
- Note: this equals 70 mcg per week of oral B12
Main Results:
- B12 injection group
- “We found a significant drop of the positive antibody rate from 100% to 42.9%”
- Oral B12 group
- Antibody “titers increased to significantly higher levels”
Additional Results:
- Maintenance vitamin B12 injections once a month could retain remission of antibodies in 87% of patients compared with 10% in those without vitamin B12 injections.
Authors’ Conclusion:
- Vitamin B12 injections can reduce higher serum anti-parietal cell antibody titers to significantly lower or undetectable levels.
Interesting Notes:
- Roughly 30% of patients with parietal cell antibodies also have thyroid antibodies.
- The following symptoms were reported by patients with parietal cell autoimmunity:
- Burning sensation in the mouth 98%
- Dry mouth 80%
- Sore tongue 60%
- These are good symptoms to add to your paperwork as a prompt for testing these antibodies.
- B12 did not affect thyroid autoimmunity in those with pre-existing thyroid autoimmunity.
- “We also found that patients with higher titers needed longer periods of vitamin B12 injection treatment to achieve complete response.”
Clinical Takeaways:
- Vitamin B12 injections can arrest stomach autoimmunity. Those with oral burning, dry mouth, and/or sore tongue are at increased risk for stomach autoimmunity.
Dr. Ruscio’s Comments:
This study is very exciting. It reinforces previous findings from this group that B12 injections can arrest stomach autoimmunity. This study also showed that oral B12 did not have this effect. After weekly injections until the antibodies are normal, the results can be maintained by once monthly injections. This therapy could potentially preserve the health of stomach tissue and therefore prevent loss of the ability to produce hydrochloric acid and intrinsic factor.
How to Test and Treat Small Intestinal Bacterial Overgrowth: an Evidence-Based Approach.
https://www.ncbi.nlm.nih.gov/pubmed/26780631
Study Purpose:
- To review the available evidence regarding SIBO treatment and to offer an evidence based treatment approach.
Intervention:
- N/A
Main Results:
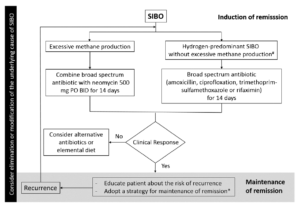
- Here is their proposed management strategy:
Additional Results:
- See below
Authors Conclusion:
- See below
Interesting Notes:
- “Multiple independent risk factors have been identified for SIBO including [4]: (1) anatomical abnormalities such as small intestinal diverticulosis; (2) postsurgical structural changes such as ileocecal valve resection, gastric bypass, and Roux-en-Y; (3) medications that slow the gut motility such as narcotics, anticholinergics, and anti-diarrheals; (4) hypo- or achlorhydria due to surgery, autoimmune gastritis, or proton pump inhibitors [5••, 6]; and (5) small bowel dysmotility irrespective of the cause (e.g., inflammatory bowel disease, celiac disease, radiation enteritis, small bowel adhesions, and systemic diseases associated with dysmotility such as scleroderma, diabetes, and amyloidosis) [5••, 7].”
- Note: we just discussed B12’s effect on autoimmune gastritis.
- “SIBO has been associated with multiple conditions including irritable bowel syndrome [8], rosacea [9], hepatic encephalopathy [11, 12], obesity [13], gastroparesis [14], Parkinson’s disease [15], fibromyalgia [16], chronic pancreatitis [17], end-stage renal disease [18], and inflammatory bowel diseases [19].”
- Note: this shows the following connect to the gut: skin, liver, metabolism, brain, and pancreas.
- Gastrointestinal symptoms may not always predict SIBO.
- “Human cells are not capable of producing methane or hydrogen gas [23]. The presence of these gases in the human breath signifies the metabolism of carbohydrate residues by gut, their absorption from the gut, and expiration through lungs.”
- “those with excessive methane production are five times more likely to have constipation [26]. Moreover, the severity of constipation directly correlates with the methane level [27].”
- “Although not fully validated, currently, the accepted gold standard for diagnosis of SIBO is the aspiration of small bowel fluid, followed by culture and bacterial count. Proximal small bowel culture may be falsely negative as it can miss overgrowth of bacteria in the mid and distal small bowel.”
- “In a meta-analysis of 10 placebo-controlled trials, antibiotics were shown to be superior to placebo with a combined normalization rate of 51 % for antibiotics compared with 10 % for placebo.”
- Two studies have shown neomycin along with Rifaximin to be more effective for methane SIBO than Rifaximin alone:
- “Based on this, we advocate 2 weeks of therapy with neomycin and rifaximin for treatment of patients with methane-predominant bacterial overgrowth.”
- Note: the term predominant, meaning neomycin may not be needed just because methane is above 3ppm. It may only be needed when methane is the predominant
- “Elemental diets may be an extremely safe and effective alternative to antibiotics.” One study found an 80-85% response rate to elemental diets.
- Herbal antibiotics showed a 46% normalization rate of SIBO breath testing according to one study.
- “Lauritano et al. [45] showed that 13, 28, and 44% of SIBO patients experience a relapse of their symptoms and breath test positivity at 3, 6, and 9 months.”
- There are 2 classes of prokinetics, which are considerations in preventing relapse of SIBO:
- “motilin receptor agonists (e.g., erythromycin and azithromycin) and
- 5-HT4 agonists (e.g., tegaserod, cisapride, and prucalopride).”
- Note: The one study looking at this found that tegaserod extended time in SIBO remission. However, erythromycin did not show a statistically significant benefit. This is important to bear in mind and suggests potentially we are overstating the effect of erythromycin. Which is why this study concluded, “Tegaserod significantly prevents the recurrence of IBS symptoms after antibiotic treatment compared to erythromycin or no prevention.”
- “In a systematic review, Rao et al. [55] found that a low FODMAP diet improved overall IBS symptoms in 6/6 trials”
Clinical Takeaways:
- Antibiotics, herbals, elemental diet, and low FODMAP diets are all efficacious treatments for SIBO and/or IBS.
- SIBO has been associated with many non-gut conditions/symptoms.
- Neomycin may not be needed just because someone has methane positivity, but may be best reserved for when methane is
- The SIBO relapse preventative effects of erythromycin may be overstated.
Dr. Ruscio’s Comments
Most of my comments on this study were provided in the clinical takeaways. However, one thing that was disappointing was the short and incomplete mention of probiotics. A handful of clinical trials have shown that probiotics can reduce SIBO gas levels. Several clinical trials have shown probiotics to benefit IBS. I fear there may be a bit of an anti-probiotic biased present here. Other than that, this was a great review of available SIBO treatment/prevention options.
Helicobacter pylori CagA antibodies and thyroid function in latent autoimmune diabetes in adults.
https://www.ncbi.nlm.nih.gov/pubmed/27775795
Study Purpose:
- “determine the association between H. pylori infection and its virulent strain CagA with antibodies against thyroperoxidase (TPO Ab) and thyrotropin (TSH) in a cohort of latent autoimmune diabetes in adult (LADA) patients.”
Intervention:
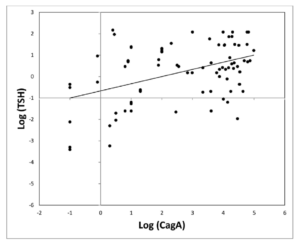
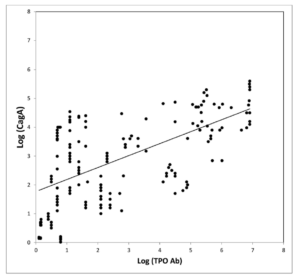
- “We included 234 LADA patients (53.8% women). Antibodies against H. pylori whole antigens and CagA, TPO Ab and TSH were assessed in all patients.”
Main Results:
- Prevalence of IgG against H. pylori and CagA was 52.1% and 20.9% respectively.
- Antibodies against H. pylori were not associated with TPO Ab and TSH.
- Antibodies against CagA showed a positive association with TSH and TPO Ab.
- Subjects with hypothyroidism (TSH ≥ 3.5 μU/ml) had an increased frequency of Ab anti CagA .
Additional Results:
- Other studies showing an association between HP and thyroid autoimmunity
- Studies showing treatment of HP can reduce thyroid AI
- **Meta-analysis showing association between H. Pylori and thyroid autoimmunity
Authors’ Conclusion:
- “We showed that titers of TPO Ab and CagA were related, suggesting that the presence of most virulent pylori could be a risk factor for the presence of thyroid autoimmunity and a functional impairment of the thyroid gland.”
Interesting Notes:
- “Latent autoimmune diabetes in adults (LADA) is a type of autoimmune diabetes characterized by the presence of antibodies against glutamic acid decarboxylase 65 (GAD65 Ab) with a clinical picture very similar to type 2 diabetes at diagnosis.”
Clinical Takeaways:
- CagA H. Pylori and HP in general are associated with thyroid autoimmunity. Treatment of HP may improve thyroid autoimmunity.
Dr. Ruscio’s Comments
This study provides some nice documentation for the gut-autoimmunity connection as it relates to HP. It appears that HP in general may be associated with thyroid autoimmunity and that CagA HP might be more strongly associated.
Does this mean all autoimmune thyroid patients should be screened for HP? Well, maybe. The data here are not complete in the sense that we don’t know that treating this finding will yield any clinical benefit. If one could perform a screening at a reasonable cost, I think this is much more justifiable. Most of the studies looked at HP stool antigen for serum antibodies.
Regarding treatment of HP: I don’t think we have strong enough data to suggest triple or quadruple therapy for HP is justified in non-symptomatic (digestively) autoimmune thyroid patients. However, natural treatment options may be a justifiable alternative for this group. Anti-microbial herbs, paired with probiotics and potentially NAC, carry extremely low adverse effects and even have secondary health benefits.
To state this simply: if someone has HP and the classic GI symptoms that it causes (ulcer, indigestion, reflux) – treat via any of the available options. If someone has no GI symptoms but has thyroid AI, consider a natural treatment option.
Solar radiation and the incidence and mortality of leading invasive cancers in the United States.
https://www.ncbi.nlm.nih.gov/pubmed/27195056
Study purpose
- To assess the relationship between level of ultraviolet light exposure and invasive cancers
Intervention:
- The North America Land Data Assimilation System (NLDAS) daily average sunlight for the continental United States from 1999–2011 was analyzed in relation to the US Cancer Statistics age-adjusted-incidence and mortality from the Centers for Disease Control and Prevention (CDC).
Main Results:
- Cancer incidence
- “We found associations between increasing solar energy and decreasing cancer incidence for: all invasive cancers, brain/nervous system cancer, breast cancer, colon/rectum cancer, corpus uteri cancer, esophageal cancer, larynx cancers, leukemias, non-Hodgkins lymphoma, ovarian cancer, prostate cancer, and urinary bladder cancer.”
- “We found associations between increasing solar energy and increasing cancer incidence for: cervix uteri cancer and liver cancer.”
- We found no associations between solar energy and melanoma.
- Cancer mortality
- “We found no association between increasing solar energy and decreasing cancer mortality for all invasive cancers.”
- “We found that increasing solar energy increased liver cancer mortality.”
- We found no associations between solar energy and melanoma.
Additional Results:
- N/A
Authors’ Conclusion:
- “In summary, the current study confirms other ecological studies relating solar radiation to the incidence and mortality of a variety of cancer types.”
Interesting Notes:
- The method used to assess solar radiation in this study is likely more accurate than latitude because it accounts for factors such as cloud cover, ozone levels, and altitude.
Clinical Takeaways:
- Reasonable sun exposure may promote health.
Dr. Ruscio’s Comments
This study essentially found that living in a location with increased UV exposure was correlated with a decreased incidence of most, but not all, invasive cancers. What is more interesting is that the invasive form of skin cancer, melanoma, did not increase in incidence nor mortality with increased UV exposure. This study supports a growing body of evidence that suggests reasonable sun exposure may improves one’s health and that strict sun avoidance may have unintended health consequences.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!