Practitioner Research Review – August 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
In Today’s Issue
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
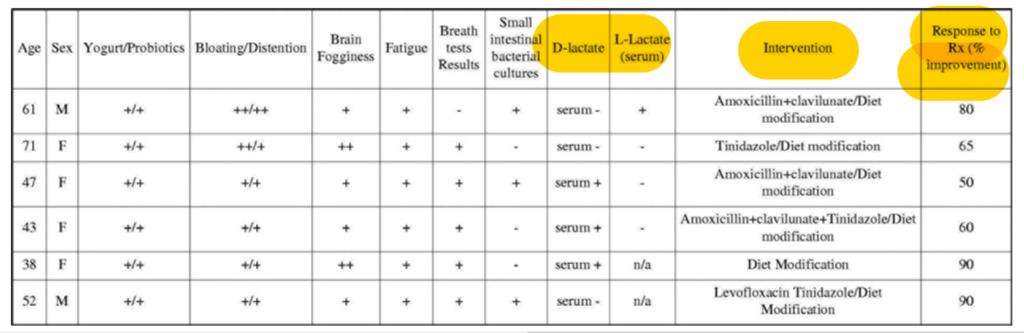
Brain Fogginess, Gas, Bloating and Distension: A Link Between SIBO, Probiotics and Metabolic Acidosis
http://www.gastrojournal.org/article/S0016-5085(14)63089-4/pdf
Study purpose:
- To assess the relationship between brain fog, SIBO, and probiotics.
Intervention:
- Patients who had been experiencing bloating and distension associated with brain fog for more than 1 year were assessed.
- Symptoms, glucose SIBO breath test, and duodenal aspirate culture for SIBO were all assessed.
- Serum or urine D-lactate and/or L-lactate were assessed after a carbohydrate challenge.
Main Results:
- 5 of the 6 patients had SIBO.
- All patients reported bloating and brain fogginess/spaciness and fatigue.
- All patients had a history of yogurt consumption, and 2/6 consumed large amounts of homemade yogurt. All took regular probiotics.
- Antibiotics resolved symptoms in 5/6 patients.
Authors’ Conclusion:
- “We found a significant association between probiotics, SIBO, d-lactic acidosis, GI symptoms and brain fogginess/fatigue in all 6 patients.”
Interesting Notes:
- “Lactobacilli tend to be resistant to antibiotics and cause d-lactic acidosis by fermenting carbohydrates in the food. The high lactate levels detected in our subjects explains their neuropsychological symptoms.”
Clinical Takeaways:
- Those with bloating accompanied by brain fog may have SIBO. In these patients, high consumption of probiotics or probiotic rich foods may cause high levels of D- and L-lactate, thus causing brain fog.
- This can be ameliorated by avoidance of probiotics, carbohydrate restriction (including FODMAPs), and antimicrobial therapy.
Dr. Ruscio’s Comments
- D- or L-lactic acidosis is rarely reported in adults, but SIBO is a condition that increases risk. When combining SIBO with a high intake of probiotics and/or probiotic rich foods, the risk could increase even more. It’s important to note that these are patients who had been in this pattern of bloating with brain fog for over 1 year, suggesting they had been subjected to high levels of probiotic intake for a while. Because probiotics can treat/kill SIBO, there is a group who will see SIBO (bloating) and brain fog improve after taking probiotics. However, for those who see no improvement or perhaps even worsen (most common reaction to probiotics is bloating in my observation), probiotics may not be a good idea. By simply monitoring someone’s response and not being dogmatically pro- or anti-probiotics, this can be easily navigated in the clinical setting. If someone responds well – continue with probiotics. If there is a negative reaction – stop probiotics.
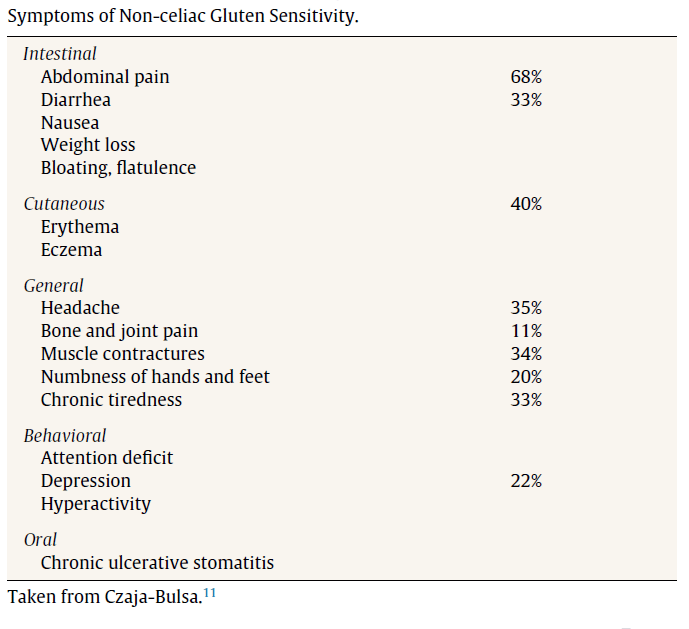
Non-celiac Gluten Sensitivity and Rheumatic Diseases
https://www.ncbi.nlm.nih.gov/pubmed/25956352
Study purpose:
- To examine the connection between NCGS and rheumatic conditions (fibromyalgia, spondyloarthritis, and autoimmune).
Intervention:
- A review of cases at the authors’ center.
Main Results:
- “The findings that point to the presence of NCGS are
- Severe asthenia (weakness and fatigue),
- Oral aphthae (canker sore),
- Associated gastrointestinal symptoms, and
- Having a relative with CD.”
- Fibromyalgia
- 36% of patients experienced a clinical improvement on gluten-free diet (90 patients in a group of 246).
- “Clinical improvement was defined as achieving at least one of the following objectives: remission of FM, return to work or to normal life, or the discontinuation of treatment with opioids.”
- “The mean follow-up time was 16 months.”
- The following symptoms were most suggestive of NCGS:
- Aphthous stomatitis (canker sores), diarrhea predominant IBS, iron anemia.
- 36% of patients experienced a clinical improvement on gluten-free diet (90 patients in a group of 246).
- Spondyloarthritis (arthritis of spine and sometimes joints of arms and legs)
- 4 cases are presented. Here is the summary:
- All were negative for celiac.
- All improved from a GF diet.
- All (3 of 4) who reintroduced gluten experienced a symptomatic relapse. The fourth person never attempted a reintro.
- 4 cases are presented. Here is the summary:
- Autoimmune
- A number of cases all having one or more various autoimmune conditions.
- An array of symptoms were reported, including joint pain, fatigue, and skin lesions.
- All cases responded to a gluten-free diet. All who later tried reintroducing gluten saw their symptoms worsen. All were negative for celiac.
Authors’ Conclusion:
- “These clinical observations of NCGS associated with systemic diseases, in which it may take months for the benefits of the diet to be noted, differ from the accepted ideas about NCGS, in which it is considered to be a nonautoimmune condition, in which the clinical response to the GFD can easily be observed in a matter of a few days or weeks.”
Interesting Notes:
- “CD can be present in the absence of gastrointestinal symptoms; in fact, nearly half of the CD patients diagnosed in adulthood do not have relevant gastrointestinal symptoms.” This includes mental fatigue and chronic musculoskeletal pain.
- The other autoimmune diseases celiac is most associated with are autoimmune thyroid disease and Sjögren’s syndrome.
- “NCGS is estimated to affect around 5% of the population.”
- Only half of those with NCGS have the celiac genes.
- “With respect to HLA, only about half the patients with NCGS carry DQ2.5 or DQ8”
- A survey by Busta of 347 NCGS patients found the following prevalences of symptoms:
- 14% of those with NCGS have an associated autoimmune condition, according to a 2014 study:
- This same study found that patients symptomatically improved in spite of often maintaining antibody positivity.
Clinical Takeaways:
- A gluten-free diet may benefit a number of rheumatic and autoimmune conditions.
- It may take months for the full effect to be realized, although some improvement should be noticed within the first month.
- The symptoms most suggestive of NCGS are:
- Severe asthenia (weakness and fatigue),
- Oral aphthae (canker sore),
- Associated gastrointestinal symptoms, and
- Having a relative with CD.
- A symptomatic relapse in improvements is almost always noted upon reintroduction.
- Antibody testing may not track with clinical response.
Dr. Ruscio Comments
The clinical takeaways sum up the important pieces here. It is important to keep in mind that it may take months for the full effect of gluten elimination to be noted, but some response is seen within the first 30 days. Also, keep in mind that relapse occurs upon reintroduction. So this suggests a practical approach: eliminate gluten, and if you feel better, stick with it. If one has NCGS, they should have an apparent relapse in symptoms upon reintroduction.
Also, remember that NCGS can manifest solely as non-digestive symptoms.
Iodine and thyroid function
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4049553/
Study purpose:
- “This paper reviews the physiologic role of iodine, methods to assess iodine nutrition, clinical implications of iodine deficiency or excess, and iodine-related thyroid problems in the Korean Peninsula.”
Intervention:
- A review of the literature.
Main Results:
- Iodine insufficiency during pregnancy and infancy caused impaired neurological development.
- Iodine insufficiency during development may cause a permanent skewing of TSH and T4, even after iodine has been repleted.
- “In a longitudinal study, persistent decreases in TSH and increases in free T4 were observed in a previously iodine insufficient population, even though the present iodine status was adequate, suggesting that low iodine intake at young age leads to thyroid autonomy that persists despite normal iodine intake later in life (36).”
- High iodine intake is often harmful for those with thyroid autoimmunity and may induce thyroid autoimmunity or dysfunction.
- “High iodine intake is associated with autoimmune thyroid disease (34).”
- “A sudden increase in iodine intake in an iodine deficient population may induce thyroid autoimmunity (42).”
- “People with anti-thyroid antibodies have a higher risk of developing thyroid dysfunction when the iodine intake is high (43).”
- Iodine intake may not affect thyroid cancer risk.
- “The overall incidence of thyroid carcinoma in populations does not appear to be influenced by iodine intake (44).”
- While insufficient intake in children is harmful, high intake of iodine in children is also harmful.
- “Excessive iodine intake in children in high iodine areas is associated with impaired thyroid function (45).”
- In this Korean sample, increased iodine intake caused increased TSH and decreased free T4.
- “In a study of 337 healthy South Korean adults, UI excretion had a weakly negative correlation with free T4 and showed a positive trend with TSH, whereas their levels of free T4 and TSH were within the normal ranges (48).”
Additional Results:
- Thyroglobulin (Tg), not to be confused with thyroglobulin antibodies (TgAbs), is a sensitive marker of iodine deficiency. Tg will increase in deficiency.
- “In areas of iodine deficiency, serum Tg increases due to greater thyroid cell mass and TSH stimulation. Serum Tg is well correlated with the severity of iodine deficiency (26).”
Authors’ Conclusion:
- “Both iodine deficiency and iodine excess are associated with an increased risk of thyroid disorders.”
Clinical Takeaways:
- Iodine balance is key. More is not better. See the following posts for more:
Dr. Ruscio’s Comments
The most striking note from this paper was the suggestion that excessive iodine intake in children may result in permanent skewing of TSH and free T4. This finding should prompt cautiousness in nutrition recommendations to mothers. Caution should be to not assume ‘more is better’ with iodine intake while pregnant and for infants.
The finding of thyroglobulin was also interesting. I am not sure if this is clinically relevant at this point. I say this because this is the first time I have heard Tg suggested as a marker to monitor iodine insufficiency. It is well known that when thyroid mass increases, so does Tg. Accordingly, I have heard of its use in monitoring thyroid cancer, but not in iodine status. I remain open but skeptical on Tg for assessing frank iodine deficiency.
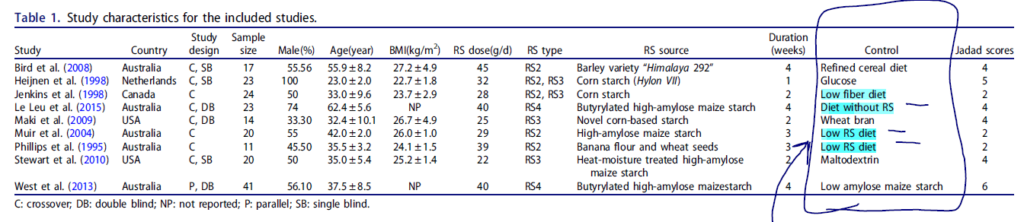
Positive effects of resistant starch supplementation on bowel function in healthy adults: a systematic review and meta-analysis of randomized controlled trials.
https://www.ncbi.nlm.nih.gov/pubmed/27593182
Study purpose:
- To assess effect of resistant starch (RS) on bowel function.
Intervention:
- Systematic review and meta-analysis of randomized controlled trials to evaluate the relationship between resistant starch supplementation and large intestinal function.
- 9 studies were included in this analysis.
- 33 grams/day was the average dose. Different types and dosages of RS were used.
- Note: in my opinion, many of these studies used a poor control – a low RS or low fiber diet. A better control would be a normal diet with normal levels of RS and/or fiber. By comparing the intervention to a low fiber or RS diet, you falsely increase the effect of the intervention.
Main Results:
- The pooled findings revealed that resistant starch significantly increased fecal wet weight and butyrate concentration. Also, RS significantly reduced fecal pH.
- There was a non-significant increase in defecation frequency of 0.04 stools/d.
Additional Results:
- Adverse events were only reported in 3 of the 9 studies.
- Lower doses appear to have a lower incidence of adverse events; 25 grams/day or less may be least prone to cause reactions.
Authors Conclusion:
- “Our study found that resistant starch elicited a beneficial effect on the function of large bowel in healthy adults.”
Clinical Takeaways:
- Resistant starch supplementation likely functions similar to fiber supplementation, which increases stool weight, SCFAs, lowers pH, and may aid in constipation. Lower doses (<25grams/day) are less likely to cause negative reactions.
- Caution may be warranted as it appears possible that internet claims are not reflective of what the clinical outcome studies support.
Dr. Ruscio Comments
Theoretically, increased SCFAs (short chain fatty acids) should reduce colon cancer risk, but this doesn’t appear to be the case. See my book preview wherein I review the evidence regarding fiber, RS, and health (including colorectal cancer) here, https://drruscio.com/dr-ruscios-book-preview-all-about-fiber/.
Someone from our audience did share this reference, stating it contains much support showing numerous health benefits of RS, https://resistantstarchresearch.com/clinical-research-summary/resistant-starch-clinical-list/. I intend to review this evidence and report back once I do. I am open, but admittedly skeptical, because I anticipate I would have come across more data supporting RS already if there was actually high quality data out there.
I am open regarding RS, but I am also cautious. In my observation, those with the more severe GI disease/dysfunction are most likely to experience negative side effects/consequences with the use of RS and with prebiotic supplementation.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!