Practitioner Research Review – April 2017
Dr. Michael Ruscio’s Monthly – Future of Functional Medicine Review Clinical Newsletter
Practical Solutions for Practitioners
Research
*Please note: the case study and research studies are not meant to be mutually reinforcing. There is often concept overlap, however the research studies are a collection of the most clinically meaningful research that has been published recently.
Use of probiotics to correct dysbiosis of normal microbiota following disease or disruptive events: a systematic review.
https://www.ncbi.nlm.nih.gov/pubmed/25157183
Study Purpose
- To summarize all the available data regarding probiotics’ ability to normalize dysbiosis.
Intervention:
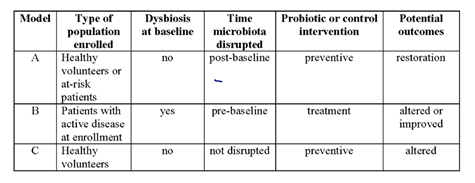
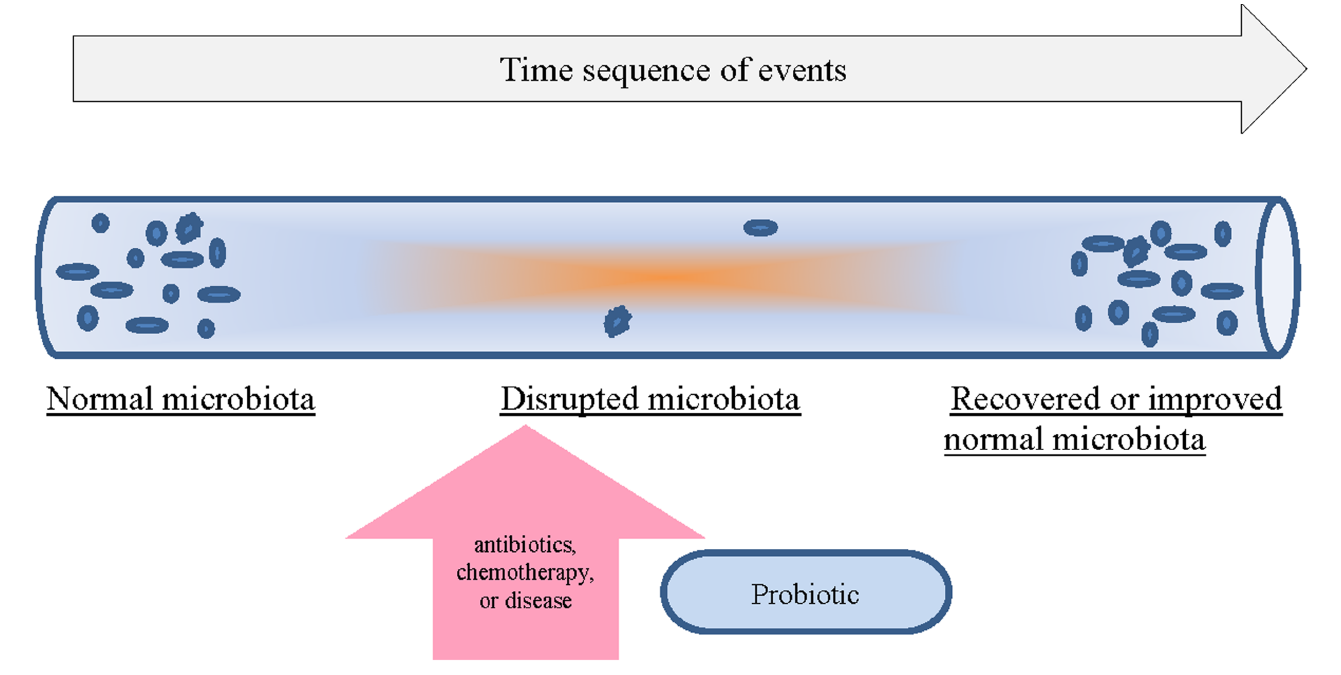
- 63 trials were examined, which looked at probiotics used in three different models.
- Model A (restoration): which assayed patients enrolled with a healthy, undisturbed microbiota, and then assayed them again after a disruptive event (such as antibiotic exposure) and probiotic therapy occurred.
- Model B (alteration): assayed patients with pre-existing disrupted microbiota (e.g., pre-existing chronic disease or active disease) and then post-probiotic therapy.
- The types of pre-existing factors that disrupted the microbiota included atopic dermatitis patients, allergies, cirrhosis, bacterial vaginosis, irritable bowel syndrome, inflammatory bowel disease (ulcerative colitis and pouchitis), idiopathic diarrhea, enteral feeding, short-bowel syndrome, and colon cancer.
- Model C (no dysbiosis): assayed volunteers with no disruptive event (before or during the clinical trial) at both pre-probiotic and post-probiotic times.
- “‘Recovery’ of the normal microbiota is defined as a restoration of the microbiota back to a normal healthy baseline.” Or, to that of healthy controls if subjects had dysbiosis at baseline (typically from disease).
Main Results:
- From a total of 63 trials,
- 83% of the probiotic products using model A restored the microbiota,
- 56% using model B improved the microbiota, and
- 21% using model C had any effect on microbiota.
- Clinical efficacy was more commonly associated with strains capable of restoration of the normal microbiota.
Additional Results:
- “… it became obvious that those probiotics with a greater ability to restore the microbiota are associated with the strongest strength of clinical efficacy.”
- “Of the seven probiotics with associated RCTs, only two probiotics (S. boulardii and L. acidophilus) have strong evidence for efficacy across most of the disease indications.”
- This study did examine results of soil based/spore forming probiotic, Bacillus clausii, however there is not as much data here as for other probiotics.
Authors’ Conclusion:
- “The ability to assess the degree of dysbiosis improvement is dependent on the enrolled population and the timing of microbiological assays. The functional claim for correcting dysbiosis is poorly supported for most probiotic strains and requires further research.”
Interesting Notes:
- About ½ the studies used single strain probiotic, about ½ used multi-strain probiotic.
- A mixture of traditional culture and non-culture (rRNA, PCR) techniques were used to assess the microbiota.
Clinical Takeaways:
- Probiotics may be able to improve the microbiota. Those which produce the best clinical response are the ones most likely to have a positive impact on the microbiota.
Dr. Ruscio’s Comments
There are many criticisms that could be made of this study, in large part because studying the microbiota is a very complex issue: how do we define a healthy MB, what testing methodology is used, how do we define ‘reestablishment of a healthy MB’, and so on.
We could also get lost in meticulous detail analyzing the subtle differences one probiotic has upon the MB compared to another. However, I would not advise it. There is one simple yet profound observation from this study that has notable clinical relevance…. The probiotics that produced the best clinical outcomes had the most favorable impact on the microbiota.
This can be interpreted two ways:
- (Non-cost effective FM) test the microbiota at baseline, then treat with a probiotic, then keep retesting and trying different probiotics until your retest results show the most favorable shift in the MB. Oh, and hopefully this will correlate with an improved patient sitting in front of you.
- (Cost effective FM) experiment with a few different probiotic formulas until you find one (or more than one) that produces the best clinical result. Then assume you have had a favorable impact on the microbiota because the patient in front of you is healthier. Oh, and save hundreds to thousands on testing/retesting.
Option 2 is the obvious choice, especially when we consider we are still not completely sure what a ‘healthy MB’ is and what the best method of assessment of the MB is.
The Unintended Consequences of a Gluten-Free Diet.
https://www.ncbi.nlm.nih.gov/pubmed/28166100
Study Purpose
- To assess if those on a gluten-free diet are at risk of heavy metals toxicity from consuming gluten-free foods that might be higher in heavy metals.
- “Commercial gluten-free products primarily contain rice flour as a substitute. Emerging evidence suggests rice-based products can contain high levels of toxic metals; rice is a recognized source of arsenic and methylmercury exposure.”
Intervention:
- “We used 2009-2014 nationally representative data from the National Health and Nutrition Examination Survey (NHANES) to analyze cross-sectional associations between self-reported gluten-free diet status and urinary and blood biomarkers of exposure to toxic metals.”
Main Results:
- Persons following a GFD had significantly increased total blood
- mercury, lead, and cadmium.
- Urine samples from subjects on a GFD had higher concentrations of total
Additional Results:
- N/A
Authors’ Conclusion:
- “To our knowledge, this is the first analysis to suggest that Americans on gluten-free diets may be exposed to higher levels of arsenic and mercury.”
Interesting Notes:
- See my comments below
Clinical Takeaways:
- If you or your patients hear about this study, rest assured there is no cause for alarm when you get past a catchy title/conclusion and actually look at the numbers.
Dr. Ruscio’s Comments
Here is what you need to know: there is a difference between statistically significant and clinically meaningful. While follow up research on this issue might be interesting, the actual results here are not cause for alarm, in my opinion. When you look at the numeric difference for a given heavy metal, between GF and non-GF dieters, in the context of the reference range, it is clear to see there is little cause for alarm.
For example, a 0.44 difference in blood mercury content when the range in 0-14.9 is not clinically meaningful. This information could be misrepresented to fear people into thinking they need detox therapy when they do not.
- Persons (with celiac) following a GFD had significantly increased total blood
- mercury (1.37 mcg/L) compared with persons not on a GFD (0.93 mcg/L) (P=.008),
- lead (1.42 mcg/L vs 1.13 mcg/L; P=.007), and
- cadmium (0.42 mcg/L vs 0.34 mcg/L; P=.03).
- Reference range for
- Mercury 0.0−14.9 μg/L
- Lead 0−19 μg/dL
- Cadmium 0.3−1.2 μg/L
- Urine samples from subjects on a GFD had higher concentrations of total
- arsenic (15.15 mcg/L) than urine samples from subjects not on a GFD (8.38 mcg/L) (P=.002).
- Reference range
- Arsenic – total arsenic: 0−50 μg/L, 0−50 μg/24 hours; inorganic arsenic: <20 μg/L
- People without celiac disease on a GFD (n=101) had significantly increased blood concentrations of
- total mercury (1.40 mcg/L) vs (0.93 mcg/L; P=.02),
- lead (1.44 mcg/L vs 1.13 mcg/L), and
- higher urine concentrations of total arsenic (14.69 mcg/L, vs. 8.32 mcg/L,).
Repeat Treatment With Rifaximin is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome.
https://www.ncbi.nlm.nih.gov/pubmed/27528177
Study Purpose
- Randomized, double-blind, placebo-controlled trial was performed to evaluate the safety and efficacy of repeat treatment with the non-systemic antibiotic rifaximin.
Intervention:
- Those who initially responded to a 2 week course of open-label rifaximin 550 mg 3 times daily who then relapsed during an observation phase (up to 18 weeks) were randomly assigned to groups and given repeat treatments of rifaximin 550 mg or placebo, 3 times daily for 2 weeks.
Main Results:
- Of 1074 patients (44.1%) who responded to open-label rifaximin initially,
- 382 (35.6%) did not relapse,
- whereas 692 (64.4%) did;
- of these, 636 were randomly assigned to receive repeat treatment with
- rifaximin (n=328) or
- placebo (n=308).
- The percentage of responders was significantly greater with rifaximin than placebo (38.1% vs 31.5%).
- Adverse event rates were low and similar between groups.
- Main efficacy parameters were both abdominal pain and stool consistency.
Additional Results:
- N/A
Authors’ Conclusion:
- “In a phase 3 study of patients with relapsing symptoms of IBS-D, repeat rifaximin treatment was efficacious and well tolerated.”
Interesting Notes:
- “Rifaximin is an oral, minimally absorbed, broad-spectrum antimicrobial agent that targets the gastrointestinal tract and is associated with a low risk of clinically relevant bacterial antibiotic resistance.”
- 2 other trials (TARGET 1 and 2) showed a 9% improvement rate of Rifaximin compared with placebo.
- “Adverse events considered by investigators to be related to study drug were experienced by 6 (1.8%) and 8 (2.6%) patients in the rifaximin and placebo groups, respectively.”
- “Importantly, 35.6% of patients did not experience IBS-D symptom relapse for up to 18 weeks of follow-up after responding to the initial, open-label course of rifaximin.”
- R’s note: So 1/3 of patients will only need one course of Rifaximin and maintain their improvements with no preventative therapy.
Clinical Takeaways:
- 2/3 patients treated for IBS-D with Rifaximin may require an additional round of treatment within the first 18 weeks. Repeat treatment is safe and effective, but does not appear to work for all patients.
Dr. Ruscio’s Comments
A 6.5% better response than placebo is not fantastic, but it’s better than nothing. Big picture, this may underscore how a holistic or comprehensive treatment approach (diet, lifestyle, probiotics…) is better than a mono-therapeutic one (abx alone).
In my opinion, the overlooked clinical pearl here (outside of the need for a comprehensive treatment approach) is sometimes patients require more than one round of treatment in order to fully recover. This is OK and does not mean treatment was a failure, the patient was non-compliant, or that the patient ‘will never clear SIBO.’ This last point is especially important, as when some patients relapse, they become fearful and go to a very pessimistic place. I simply tell my patients, “Your microbiota may require a little more nudging with antimicrobials before it can return to a healthier equilibrium.”
Antibiotics carry a negative stigma, and rightfully so; however, not all antibiotics are equal. If a patient has not fully responded to other, less invasive therapies (diet, probiotics, etc…) and requires Abx, this study should be assuring that adverse events do not appear any more than those receiving placebo.
The Effect of Vitamin D on Thyroid Autoimmunity in Levothyroxine-Treated Women with Hashimoto’s Thyroiditis and Normal Vitamin D Status.
https://www.ncbi.nlm.nih.gov/pubmed/28073128
Study Purpose
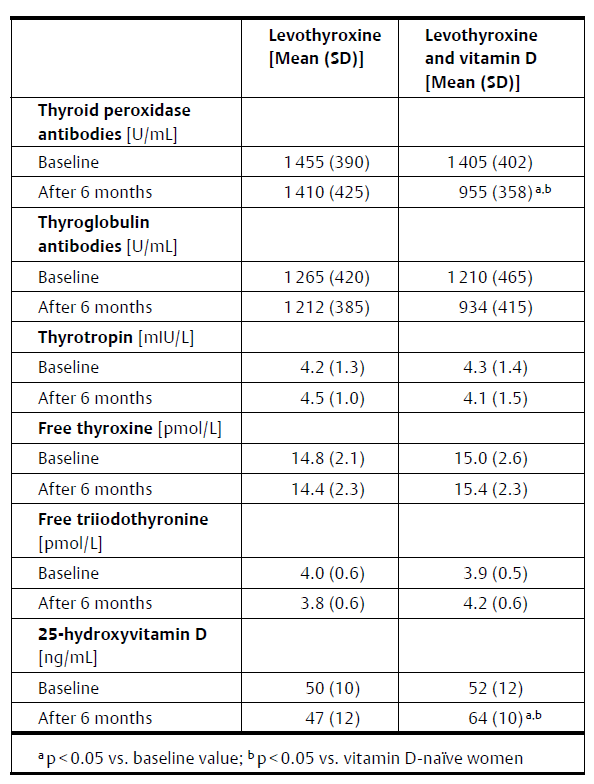
- To assess if vitamin D supplementation could improve thyroid autoimmunity in women already on levothyroxine.
Intervention:
- “The study included 34 women with Hashimoto’s thyroiditis and normal vitamin D status (serum 25-hydroxyvitamin D levels above 30 ng/mL) who had been treated for at least 6 months with levothyroxine.”
- “On the basis of patient preference, women were divided into 2 groups, receiving (n = 18) or not receiving (n = 16) oral vitamin D preparations (2000 IU daily).”
Main Results:
- Vitamin D supplementation increased vitamin D levels and reduced TPO and TG antibodies; the result was more pronounced for TPO.
Additional Results:
- At the start of the study, the lower one’s vitamin D level, the higher their antibodies tended to be. The more someone’s vitamin D levels changed, the more their thyroid antibodies tended to improve.
- Vitamin D did not affect TSH or free thyroid hormone levels.
- Those who were not on enough thyroid hormone (who had high TSH and normal T4 in spite of being on medication) had more benefit from vitamin D. TPO EFFECT: -42% compared to -20%
- “Women with markedly elevated antibody titers seem to be the best candidates for add-on vitamin D therapy.”
- TPO may be a better marker to monitor vitamin D’s effect on thyroid autoimmunity.
Authors’ Conclusion:
- “This finding indicates that exogenous vitamin D may reduce thyroid autoimmunity in women with Hashimoto’s thyroiditis and normal vitamin D status chronically treated with levothyroxine.”
Interesting Notes:
- Hashimoto’s has a prevalence of over 2% in women in the US.
- “In a recent meta-analysis, Wang et al. [9] found that patients with autoimmune thyroid disease had lower levels of 25-hydroxyvitamin D and were more likely to be deficient in 25-hydroxyvitamin D. Some [10, 11], but not all [12], studies have shown that polymorphisms of the vitamin D receptor may make patients more prone to the development of Hashimoto’s thyroiditis.”
- “Recently, we have found that levothyroxine increased 25-hydroxyvitamin D levels in women with postpartum thyroiditis [13], …, while no effect was observed in levothyroxine-treated women with non-autoimmune hypothyroidism [13].”
- Other studies have shown vitamin D can reduce thyroid autoimmunity [15].
- Other studies have shown that levothyroxine can decrease thyroid antibodies also [16–18].
Clinical Takeaways:
- Vitamin D supplementation may improve thyroid autoimmunity in those already on levothyroxine and in those with already normal vitamin D levels. Those with the lowest vitamin D and the highest levels of antibodies have the highest chance of success.
Dr. Ruscio’s Comments
We have much association data regarding vitamin D deficiency in various conditions, but many of the clinical/supplemental trials have been disappointing. This study is substantial because it helps fill a research void regarding vitamin D supplementation and thyroid autoimmunity.
Simply put, this study showed vitamin D can improve thyroid autoimmunity by 20-40%. What else is important to note is levothyroxine can increase vitamin D levels and levothyroxine can reduce thyroid antibodies. It’s important for natural-leaning providers to understand this. This might mean that for patients who start a gluten-free diet with their natural doctor shortly after starting levothyroxine with their endocrinologist, the decrease in thyroid autoimmunity that is later documented might not be solely coming from the diet. Hint: this means the patient might not need to adhere to dauntingly strict 100% gluten avoidance.
Additionally, since these women were already on levothyroxine for 6 months before starting vitamin D, the effect on thyroid autoimmunity from levothyroxine was likely minimized, thus giving us a good isolation for the effect of vitamin D.
Another noteworthy finding is these women already had at least somewhat normal levels of vitamin D (all were above 30), so the effect may not only be reserved to deficient populations.
Finally, those who were not on enough thyroid hormone (who had high TSH and normal T4 in spite of being on medication) had more benefit. How do we account for this? One theory suggests this is likely because inadequate suppression of TSH does not allow adequate gland suppression. When the gland is suppressed, it does not have to work to produce thyroid hormone and may then be better able to heal and repair, which may reduce a leaky gland-blood barrier. This then allows less antigens into the blood stream, which pours less gas on the autoimmune fire.
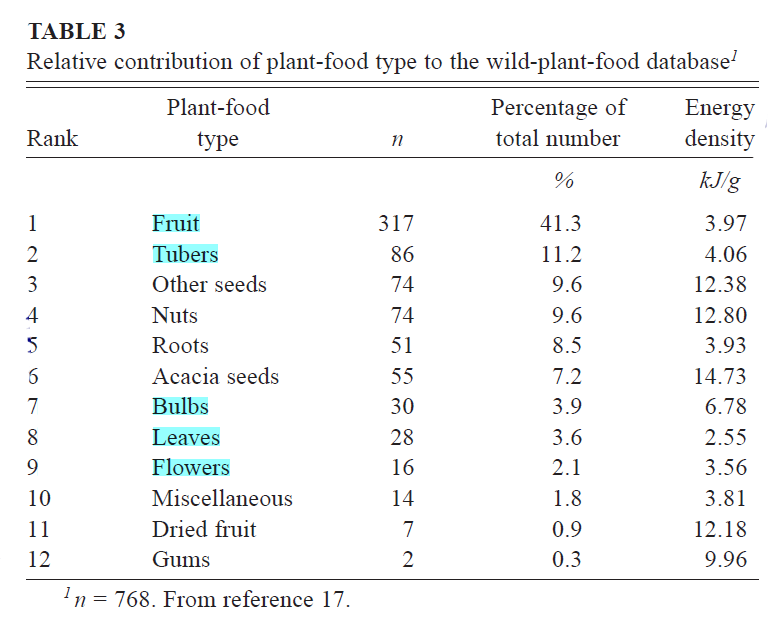
Plant-animal subsistence ratios and macronutrient energy estimations in worldwide hunter-gatherer diets.
https://www.ncbi.nlm.nih.gov/pubmed/10702160
Study Purpose
- To assess the diets of hunter-gatherer populations worldwide.
Intervention:
- “We analyzed the economic subsistence data for all 229 hunter-gatherer societies using all 3 subsistence categories (gathered plant foods, hunted animal foods, and fished animal foods) contained within the updated and revised version of the Ethnographic Atlas.”
Main Results:
- “Our analysis showed that whenever and wherever it was ecologically possible, hunter-gatherers consumed high amounts (45–65% of energy) of animal food.
- Most (73%) of the worldwide hunter-gatherer societies derived >50% (³56–65% of energy) of their subsistence from animal foods,
- whereas only 14% of these societies derived >50% (³56–65% of energy) of their subsistence from gathered plant foods.”
- “This high reliance on animal-based foods coupled with the relatively low carbohydrate content of wild plant foods produces universally characteristic macronutrient consumption ratios in which protein is elevated (19–35% of energy) at the expense of carbohydrates (22–40% of energy).”
- R’s note: this breaks down to roughly 110-200g of carbs per day for a 2,000 calorie diet.
- “The most plausible percentages of total energy would be 19–35% for dietary protein, 22–40% for carbohydrate, and 28–58% for fat.”
- “Our macronutrient projections for worldwide hunter-gatherer diets indicate that these diets would be extremely high in protein (19–35% of energy) and low in carbohydrate (22–40% of energy) by normal Western standards, whereas the fat intake would be comparable or higher (28–58% of energy) than values currently consumed in modern, industrialized societies.”
Additional Results:
- “When the subsistence dependencies of hunter-gatherers were analyzed by latitude … plant food markedly decreases with increasing latitude, primarily at a threshold value of >40° N or S. Because hunted land animal-food subsistence generally does not increase with increasing latitude, then the reduction in plant-food subsistence is replaced by increased subsistence on fished animal foods.”
- “For societies living at >40° N or S, there is an increasing latitudinal dependence on animal foods, which is primarily met by more fished animal foods.”
- “virtually all of the edible carcass was consumed.”
- “…virtually all of the potential fat contained in an animal’s carcass—except for that in the hooves, hide, and horn—would generally have been consumed by hunter-gatherers.”
- “No hunter-gatherer population is entirely or largely dependent (86–100% subsistence) on gathered plant foods, whereas 20% (n = 46) are highly or solely dependent (86–100%) on fished and hunted animal foods.”
- “Cereal grains represent the highest single food item consumed on the basis of energy content in both the United States (49) and the rest of the world (50); however, they were rarely consumed by most hunter-gatherers (37, 47), except as starvation foods or by hunter-gatherers living in arid and marginal environments.”
Authors’ Conclusion:
- “Whenever and wherever it was ecologically possible, hunter-gatherers would have consumed high amounts (45–65% of total energy) of animal food. Most (73%) hunter-gatherer societies worldwide derived > 50% (³56–65%) of their subsistence from animal foods, whereas only 13.5% of these societies derived more than half (³56–65%) of their subsistence from gathered plant foods. In turn, this high reliance on animal-based foods coupled with the relatively low carbohydrate content of wild
- plant foods produces universally characteristic macronutrient
- consumption ratios in which protein intakes are greater at the
- expense of carbohydrate.”
Interesting Notes:
- N/A
Clinical Takeaways:
- A paleo-type diet that is lower in carb and higher in protein and fat, relative to standard western diets, was what the majority of hunter-gatherers consumed, and may therefore be a healthier diet for modern day humans. Many studies have reinforced this; however, all diets devoid of processed foods and which focus on whole foods seem to provide health benefits when compared to western diets.
Dr. Ruscio’s Comments
Nothing shocking here wherein this study suggests a paleo-type is what was consumed by our ancestors. Something important to note is that the lower carb a society ate, usually due to increasing latitude, the more fish consumption appears in the diet. This might mean that it is important for those eating lower carb to ensure they get a few servings of fish in per week at minimum. Also, be sure not to make documented sources of high mercury fish like shark, whale, and swordfish. Note: tuna appears safe https://www.ncbi.nlm.nih.gov/pubmed/26463749.
Also interesting to note is that fruits, tubers, nuts, seeds, and roots were consumed more commonly than leafy vegetables. Not everyone tolerates tubers, nuts, etc.…, but this is interesting to note nonetheless.
I’d like to hear your thoughts or questions regarding any of the above information. Please leave comments or questions below – it might become our next practitioner question of the month.

Like what your reading?
Please share this with a colleague and help us improve functional medicine
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!