Patient Summary:
Current Health Rating: 75/100
- Overview Context:
- John is a 20 year old male with significant abdominal pain after eating, which has worsened over the past few months. He is in military school and is very limited with food choices.
- Symptoms and Concerns
- Chief Complaints:
- Lower abdominal pain after meals
- Gas
- Bloating
- Belching
- Mixed diarrhea and constipation
- Other Symptoms:
- Brain fog
- Acne
- Onset, Timeline and History:
- Didn’t have any symptoms until he joined military school
- Symptoms have gotten worse in the past few months without any obvious cause
Past Medical History
- Prior Diagnosis:
- IBS Mixed (2022)
- Medications:
- NA
Prior Testing and Treatment History
- Prior Testing Summary:
- NA
- Previous Diets:
- Helpful
- Dairy Free
- “I know dairy is definitely a culprit for my abdominal pain”
- Low FODMAP diet
- Fasting
- Dairy Free
- Non Responsive
- Gluten Free
- Helpful
- Previous Treatments:
- Helpful
- PRObiotics
- Digestive enzymes
- Hydrochloric acid
- Helpful
- Initial DDX:
- Gastrointestinal
- SIBO
- Dysbiosis
- Hypochlorhydria (+ response to HCl)
- GI pathogen
- Toxic
- Mold (Currently living in a dorm that was built in 1836, symptoms began after school)
- Gastrointestinal
- Initial Treatment Hierarchy:
- Step 1
- Elemental diet (2-4 day reset to hybrid)
- Triple probiotics
- GI Support Nutrients
- Continue current low FODMAP diet
- Testing: SIBO breath test, stool test
- Step 2:
- Herbal antimicrobials, expand diet, increase triple probiotics
- Step 3:
- Immunoglobulins, secretions (broad-spectrum enzymes +/- HCl)
- Step 4:
- Mold
- Step 1
- Recommended Testing
- SIBO breath testing
- Stool testing
- Initial Treatment Recommendations
- Diet:
- Continue a low FODMAP Paleo diet
- Treatment:
- Begin implementing Elemental Diet for 2-4 days; if symptoms improve, continue using Elemental Diet to replace 1-2 meals daily
- GI Supportive Nutrients
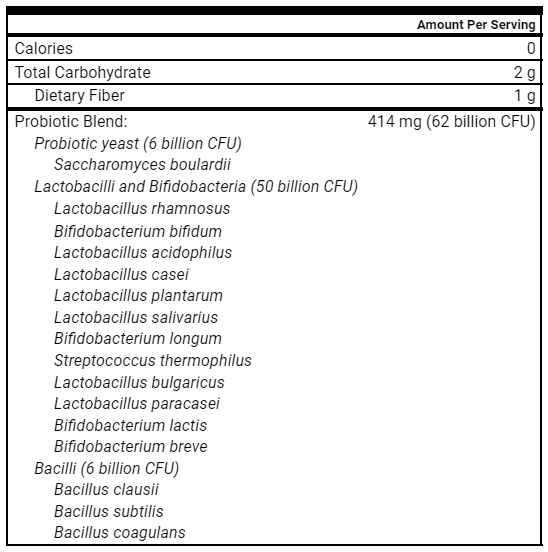
- Lactobacillus & Bifidobacterium probiotics, saccharomyces boulardii, and soil-based probiotics.
- Followup: 5 weeks
- Diet:
- Clinician Summary
- It’s important for context to know that we as a clinic have moved away from functional GI testing. This patient was seen prior to that shift. The initial testing was done to assess for SIBO and the significance of dysbiosis. As you’ll find out below, not only did these tests not change treatment, the results had the potential to lead us down the wrong path.
- Our primary focus will be on addressing suspected dysbiosis.
- I am considering mold as he is living in a very old dorm built in the 1800s.
- Subjective Assessment: 75/100, 0% better overall. Despite some symptoms improving, worse abdominal pain and brain fog make him feel overall no different than before.
- Current Symptoms:
- Improved:
- Diarrhea
- Constipation
- Acne
- Same:
- Loss of energy
- Worsened:
- Brain fog
- Stomach pain
- Improved:
- Treatment Response:
- Rifaximin (x2 week w/ local provider): Temporary improvement in abdominal pain and acne.
- Elemental Diet Reset: Reduced abdominal pain, but still had loose stools.
- Triple probiotics
- GI Support Nutrients: Unclear if beneficial.
- Paleo low FODMAP diet: Helpful, but too restrictive.
- Notes:
- Difficulty adhering to diet and avoiding known triggers such as dairy due to military communal dining.
- Current Symptoms:
- Lab Results
Aerodiagnostics Glucose SIBO breath test
- Negative
Doctor’s Data GI-360 Microbiome (dysbiosis)
- Dysbiosis index 1 (normal)
- Diversity score 4 (normal)
- Impression:
- Despite his stool and breath tests coming back normal, the next best step will be to pursue herbal antimicrobials. His positive response to Rifaximin is more informative for our next steps than the negative GI tests are.
- I am also concerned about him not eating enough food/electrolytes given how intense his military training is. This can lead to fatigue and brain fog. The next best step for him will be to work on expanding his diet, with a focus on increasing protein, carbohydrates, and electrolyte/salt intake.
- Updated DDX:
- Diet
- Nutrient deficiencies (hypocaloric, too low carb and protein)
- Gastrointestinal
SIBO(r/o 7/2022)- Dysbiosis (positive response to rifaximin, negative dysbiosis on stool testing)
- Hypochlorhydria (positive response to HCl)
- GI pathogen
- Toxic
- Mold (Currently living in a dorm that was built 1836, symptoms began after school)
- Diet
- Updated Treatment Hierarchy:
Step 1Elemental diet 2-4 reset to hybridTriple probioticsGI Support NutrientsContinue current low FODMAP dietTesting: SIBO breath test, Stool Test
- Step 2:
- Herbal antimicrobials, expand diet, increase carbohydrates and protein, double dose of triple probiotics.
- Step 3:
- Immunoglobulins, secretions (broad-spectrum enzymes +/- HCl)
- Step 4:
- Mold
- Updated Treatment Recommendations
- Diet
- Work on expanding diet while avoiding any problematic foods as best you can
- Increase carbohydrates and protein to support caloric and nutrient needs
- Increase salt/electrolytes
- Supplements
- Start
- Double dose of probiotics
- Herbal antimicrobials
- Continue
- GI Support Nutrients
- Start
- Followup: 6 weeks or sooner, if needed
- Diet
- Subjective Assessment: 76/100, 25% better overall. Loose stools are gone, constipation present but very mild. Abdominal pain is less frequent, but severity is the same when it happens.
- Current Symptoms:
- Improved:
- Stomach pain
- Loose stools
- Brain fog
- Same:
- Acne
- Worse:
- NA
- Improved:
- Treatment Response:
- Herbal antimicrobials (1 month): Stools normalizing, reduced frequency of brain fog and stomach pain.
- Current Symptoms:
- Impression:
- This patient noticed improvement in his most concerning symptom of abdominal pain. His positive response to Rifaximin and 1 month of herbal antimicrobials further emphasizes that dysbiosis is likely at the root cause of his symptoms, despite his normal stool and breath tests.
- Updated Treatment Recommendations
- New Treatment:
- Continue with second month of antimicrobials
- Double dose of probiotics
- Followup: 2 weeks after finishing second month of antimicrobials
- New Treatment:
Take Home Points
- Highlighted Clinical Rules
- Remember that lab tests only tell about 25% of the whole clinical picture. Good history taking, physical exam (when necessary), and assessment of prior treatment response supplies 75% of the information needed to make informed treatment decisions.
- Clinician Commentary
- This case study highlights the importance of treating the person and not the test. Despite a negative SIBO breath test and a normal dysbiosis score, this patient responded well to herbal antimicrobial therapy. While it’s possible that the type of stool test performed didn’t pick up on some pathogen, it still doesn’t take away from the main point that testing was not needed in this case. His symptoms are improving, and we didn’t need a test to guide treatment. Instead, the most important clue in this case was his positive, although temporary, response to Rifaximin. Understanding a patient’s previous response to treatment can be so important in helping them get well.
- In the clinic, we often find this phrase to be very helpful: “The treatment is often the test.” How a patient responds to a given treatment can be very insightful as to what is causing their symptoms. For example, a positive response to:
- A low FODMAP diet… can indicate dysbiosis
- Hiatal hernia technique… can indicate a hiatal hernia
- Getting out of your home for a week… may indicate mold or other environmental issues
- Mouth taping… may indicate sleep disordered breathing
- In this patient’s case, treatment with Rifaximin was more insightful than the $500 of GI testing that was performed. Testing has its place, but we’re finding more and more that functional GI testing often wastes money and doesn’t improve patient outcomes.
Study Details
Study Purpose
- Various dietary interventions have been used to treat eosinophilic esophagitis (EoE). This study aims to compare the efficacy of different interventions for inducing histologic remission in those with EoE.
Methods
- Meta-analysis of 33 studies, 1,317 patients with eosinophilic esophagitis
- 1,128 children
- 189 adults
- Patients were treated with one of the following:
- Elemental diet
- Allergy test-directed elimination diets
- 6-food elimination diets (SFED)
- 4-food elimination diets (FFED)
- Gluten free diet
- Dairy free diet
Results
- Elemental and 6-food elimination diets were the most effective at inducing histologic remission.
- “Elemental diets and SFEDs were the most effective, achieving <15 eosinophils/high-power field in 90.8% and 72.1% of patients, respectively.”
- Allergy test-directed elimination diets were the least effective for inducing histologic remission.
- “Overall efficacy was 45.5%. The 2 studies carried out on adult patients showed a significantly lower response rate of only 26.6% and 35%”
Authors’ Conclusions
- “Our results show that the various dietary treatment strategies are associated with varied efficacy rates, ranging from 90.8% for elemental diets to 45.5% for allergy testing–directed food elimination.”
- “Results from SFED showed a great deal of homogeneity (with I2 = 0%), which indicate that the results are widely generalizable. For elemental diet-based studies, the homogeneity was moderate (I2 = 52.3%). In contrast, results from studies assessing allergy testing–based food elimination proved highly heterogeneous (I2 = 75.1%), calling into question whether this treatment should be recommended to EoE patients.”
Interesting Notes
- While elemental dieting led to the greatest histologic remission, it’s important to note many of the studies had patients use it exclusively for 4-6 weeks, which is not practical for most patients. The 6-food elimination diet was also effective and likely much more practical.
- The results of this study enforce our observation that treating the person is more effective than treating the tests. In this case, empirical dietary treatments were more effective than lab-directed treatment.
- A recent 2022 systematic review on allergy-test-based elimination diets came to a similar conclusion. The authors stated “the efficacy of targeted elimination diets, guided by skin-prick test, specific IgE, and/or atopy patch tests does not appear superior to empirical ones.”
What Should I Do In Clinical Practice?
- Consider a short term elemental diet with or without an elimination diet for your patients with EoE. While the studies reviewed in the meta-analysis above used an elemental diet for long periods of time, we commonly find that 2-4 day “resets” dramatically reduce many GI symptoms.
Study Details
Study Purpose
- What effect does an individualized exercise program have on symptoms associated with post-COVID-19 condition, specifically fatigue and shortness of breath?
Methods
- 39 patients with post-COVID-19 symptoms, randomized to:
- Supervised Exercise Group
- Control Group (self-management exercise program from the World Health Organization)
- Supervised Exercise Group – 2 days of resistance training combined with moderate intensity aerobic training and 1 day of low intensity aerobic training
- Resistance training: 3 sets x 8 repetitions (50% of 1 rep max) of 4 exercises:
- Squat
- Bench press
- Deadlift
- Bench pull
- Moderate intensity aerobic training: 4 – 6 sets x 3 – 5 min at 70%–80% max heart rate, followed by 2–3 min at 55%–65% max heart rate
- Low intensity aerobic training (30-60 minutes at 65-70% max heart rate)
- Resistance training: 3 sets x 8 repetitions (50% of 1 rep max) of 4 exercises:
Results
- After 2 months of training, compared to the control group, the tailored exercise program led to greater improvements in:
- Number of patients with dyspnea (5.4% vs 83%)
- Physical activity quality of life (+41.5% vs +6.5%)
- Fatigue score (-50% vs -13.3%)
- Post-covid functional status score (-64% vs -29%) (lower is better)
- VO2max (+5.7% vs -0.8%)
- Depression scores (-53% vs -34%)
- Muscular strength (sit-to-stand and half-squat)
- 3 days of training per week led to clinically meaningful improvements in VO2max
- “The intervention group significantly improved their VO2max by a mean of 2.1 ml/kg/min−1. Increases >1 ml/kg/min−1 are usually considered clinically relevant in the population with cardiopulmonary disease and are related to “hard” clinical outcomes, such as mortality, readmissions, or quality of life.”
- NO patients dropped out in the intervention group
- “Thanks to the fact that all of them were treated individually, adjusting the intensity of intra-session training (always completing the pre-established volume), no patient dropped out due to tolerance issues.”
Authors’ Conclusions
- “As patients with a post-COVID condition may share some of the symptoms that occur in patients experiencing myalgic encephalomyelitis/chronic fatigue syndrome, management of post-exertional malaise and individualization should be one of the main goals of exercise programs in this population.”
- “Improvements in the quality of life, mood disorder symptoms, and cardiovascular and strength fitness suggest that exercise could have a main role in recovering active life when suffering long-term disability because of post-COVID-19 condition.”
Final Comments
- This study outlines a very simple and effective exercise routine that improved clinically meaningful outcomes in those with post-COVID-19 condition. As the authors suggested, post-COVID-19 syndrome has many similar symptoms to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). In fact, a proportion of patients with post-COVID-19 condition will fit the diagnostic criteria for ME/CFS [1]. Exercise has also been shown to improve fatigue in those with ME/CFS according to a 2019 meta analysis.
- Cardiorespiratory fitness (CRF) is one of the most important, modifiable indicators of long-term mortality. CRF is improved with many different forms of exercise, including weight training, HIIT, vigorous walking and aerobic training. A large retrospective study found that compared to those with the highest CRF, those with the lowest CRF had a 5x greater risk of all-cause mortality. The lowest level of CRF was a greater risk factor for all cause mortality than other common risk factors, including smoking, coronary artery disease and diabetes.
- We at the clinic are starting to prioritize exercise recommendations to our patients, especially for those with fatigue. As this study illustrates, a combination of moderate aerobic training, light aerobic training and resistance training for only 3 days per week is a helpful starting point.
Hormetic stressors are healthy types of stress, including exercise, sauna and cold exposure. Incorporating these into a routine can be very helpful. Prioritizing your own hormetic stressor routine will allow you to provide better care for your patients because you’ll think more clearly, have more energy, and be more resilient to stressors. A huge side-benefit is you’ll be able to speak from experience when helping patients with their own routines.
Here are the steps to ensure success with your routine:
- Step 1: Choose your routine
- Step 2: Create the time for it
- Step 3: Commit
Step 1: Choose your routine
Plan what your routine will look like and write it down somewhere you can easily reference. Start with a routine you can easily maintain, and then build from there. As an example, I am currently doing:
- 3 days per week of strength training (split between lower, upper and full body)
- 2 days per week of low intensity (zone 2) aerobic training
- 1-2 days per week of high intensity interval training
- Post-exercise sauna followed by cold exposure 5-6 days per week
- I could only do 2-3 days per week initially due to increased fatigue, but I can now tolerate almost daily sauna sessions.
Figure out how much time you’ll need to complete your routine so you can then move on to the next step.
Step 2: Create the time for it
You’re likely busy, which is why it’s important to create the time for exercise. When we don’t create the time, we’re less likely to follow through with our plans.
Figure out how much time you’ll need for your routine, pick a time that works for you and commit to it!
Step 3: Commit
There are many mornings I don’t want to get out of bed to do a hard workout. However, I have NEVER regretted it once I’m done! In fact, it’s on the mornings I miss my workout that I feel more tired.
In order to maintain your commitment, make the execution of the routine as easy as possible. This involves pre-planning and writing down your routine to take the guesswork out. Setting up everything you’ll need for your workout ahead of time can be helpful. .
Everything I set up the night before my workout includes:
- Workout clothes
- Water cup
- Pre-workout ingredients (creatine, citrulline, protein powder, electrolytes)
- Espresso machine is ready to go
Creating this routine into a habit can truly be a life changer. Choose a routine that works for you, and also one that challenges you. Let us know how this goes for you!
Best of luck in your implementation,
Dr. Scott