The Often Overlooked Gut-Thyroid Connection
Dr. Michael Ruscio is a DC, Naturopathic Practitioner, researcher, and clinician. He serves as an Adjunct Professor at the University of Bridgeport and has published numerous papers in scientific journals as well as the book Healthy Gut, Healthy You. He also founded the Ruscio Institute of Functional Health, where he helps patients with a wide range of GI conditions and serves as the Head of Research.Your thyroid symptoms could be coming from your gut.
- Gut-Thyroid Conditions are Linked|
- Thyroid Symptoms or Gut Symptoms?|
- Gut Treatments Improve Thyroid Health|
- Better Absorption of Thyroid Medication|
- Gut Health Tips for Thyroid Patient|
- Case Studies|
- Don’t Let This Happen to You|
If you’ve been diagnosed with a thyroid condition, like Hashimoto’s disease, you may assume that your symptoms of fatigue, brain fog, poor mood, and constipation are the result of poor thyroid function.
However, if you are taking thyroid medication and your TSH and free T4 levels are normal, it’s unlikely that you are experiencing thyroid symptoms. Poor gut health is a more likely cause. The connection between gut health and thyroid health is backed by a significant amount of research, yet it’s often overlooked in clinical practice.

Scientific evidence shows a strong connection between thyroid health and gut health. Based on current research, we know that:
- Thyroid conditions and gut conditions tend to occur together [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12]
- Fatigue, depression, anxiety, brain fog, and headache are common symptoms of gut conditions [4, 13, 14, 15, 16, 17, 18]
- Treating gut conditions can improve thyroid health [7, 8, 19, 20, 21, 22, 23, 24]
Good thyroid health starts in the gut. Simple, gut-directed therapies can help you to resolve frustrating symptoms, reduce thyroid inflammation, reduce thyroid antibodies, and, in some cases, reduce thyroid medication.
In this article we’ll explore the scientific facts behind the gut-thyroid connection and provide helpful tips to get you on the road to better gut and thyroid health.
Gut and Thyroid Conditions Are Linked
Even if you don’t have obvious gut symptoms, it’s important to know that gut conditions and thyroid conditions are very often found in the same patients. Here are some examples from the research:
| Celiac Disease and Non-Celiac Gluten Sensitivity | |
| Leaky Gut |
|
| Low Stomach Acid | |
| Small Intestinal Bacterial Overgrowth | |
| H. Pylori Infection |
While these studies only show association and not cause, collectively, they suggest an overall pattern of gut disturbances in thyroid patients.
Thyroid Symptoms or Gut Symptoms?
Symptoms like fatigue, brain fog, depression, and anxiety, and headaches aren’t unique to hypothyroidism. In fact, they are also symptoms of gut health conditions. Consider these research highlights:
|
Fatigue |
|
| Brain Fog | |
| Depression and Anxiety | |
| Headache |
This overlap between gut symptoms and thyroid symptoms leads to a common problem for thyroid patients. Once you get a thyroid diagnosis, healthcare practitioners tend to focus exclusively on thyroid treatments and stop considering other options. The result is that you end up chasing various thyroid solutions, without ever resolving your symptoms.
Thyroid medication can be very helpful for improving your thyroid hormone levels, however it doesn’t always lead to symptom resolution. As we see regularly in the clinic, healing your gut issues is the missing piece for many thyroid patients.
Research supports using a gut-focused approach to treating thyroid patients. Let’s take a closer look.
Gut Treatments Improve Thyroid Health
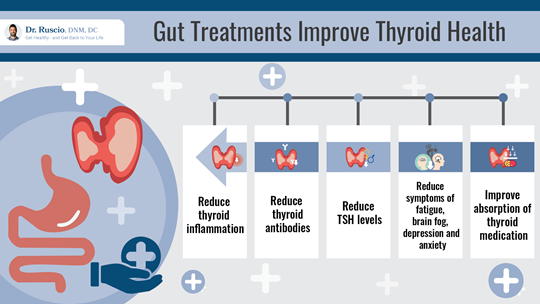
The research clearly shows that when you treat gut conditions, thyroid health also improves, sometimes dramatically. One small study found an astounding average drop in TPO antibodies of 2,029 when patients were treated for H. pylori gut infections [19]. Treating H. pylori has also been shown to improve TSH levels [7, 8, 20].
Treating Blastocystis hominis (a gut pathogen) has been shown to reduce inflammatory markers, thyroid antibodies, and TSH levels [21].
Identifying and removing food triggers can be helpful for some thyroid patients.
- One study found that lactose restriction led to significant decreases in TSH levels for thyroid patients with lactose intolerance [22].
- Another study found that a gluten-free diet improved the effects of thyroid medication for thyroid patients with atypical celiac disease [23].
Research also shows that gut treatments improve thyroid-like symptoms, including
All of this evidence suggests that if you have a thyroid diagnosis, it’s worth supporting your gut health as a means to reducing your symptoms and improving your thyroid health.
Gut Problems Are Two to Ten Times More Likely Than Thyroid Problems
Misdiagnosis of thyroid conditions is sadly common [29, 30]. For a surprising number of patients, an incorrect thyroid diagnosis creates a needless distraction that gets in the way of identifying the true problem and resolving symptoms. Research confirms what we frequently see in the clinic:
- Gut conditions are much more common than hypothyroidism [31, 32, 33].
- Gut conditions are frequently underdiagnosed [31, 34].
- Hypothyroidism is frequently over diagnosed [29, 30].
An estimated 10-15% of people in the USA have IBS, but only about half of these cases have been diagnosed [31]. In one survey of patients with GI complaints, 43.1% of subjects who met the Rome IV criteria for IBS had never been diagnosed [32]. Beyond IBS, research suggests that nearly 40% of adults worldwide have a functional gastrointestinal disorder [34].
Compared to 10-40% of people with IBS or functional gastrointestinal disorders, only 4.6% of the US population is hypothyroid [33]. One study showed up to 60% of patients may be taking thyroid hormone replacement unnecessarily [30].
A Healthier Gut = Better Absorption of Thyroid Medication
Another benefit of better gut health is that it may result in better absorption of thyroid medication.
Several studies found that gut infections, food sensitivities, low stomach acid, and other gut conditions can impair absorption of standard thyroid hormone medication [20, 22, 23, 35].
In one study, 21% of patients were able to reduce their thyroid medication dose after H. pylori treatment [8].
Probiotics are a great starting point for improving your gut health. In another study, thyroid patients who took probiotics were able to reduce their thyroid medication dosage [24].
Probiotics help with thyroid medication absorption because they improve the balance of microorganisms in your gut, reduce gut inflammation and help to heal the gut lining [36, 37, 38, 39, 40].
Gut Health Tips for Thyroid Patients
If you are taking thyroid medication and still have thyroid-like symptoms, improving your gut health may make a big difference. Improving gut health may also help those who have thyroid-like symptoms but test negative for a thyroid condition.
The best way to begin healing the gut is with a whole foods, anti-inflammatory diet and probiotic supplements. A paleo-like diet is a great anti-inflammatory diet template that works well for most thyroid patients.
Triple Probiotic Therapy is a therapeutic, multistrain approach that we developed in the clinic through years of trial and error with prescribing probiotics. It includes research-validated probiotic strains from all three major probiotic categories:
- Lactobacillus & bifidobacterium species
- Saccharomyces Boulardii (a probiotic fungus)
- Bacillus species (soil-based probiotics)
We know from research that multistrain probiotics are more effective than single strains [41, 42, 43]. We’ve also learned from patients that trying random probiotic products isn’t always helpful. For many patients who have tried probiotics in the past, Triple Probiotic Therapy achieves significantly better results.
We recommend starting your gut healing journey with a 3-4 week trial that combines an anti-inflammatory diet and Triple Probiotic Therapy. Any level of symptom improvement during this trial period is an indication that your gut health is improving. If you see improvement and are starting to feel better, continue with this approach.

For some patients, dietary improvements and probiotics will be all the treatment needed to completely eliminate thyroid-like symptoms. Other patients may need to take additional steps, such as:
- Taking HCL supplements for low stomach acid
- Taking digestive enzymes
- Taking nutrients to heal the intestinal lining
- Taking supplements like vitamin D and selenium.
- Diagnosis and treatment for gut infections such as SIBO, H. pylori, and Blastocystis hominis.
Our clinic can help you navigate more advanced steps of gut health treatment.
As your gut becomes healthier and your symptoms resolve, you may start to absorb thyroid medication better. Lab tests and a bit of fine tuning with your health provider can help to optimize your medication dose. The majority of patients do not need alternative thyroid medication, such as combined T4/T3 therapy.
Case Studies
My clinical experience parallels the research results I have shared in this article. Here are a couple of patient stories that show how treating the gut can resolve stubborn thyroid symptoms.
Amy was misdiagnosed with a thyroid condition and spent a year and a half trying to fix her thyroid.
Thyroid medication alone didn’t resolve Paige’s symptoms.
Don’t Let This Happen To You
Many thyroid patients suffer needlessly with unresolved symptoms, spending energy and money chasing thyroid treatments that don’t work. If you are struggling with stubborn “thyroid” symptoms, a change in focus can help.
Thyroid treatments will never fully work when the root cause of your symptoms is a gut imbalance. Simple interventions to improve gut health can lead to quick and effective symptom relief for thyroid patients. Start with an anti-inflammatory diet and a therapeutic probiotic protocol.
➕ References
- Kahaly GJ, Frommer L, Schuppan D. Celiac Disease and Glandular Autoimmunity. Nutrients. 2018 Jun 25;10(7):814. doi: 10.3390/nu10070814. PMID: 29941778; PMCID: PMC6073228.
- Roy A, Laszkowska M, Sundström J, Lebwohl B, Green PH, Kämpe O, Ludvigsson JF. Prevalence of Celiac Disease in Patients with Autoimmune Thyroid Disease: A Meta-Analysis. Thyroid. 2016 Jul;26(7):880-90. doi: 10.1089/thy.2016.0108. PMID: 27256300.
- Losurdo G, Piscitelli D, Giangaspero A, Principi M, Buffelli F, Giorgio F, Montenegro L, Sorrentino C, Amoruso A, Ierardi E, Di Leo A. Evolution of nonspecific duodenal lymphocytosis over 2 years of follow-up. World J Gastroenterol. 2015 Jun 28;21(24):7545-52. doi: 10.3748/wjg.v21.i24.7545. PMID: 26140001; PMCID: PMC4481450.
- Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014 May 23;12:85. doi: 10.1186/1741-7015-12-85. PMID: 24885375; PMCID: PMC4053283.
- Küçükemre Aydın B, Yıldız M, Akgün A, Topal N, Adal E, Önal H. Children with Hashimoto’s Thyroiditis Have Increased Intestinal Permeability: Results of a Pilot Study. J Clin Res Pediatr Endocrinol. 2020 Sep 2;12(3):303-307. doi: 10.4274/jcrpe.galenos.2020.2019.0186. Epub 2020 Jan 28. PMID: 31990165; PMCID: PMC7499128.
- Cellini M, Santaguida MG, Virili C, Capriello S, Brusca N, Gargano L, Centanni M. Hashimoto’s Thyroiditis and Autoimmune Gastritis. Front Endocrinol (Lausanne). 2017 Apr 26;8:92. doi: 10.3389/fendo.2017.00092. PMID: 28491051; PMCID: PMC5405068.
- Centanni M, Gargano L, Canettieri G, Viceconti N, Franchi A, Delle Fave G, Annibale B. Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006 Apr 27;354(17):1787-95. doi: 10.1056/NEJMoa043903. PMID: 16641395.
- Bugdaci MS, Zuhur SS, Sokmen M, Toksoy B, Bayraktar B, Altuntas Y. The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine. Helicobacter. 2011 Apr;16(2):124-30. doi: 10.1111/j.1523-5378.2011.00830.x. Erratum in: Helicobacter. 2011 Dec;16(6):482. Albayrak, Banu [corrected to Bayraktar, Banu]. PMID: 21435090.
- Konrad P, Chojnacki J, Kaczka A, Pawłowicz M, Rudnicki C, Chojnacki C. Ocena czynności tarczycy u osób z zespołem przerostu bakteryjnego jelita cienkiego [Thyroid dysfunction in patients with small intestinal bacterial overgrowth]. Pol Merkur Lekarski. 2018 Jan 23;44(259):15-18. Polish. PMID: 29374417.
- Brechmann T, Sperlbaum A, Schmiegel W. Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study. World J Gastroenterol. 2017 Feb 7;23(5):842-852. doi: 10.3748/wjg.v23.i5.842. PMID: 28223728; PMCID: PMC5296200.
- Choi YM, Kim TY, Kim EY, Jang EK, Jeon MJ, Kim WG, Shong YK, Kim WB. Association between thyroid autoimmunity and Helicobacter pylori infection. Korean J Intern Med. 2017 Mar;32(2):309-313. doi: 10.3904/kjim.2014.369. Epub 2017 Jan 16. PMID: 28092700; PMCID: PMC5339455.
- Shi WJ, Liu W, Zhou XY, Ye F, Zhang GX. Associations of Helicobacter pylori infection and cytotoxin-associated gene A status with autoimmune thyroid diseases: a meta-analysis. Thyroid. 2013 Oct;23(10):1294-300. doi: 10.1089/thy.2012.0630. Epub 2013 Sep 11. PMID: 23544831.
- Han CJ, Yang GS. Fatigue in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis of Pooled Frequency and Severity of Fatigue. Asian Nurs Res (Korean Soc Nurs Sci). 2016 Mar;10(1):1-10. doi: 10.1016/j.anr.2016.01.003. Epub 2016 Feb 1. PMID: 27021828.
- Maes M, Leunis JC. Normalization of leaky gut in chronic fatigue syndrome (CFS) is accompanied by a clinical improvement: effects of age, duration of illness and the translocation of LPS from gram-negative bacteria. Neuro Endocrinol Lett. 2008 Dec;29(6):902-10. PMID: 19112401.
- Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018 Jun 19;9(6):162. doi: 10.1038/s41424-018-0030-7. PMID: 29915215; PMCID: PMC6006167.
- van Langenberg DR, Yelland GW, Robinson SR, Gibson PR. Cognitive impairment in Crohn’s disease is associated with systemic inflammation, symptom burden and sleep disturbance. United European Gastroenterol J. 2017 Jun;5(4):579-587. doi: 10.1177/2050640616663397. Epub 2016 Aug 8. PMID: 28588890; PMCID: PMC5446137.
- Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019 Jul;50(2):132-143. doi: 10.1111/apt.15325. Epub 2019 Jun 3. PMID: 31157418.
- Li C, Yu S, Li H, Zhou J, Liu J, Tang W, Zhang L. Clinical features and risk factors for irritable bowel syndrome in Migraine patients. Pak J Med Sci. 2017 May-Jun;33(3):720-725. doi: 10.12669/pjms.333.12379. PMID: 28811802; PMCID: PMC5510134.
- Bertalot G, Montresor G, Tampieri M, Spasiano A, Pedroni M, Milanesi B, Favret M, Manca N, Negrini R. Decrease in thyroid autoantibodies after eradication of Helicobacter pylori infection. Clin Endocrinol (Oxf). 2004 Nov;61(5):650-2. doi: 10.1111/j.1365-2265.2004.02137.x. PMID: 15521972.
- Ribichini D, Fiorini G, Repaci A, Castelli V, Gatta L, Vaira D, Pasquali R. Tablet and oral liquid L-thyroxine formulation in the treatment of naïve hypothyroid patients with Helicobacter pylori infection. Endocrine. 2017 Sep;57(3):394-401. doi: 10.1007/s12020-016-1167-3. Epub 2016 Nov 15. PMID: 27848196.
- El-Zawawy HT, Farag HF, Tolba MM, Abdalsamea HA. Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17. Ther Adv Endocrinol Metab. 2020 Feb 21;11:2042018820907013. doi: 10.1177/2042018820907013. PMID: 32128107; PMCID: PMC7036484.
- Asik M, Gunes F, Binnetoglu E, Eroglu M, Bozkurt N, Sen H, Akbal E, Bakar C, Beyazit Y, Ukinc K. Decrease in TSH levels after lactose restriction in Hashimoto’s thyroiditis patients with lactose intolerance. Endocrine. 2014 Jun;46(2):279-84. doi: 10.1007/s12020-013-0065-1. PMID: 24078411.
- Virili C, Bassotti G, Santaguida MG, Iuorio R, Del Duca SC, Mercuri V, Picarelli A, Gargiulo P, Gargano L, Centanni M. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J Clin Endocrinol Metab. 2012 Mar;97(3):E419-22. doi: 10.1210/jc.2011-1851. Epub 2012 Jan 11. PMID: 22238404.
- Talebi S, Karimifar M, Heidari Z, Mohammadi H, Askari G. The effects of synbiotic supplementation on thyroid function and inflammation in hypothyroid patients: A randomized, double‑blind, placebo‑controlled trial. Complement Ther Med. 2020 Jan;48:102234. doi: 10.1016/j.ctim.2019.102234. Epub 2019 Nov 3. PMID: 31987229.
- Altobelli E, Del Negro V, Angeletti PM, Latella G. Low-FODMAP Diet Improves Irritable Bowel Syndrome Symptoms: A Meta-Analysis. Nutrients. 2017 Aug 26;9(9):940. doi: 10.3390/nu9090940. PMID: 28846594; PMCID: PMC5622700.
- Marum AP, Moreira C, Saraiva F, Tomas-Carus P, Sousa-Guerreiro C. A low fermentable oligo-di-mono saccharides and polyols (FODMAP) diet reduced pain and improved daily life in fibromyalgia patients. Scand J Pain. 2016 Oct;13:166-172. doi: 10.1016/j.sjpain.2016.07.004. Epub 2016 Aug 22. PMID: 28850525.
- Ng QX, Peters C, Ho CYX, Lim DY, Yeo WS. A meta-analysis of the use of probiotics to alleviate depressive symptoms. J Affect Disord. 2018 Mar 1;228:13-19. doi: 10.1016/j.jad.2017.11.063. Epub 2017 Nov 16. PMID: 29197739.
-
Effects of regulating intestinal microbiota on anxiety symptoms: A systematic review
- Nancy A. Melville. Mild Hypothyroidism Being Overtreated, Avoid Pills, Says Panel. Medscape Medical News. 2019.
- Livadas S, Bothou C, Androulakis I, Boniakos A, Angelopoulos N, Duntas L. Levothyroxine Replacement Therapy and Overuse: A Timely Diagnostic Approach. Thyroid. 2018 Nov 30. doi: 10.1089/thy.2018.0014. Epub ahead of print. PMID: 30351232.
- https://gi.org/topics/irritable-bowel-syndrome/
- Am J Gastroenterol. IBS is underdiagnosed and undertreated in the US. Clinical Essentials, Univadis from Medscape. 2017.
- https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism
- Kenny Walter. Nearly 40% of Adults Suffer From a Functional Gastrointestinal Disorder. HCP Live. 2020.
- Castellana M, Castellana C, Giovanella L, Trimboli P. Prevalence of gastrointestinal disorders having an impact on tablet levothyroxine absorption: should this formulation still be considered as the first-line therapy? Endocrine. 2020 Feb;67(2):281-290. doi: 10.1007/s12020-019-02185-4. Epub 2020 Jan 17. PMID: 31953721.
- Leblhuber F, Steiner K, Schuetz B, Fuchs D, Gostner JM. Probiotic Supplementation in Patients with Alzheimer’s Dementia – An Explorative Intervention Study. Curr Alzheimer Res. 2018;15(12):1106-1113. doi: 10.2174/1389200219666180813144834. PMID: 30101706; PMCID: PMC6340155.
- Toribio-Mateas M. Harnessing the Power of Microbiome Assessment Tools as Part of Neuroprotective Nutrition and Lifestyle Medicine Interventions. Microorganisms. 2018 Apr 25;6(2):35. doi: 10.3390/microorganisms6020035. PMID: 29693607; PMCID: PMC6027349.
- Mujagic Z, de Vos P, Boekschoten MV, Govers C, Pieters HH, de Wit NJ, Bron PA, Masclee AA, Troost FJ. The effects of Lactobacillus plantarum on small intestinal barrier function and mucosal gene transcription; a randomized double-blind placebo controlled trial. Sci Rep. 2017 Jan 3;7:40128. doi: 10.1038/srep40128. PMID: 28045137; PMCID: PMC5206730.
- Sindhu KN, Sowmyanarayanan TV, Paul A, Babji S, Ajjampur SS, Priyadarshini S, Sarkar R, Balasubramanian KA, Wanke CA, Ward HD, Kang G. Immune response and intestinal permeability in children with acute gastroenteritis treated with Lactobacillus rhamnosus GG: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2014 Apr;58(8):1107-15. doi: 10.1093/cid/ciu065. Epub 2014 Feb 5. PMID: 24501384; PMCID: PMC3967829.
- Lamprecht M, Bogner S, Schippinger G, Steinbauer K, Fankhauser F, Hallstroem S, Schuetz B, Greilberger JF. Probiotic supplementation affects markers of intestinal barrier, oxidation, and inflammation in trained men; a randomized, double-blinded, placebo-controlled trial. J Int Soc Sports Nutr. 2012 Sep 20;9(1):45. doi: 10.1186/1550-2783-9-45. PMID: 22992437; PMCID: PMC3465223.
- American College of Gastroenterology Task Force on Irritable Bowel Syndrome, Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009 Jan;104 Suppl 1:S1-35. doi: 10.1038/ajg.2008.122. PMID: 19521341.
- Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014 Oct;109(10):1547-61; quiz 1546, 1562. doi: 10.1038/ajg.2014.202. Epub 2014 Jul 29. PMID: 25070051.
- Zhang C, Jiang J, Tian F, Zhao J, Zhang H, Zhai Q, Chen W. Meta-analysis of randomized controlled trials of the effects of probiotics on functional constipation in adults. Clin Nutr. 2020 Oct;39(10):2960-2969. doi: 10.1016/j.clnu.2020.01.005. Epub 2020 Jan 14. PMID: 32005532.
➕ Links & Resources
More on the Thyroid:
- What Does Your Thyroid Do?
- What are Optimal Thyroid Levels?
- Do You Need a Thyroid Detox?
- What Causes Thyroiditis?
- A Low-Iodine Diet May Improve Hypothyroidism
- When Should I Worry About My Thyroid Nodule?
- What Causes Thyroid Nodules to Grow?
- How Long Can You Go Without Thyroid Medication?
- How Should I Use Thyroid Supplements?
- What Does Pain in the Thyroid Mean?
- What are Healthy Levels for Thyroid Antibodies?
- Find Your Ideal Thyroid Medication in 4 Simple Steps
Discussion
I care about answering your questions and sharing my knowledge with you. Leave a comment or connect with me on social media asking any health question you may have and I just might incorporate it into our next listener questions podcast episode just for you!